Dabigatran: Difference between revisions
No edit summary |
Gerald Chi (talk | contribs) mNo edit summary |
||
| Line 5: | Line 5: | ||
* [[Pradaxa|Pradaxa]] | * [[Pradaxa|Pradaxa]] | ||
==Disclaimer== | |||
'''''WikiDoc Drug Project is a constellation of drug information for healthcare providers and patients vigorously vetted on the basis of FDA package insert, MedlinePlus, Practice Guidelines, Scientific Statements, and scholarly medical literature. The information provided is not a medical advice or treatment. WikiDoc does not promote any medication or off-label use of drugs. Please read our full disclaimer [[wikidoc:General_disclaimer|{{fontcolor|#FF0000|here}}]].''''' | |||
==<span style="color:#FF0000; background:#000000;">Black Box Warning</span>== | |||
{| style="border: 3px solid #696969;" | |||
| style="background: #000000; border: 0px; padding: 20px 20px; width: 800px;" | | |||
<center> | |||
<font color="#F8F8FF" style="font-weight: bold;">WARNING: DISCONTINUING PRADAXA IN PATIENTS WITHOUT ADEQUATE CONTINUOUS ANTICOAGULATION INCREASES RISK OF STROKE</font> | |||
</center> | |||
<center> | |||
<font color="#F8F8FF" size="1" style="font-style: italic;">See full prescribing information for complete boxed warning.</font> | |||
</center> | |||
<font color="#F8F8FF" style="font-weight: bold;"> | |||
Discontinuing PRADAXA places patients at an increased risk of thrombotic events. If anticoagulation with PRADAXA must be discontinued for a reason other than pathological bleeding, consider coverage with another anticoagulant.</font> | |||
|} | |||
==Overview== | ==Overview== | ||
{{PAGENAME}} is an [[anti-coagulant]], [[direct thrombin inhibitor]] drug that is FDA approved for the prophylaxis of [[stroke]] and systemic [[embolism]] in patients with non-valvular [[atrial fibrillation]]. There is a Black Box Warning for this drug as shown <span style="background:#000000;">'''[[{{PAGENAME}}#Black Box Warning|{{fontcolor|#FF0000|here}}]]'''</span>. Common adverse reactions include [[bleeding]], [[esophagitis]], [[gastritis]], [[gastroesophageal reflux disease]], [[gastrointestinal hemorrhage]], [[gastrointestinal ulcer]], and [[indigestion]]. | |||
==Adult Indications and Dosage== | |||
===FDA-Labeled Indications and Dosage (Adult)=== | |||
=====Condition 1===== | |||
* Dosing Information | |||
:: (Dosage) | |||
|contraindications=*Active pathological bleeding [see Warnings and Precautions (5.2) and Adverse Reactions (6.1)]. | |||
*History of a serious hypersensitivity reaction to PRADAXA (e.g., anaphylactic reaction or anaphylactic shock) [see Adverse Reactions (6.1)]. | |||
*Mechanical prosthetic heart valve [see Warnings and Precautions (5.3)] | |||
|warnings====Increased Risk of Stroke with Discontinuation of PRADAXA=== | |||
Discontinuing PRADAXA in absence of adequate alternative anticoagulation increases the risk of thrombotic events. If PRADAXA must be discontinued for a reason other than pathological bleeding, consider coverage with another anticoagulant [see Dosage and Administration (2.6)]. | |||
===Risk of Bleeding=== | |||
PRADAXA increases the risk of bleeding and can cause significant and, sometimes, fatal bleeding. Promptly evaluate any signs or symptoms of blood loss (e.g., a drop in hemoglobin and/or hematocrit or hypotension). Discontinue PRADAXA in patients with active pathological bleeding [see Dosage and Administration (2.2)]. | |||
Risk factors for bleeding include the concomitant use of other drugs that increase the risk of bleeding (e.g., anti-platelet agents, heparin, fibrinolytic therapy, and chronic use of NSAIDs). PRADAXA’s anticoagulant activity and half-life are increased in patients with renal impairment [see Clinical Pharmacology (12.2)]. | |||
A specific reversal agent for dabigatran is not available. [[Hemodialysis]] can remove dabigatran; however the clinical experience supporting the use of hemodialysis as a treatment for bleeding is limited [see Overdosage (10)]. Activated prothrombin complex concentrates (aPCCs, e.g., FEIBA), or recombinant Factor VIIa, or concentrates of coagulation factors II, IX or X may be considered but their use has not been evaluated in clinical trials. Protamine sulfate and vitamin K are not expected to affect the anticoagulant activity of dabigatran. Consider administration of platelet concentrates in cases where thrombocytopenia is present or long-acting antiplatelet drugs have been used. | |||
===Thromboembolic and Bleeding Events in Patients with Prosthetic Heart Valves=== | |||
The safety and efficacy of PRADAXA in patients with bileaflet mechanical prosthetic heart valves was evaluated in the RE-ALIGN trial, in which patients with bileaflet mechanical prosthetic heart valves (recently implanted or implanted more than three months prior to enrollment) were randomized to dose adjusted warfarin or 150, 220, or 300 mg of PRADAXA twice a day. RE-ALIGN was terminated early due to the occurrence of significantly more thromboembolic events (valve thrombosis, stroke, [[transient ischemic attack]], and [[myocardial infarction]]) and an excess of major bleeding (predominantly post-operative pericardial effusions requiring intervention for hemodynamic compromise) in the PRADAXA treatment arm as compared to the [[warfarin]] treatment arm. These bleeding and thromboembolic events were seen both in patients who were initiated on PRADAXA post-operatively within three days of mechanical bileaflet valve implantation, as well as in patients whose valves had been implanted more than three months prior to enrollment. Therefore, the use of PRADAXA is contraindicated in patients with mechanical prosthetic valves [see Contraindications (4)]. | |||
The use of PRADAXA for the prophylaxis of thromboembolic events in patients with atrial fibrillation in the setting of other forms of valvular heart disease, including the presence of a bioprosthetic heart valve, has not been studied and is not recommended. | |||
===Effect of P-gp Inducers and Inhibitors on Dabigatran Exposure=== | |||
The concomitant use of PRADAXA with P-gp inducers (e.g. rifampin) reduces exposure to dabigatran and should generally be avoided [see Clinical Pharmacology(12.3)]. | |||
P-gp inhibition and impaired renal function are the major independent factors that result in increased exposure to dabigatran [see Clinical Pharmacology (12.3)]. Concomitant use of P-gp inhibitors in patients with renal impairment is expected to produce increased exposure of dabigatran compared to that seen with either factor alone. | |||
Consider reducing the dose of PRADAXA to 75 mg twice daily when [[dronedarone]] or systemic [[ketoconazole]] is coadministered with PRADAXA in patients with moderate renal impairment (CrCl 30-50 mL/min). Avoid use of PRADAXA and P-gp inhibitors in patients with severe renal impairment (CrCl 15-30 mL/min) [see Drug Interactions (7) and Use in Specific Populations (8.6)]. | |||
|clinicalTrials=Because clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. | |||
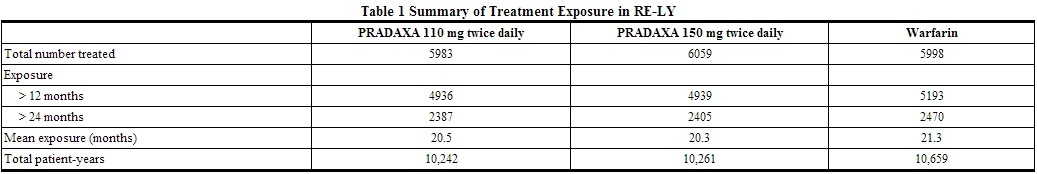
The RE-LY (Randomized Evaluation of Long-term Anticoagulant Therapy) study provided safety information on the use of two doses of PRADAXA and warfarin [see Clinical Studies (14)]. The numbers of patients and their exposures are described in Table 1. Limited information is presented on the 110 mg dosing arm because this dose is not approved. | |||
{| | |||
|- | |||
|[[File:Dabigatran02.jpg|thumb|800px|left]] | |||
|- | |||
|} | |||
====Drug Discontinuation in RE-LY==== | |||
The rates of adverse reactions leading to treatment discontinuation were 21% for PRADAXA 150 mg and 16% for warfarin. The most frequent adverse reactions leading to discontinuation of PRADAXA were bleeding and gastrointestinal events (i.e., dyspepsia, nausea, upper abdominal pain, gastrointestinal hemorrhage, and diarrhea). | |||
====Bleeding [see Warnings and Precautions (5.2)]==== | |||
Table 2 shows the number of patients experiencing serious bleeding during the treatment period in the RE-LY study, with the bleeding rate per 800 patient-years (%). Major bleeds fulfilled one or more of the following criteria: bleeding associated with a reduction in hemoglobin of at least 2 grams per deciliter or leading to a transfusion of at least 2 units of blood, or symptomatic bleeding in a critical area or organ (intraocular, intracranial, intraspinal or intramuscular with compartment syndrome, retroperitoneal bleeding, intra-articular bleeding, or pericardial bleeding). A life-threatening bleed met one or more of the following criteria: fatal, symptomatic intracranial bleed, reduction in hemoglobin of at least 5 grams per deciliter, transfusion of at least 4 units of blood, associated with hypotension requiring the use of intravenous inotropic agents, or necessitating surgical intervention. Intracranial hemorrhage included intracerebral (hemorrhagic stroke), subarachnoid, and subdural bleeds. | |||
{| | |||
|- | |||
|[[File:Dabigatran03.jpg|thumb|800px|left]] | |||
|- | |||
|} | |||
The risk of major bleeds was similar with PRADAXA 150 mg and warfarin across major subgroups defined by baseline characteristics, with the exception of age, where there was a trend towards a higher incidence of major bleeding on PRADAXA (hazard ratio 1.2, 95% CI: 1.0 to 1.4) for patients ≥75 years of age. | |||
There was a higher rate of major gastrointestinal bleeds in patients receiving PRADAXA 150 mg than in patients receiving warfarin (1.6% vs. 1.1%, respectively, with a hazard ratio vs. warfarin of 1.5, 95% CI, 1.2 to 1.9), and a higher rate of any gastrointestinal bleeds (6.1% vs. 4.0%, respectively). | |||
====Gastrointestinal Adverse Reactions==== | |||
Patients on PRADAXA 150 mg had an increased incidence of gastrointestinal adverse reactions (35% vs. 24% on warfarin). These were commonly dyspepsia (including abdominal pain upper, abdominal pain, abdominal discomfort, and epigastric discomfort) and gastritis-like symptoms (including GERD, esophagitis, erosive gastritis, gastric hemorrhage, hemorrhagic gastritis, hemorrhagic erosive gastritis, and gastrointestinal ulcer). | |||
====Hypersensitivity Reactions==== | |||
In the RE-LY study, drug hypersensitivity (including urticaria, rash, and pruritus), allergic edema, anaphylactic reaction, and anaphylactic shock were reported in <0.1% of patients receiving PRADAXA. | |||
|postmarketing=The following adverse reactions have been identified during post approval use of PRADAXA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The following adverse reactions have been identified during post approval use of PRADAXA: angioedema, thrombocytopenia, esophageal ulcer. | |||
|drugInteractions=The concomitant use of PRADAXA with [P-gp inducers] (e.g., [[rifampin]]) reduces exposure to dabigatran and should generally be avoided [see Clinical Pharmacology(12.3)]. | |||
P-gp inhibition and impaired renal function are the major independent factors that result in increased exposure to dabigatran [see Clinical Pharmacology (12.3)]. Concomitant use of P-gp inhibitors in patients with renal impairment is expected to produce increased exposure of dabigatran compared to that seen with either factor alone. | |||
In patients with moderate renal impairment (CrCl 30-50 mL/min), consider reducing the dose of PRADAXA to 75 mg twice daily when administered concomitantly with the P-gp inhibitor dronedarone or systemic ketoconazole. The use of P-gp inhibitors (verapamil, amiodarone, quinidine, and clarithromycin) does not require a dose adjustment of PRADAXA. These results should not be extrapolated to other P-gp inhibitors [see Warnings and Precautions (5.4), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)]. | |||
The concomitant use of PRADAXA and P-gp inhibitors in patients with severe renal impairment (CrCl 15-30 mL/min) should be avoided [see Warnings and Precautions(5.4), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)]. | |||
|useInPregnancyFDA=Pregnancy Category C | |||
There are no adequate and well-controlled studies in pregnant women. | |||
Dabigatran has been shown to decrease the number of implantations when male and female rats were treated at a dosage of 70 mg/kg (about 2.6 to 3.0 times the human exposure at maximum recommended human dose [MRHD] of 300 mg/day based on area under the curve [AUC] comparisons) prior to mating and up to implantation (gestation Day 6). Treatment of pregnant rats after implantation with dabigatran at the same dose increased the number of dead offspring and caused excess vaginal/uterine bleeding close to parturition. Although dabigatran increased the incidence of delayed or irregular ossification of fetal skull bones and vertebrae in the rat, it did not induce major malformations in rats or rabbits. | |||
|useInLaborDelivery=Safety and effectiveness of PRADAXA during labor and delivery have not been studied in clinical trials. Consider the risks of bleeding and of stroke in using PRADAXA in this setting [see Warnings and Precautions (5.2)]. | |||
Death of offspring and mother rats during labor in association with uterine bleeding occurred during treatment of pregnant rats from implantation (gestation Day 7) to weaning (lactation Day 21) with dabigatran at a dose of 70 mg/kg (about 2.6 times the human exposure at MRHD of 300 mg/day based on AUC comparisons). | |||
|useInNursing=It is not known whether dabigatran is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when PRADAXA is administered to a nursing woman. | |||
|useInPed=Safety and effectiveness of PRADAXA in pediatric patients have not been established. | |||
|useInGeri=Of the total number of patients in the RE-LY study, 82% were 65 and over, while 40% were 75 and over. The risk of stroke and bleeding increases with age, but the risk-benefit profile is favorable in all age groups [see Warnings and Precautions (5), Adverse Reactions (6.1), and Clinical Studies (14)]. | |||
|useInRenalImpair=No dose adjustment of PRADAXA is recommended in patients with mild or moderate renal impairment [see Clinical Pharmacology (12.3)]. Reduce the dose of PRADAXA in patients with severe renal impairment (CrCl 15-30 mL/min) [see Dosage and Administration (2.1, 2.2) and Clinical Pharmacology (12.3)]. Dosing recommendations for patients with CrCl <15 mL/min or on dialysis cannot be provided. | |||
Adjust dose appropriately in patients with renal impairment receiving concomitant P-gp inhibitors [see Warnings and Precautions (5.4), Drug Interactions (7), and Clinical Pharmacology (12.3)]. | |||
|administration=Route: Oral | |||
===Instructions to Patients=== | |||
Instruct patients to swallow the capsules whole. PRADAXA should be taken with a full glass of water. Breaking, chewing, or emptying the contents of the capsule can result in increased exposure [see Clinical Pharmacology (12.3)]. | |||
If a dose of PRADAXA is not taken at the scheduled time, the dose should be taken as soon as possible on the same day; the missed dose should be skipped if it cannot be taken at least 6 hours before the next scheduled dose. The dose of PRADAXA should not be doubled to make up for a missed dose. | |||
===Converting from or to Warfarin=== | |||
When converting patients from warfarin therapy to PRADAXA, discontinue warfarin and start PRADAXA when the INR is below 2.0. | |||
When converting from PRADAXA to warfarin, adjust the starting time of warfarin based on creatinine clearance as follows: | |||
For CrCl ≥50 mL/min, start warfarin 3 days before discontinuing PRADAXA. | |||
For CrCl 30-50 mL/min, start warfarin 2 days before discontinuing PRADAXA. | |||
For CrCl 15-30 mL/min, start warfarin 1 day before discontinuing PRADAXA. | |||
For CrCl <15 mL/min, no recommendations can be made. | |||
Because PRADAXA can increase INR, the INR will better reflect warfarin’s effect only after PRADAXA has been stopped for at least 2 days [see Clinical Pharmacology (12.2)]. | |||
===Converting from or to Parenteral Anticoagulants=== | |||
For patients currently receiving a parenteral anticoagulant, start PRADAXA 0 to 2 hours before the time that the next dose of the parenteral drug was to have been administered or at the time of discontinuation of a continuously administered parenteral drug (e.g., intravenous unfractionated heparin). | |||
For patients currently taking PRADAXA, wait 12 hours (CrCl ≥30 mL/min) or 24 hours (CrCl <30 mL/min) after the last dose of PRADAXA before initiating treatment with a parenteral anticoagulant [see Clinical Pharmacology (12.3)]. | |||
== | ===Surgery and Interventions=== | ||
If possible, discontinue PRADAXA 1 to 2 days (CrCl ≥50 mL/min) or 3 to 5 days (CrCl <50 mL/min) before invasive or surgical procedures because of the increased risk of bleeding. Consider longer times for patients undergoing major surgery, spinal puncture, or placement of a spinal or epidural catheter or port, in whom complete hemostasis may be required [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)]. | |||
If surgery cannot be delayed, there is an increased risk of bleeding [see Warnings and Precautions (5.2)]. This risk of bleeding should be weighed against the urgency of intervention [see Warnings and Precautions (5.1)]. | |||
|monitoring=INR is relatively insensitive to the exposure to dabigatran and cannot be interpreted the same way as used for warfarin monitoring. | |||
|IVCompat=FDA Package Insert for Metoprolol tartrate contains no information regarding Black Box Warning. | |||
|overdose=Accidental overdose may lead to hemorrhagic complications. There is no reversal agent for dabigatran. In the event of hemorrhagic complications, initiate appropriate clinical support, discontinue treatment with PRADAXA, and investigate the source of bleeding. Dabigatran is primarily eliminated by the kidneys with a low plasma protein binding of approximately 35%. Hemodialysis can remove dabigatran; however, data supporting this approach are limited. Using a high-flux dialyzer, blood flow rate of 200 mL/min, and dialysate flow rate of 700 mL/min, approximately 49% of total dabigatran can be cleared from plasma over 4 hours. At the same dialysate flow rate, approximately 57% can be cleared using a dialyzer blood flow rate of 300 mL/min, with no appreciable increase in clearance observed at higher blood flow rates. Upon cessation of hemodialysis, a redistribution effect of approximately 7% to 15% is seen. The effect of dialysis on dabigatran’s plasma concentration would be expected to vary based on patient specific characteristics. Measurement of aPTT or ECT may help guide therapy. | |||
}} | |||
{{Antithrombotics}} | {{Antithrombotics}} | ||
Revision as of 16:02, 28 March 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]
Dabigatran Etexilate Mesylate
Disclaimer
WikiDoc Drug Project is a constellation of drug information for healthcare providers and patients vigorously vetted on the basis of FDA package insert, MedlinePlus, Practice Guidelines, Scientific Statements, and scholarly medical literature. The information provided is not a medical advice or treatment. WikiDoc does not promote any medication or off-label use of drugs. Please read our full disclaimer here.
Black Box Warning
|
WARNING: DISCONTINUING PRADAXA IN PATIENTS WITHOUT ADEQUATE CONTINUOUS ANTICOAGULATION INCREASES RISK OF STROKE See full prescribing information for complete boxed warning. Discontinuing PRADAXA places patients at an increased risk of thrombotic events. If anticoagulation with PRADAXA must be discontinued for a reason other than pathological bleeding, consider coverage with another anticoagulant. |
Overview
Dabigatran is an anti-coagulant, direct thrombin inhibitor drug that is FDA approved for the prophylaxis of stroke and systemic embolism in patients with non-valvular atrial fibrillation. There is a Black Box Warning for this drug as shown here. Common adverse reactions include bleeding, esophagitis, gastritis, gastroesophageal reflux disease, gastrointestinal hemorrhage, gastrointestinal ulcer, and indigestion.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Condition 1
- Dosing Information
- (Dosage)
|contraindications=*Active pathological bleeding [see Warnings and Precautions (5.2) and Adverse Reactions (6.1)].
- History of a serious hypersensitivity reaction to PRADAXA (e.g., anaphylactic reaction or anaphylactic shock) [see Adverse Reactions (6.1)].
- Mechanical prosthetic heart valve [see Warnings and Precautions (5.3)]
|warnings====Increased Risk of Stroke with Discontinuation of PRADAXA===
Discontinuing PRADAXA in absence of adequate alternative anticoagulation increases the risk of thrombotic events. If PRADAXA must be discontinued for a reason other than pathological bleeding, consider coverage with another anticoagulant [see Dosage and Administration (2.6)].
Risk of Bleeding
PRADAXA increases the risk of bleeding and can cause significant and, sometimes, fatal bleeding. Promptly evaluate any signs or symptoms of blood loss (e.g., a drop in hemoglobin and/or hematocrit or hypotension). Discontinue PRADAXA in patients with active pathological bleeding [see Dosage and Administration (2.2)].
Risk factors for bleeding include the concomitant use of other drugs that increase the risk of bleeding (e.g., anti-platelet agents, heparin, fibrinolytic therapy, and chronic use of NSAIDs). PRADAXA’s anticoagulant activity and half-life are increased in patients with renal impairment [see Clinical Pharmacology (12.2)].
A specific reversal agent for dabigatran is not available. Hemodialysis can remove dabigatran; however the clinical experience supporting the use of hemodialysis as a treatment for bleeding is limited [see Overdosage (10)]. Activated prothrombin complex concentrates (aPCCs, e.g., FEIBA), or recombinant Factor VIIa, or concentrates of coagulation factors II, IX or X may be considered but their use has not been evaluated in clinical trials. Protamine sulfate and vitamin K are not expected to affect the anticoagulant activity of dabigatran. Consider administration of platelet concentrates in cases where thrombocytopenia is present or long-acting antiplatelet drugs have been used.
Thromboembolic and Bleeding Events in Patients with Prosthetic Heart Valves
The safety and efficacy of PRADAXA in patients with bileaflet mechanical prosthetic heart valves was evaluated in the RE-ALIGN trial, in which patients with bileaflet mechanical prosthetic heart valves (recently implanted or implanted more than three months prior to enrollment) were randomized to dose adjusted warfarin or 150, 220, or 300 mg of PRADAXA twice a day. RE-ALIGN was terminated early due to the occurrence of significantly more thromboembolic events (valve thrombosis, stroke, transient ischemic attack, and myocardial infarction) and an excess of major bleeding (predominantly post-operative pericardial effusions requiring intervention for hemodynamic compromise) in the PRADAXA treatment arm as compared to the warfarin treatment arm. These bleeding and thromboembolic events were seen both in patients who were initiated on PRADAXA post-operatively within three days of mechanical bileaflet valve implantation, as well as in patients whose valves had been implanted more than three months prior to enrollment. Therefore, the use of PRADAXA is contraindicated in patients with mechanical prosthetic valves [see Contraindications (4)].
The use of PRADAXA for the prophylaxis of thromboembolic events in patients with atrial fibrillation in the setting of other forms of valvular heart disease, including the presence of a bioprosthetic heart valve, has not been studied and is not recommended.
Effect of P-gp Inducers and Inhibitors on Dabigatran Exposure
The concomitant use of PRADAXA with P-gp inducers (e.g. rifampin) reduces exposure to dabigatran and should generally be avoided [see Clinical Pharmacology(12.3)].
P-gp inhibition and impaired renal function are the major independent factors that result in increased exposure to dabigatran [see Clinical Pharmacology (12.3)]. Concomitant use of P-gp inhibitors in patients with renal impairment is expected to produce increased exposure of dabigatran compared to that seen with either factor alone.
Consider reducing the dose of PRADAXA to 75 mg twice daily when dronedarone or systemic ketoconazole is coadministered with PRADAXA in patients with moderate renal impairment (CrCl 30-50 mL/min). Avoid use of PRADAXA and P-gp inhibitors in patients with severe renal impairment (CrCl 15-30 mL/min) [see Drug Interactions (7) and Use in Specific Populations (8.6)]. |clinicalTrials=Because clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The RE-LY (Randomized Evaluation of Long-term Anticoagulant Therapy) study provided safety information on the use of two doses of PRADAXA and warfarin [see Clinical Studies (14)]. The numbers of patients and their exposures are described in Table 1. Limited information is presented on the 110 mg dosing arm because this dose is not approved.
 |
Drug Discontinuation in RE-LY
The rates of adverse reactions leading to treatment discontinuation were 21% for PRADAXA 150 mg and 16% for warfarin. The most frequent adverse reactions leading to discontinuation of PRADAXA were bleeding and gastrointestinal events (i.e., dyspepsia, nausea, upper abdominal pain, gastrointestinal hemorrhage, and diarrhea).
Bleeding [see Warnings and Precautions (5.2)]
Table 2 shows the number of patients experiencing serious bleeding during the treatment period in the RE-LY study, with the bleeding rate per 800 patient-years (%). Major bleeds fulfilled one or more of the following criteria: bleeding associated with a reduction in hemoglobin of at least 2 grams per deciliter or leading to a transfusion of at least 2 units of blood, or symptomatic bleeding in a critical area or organ (intraocular, intracranial, intraspinal or intramuscular with compartment syndrome, retroperitoneal bleeding, intra-articular bleeding, or pericardial bleeding). A life-threatening bleed met one or more of the following criteria: fatal, symptomatic intracranial bleed, reduction in hemoglobin of at least 5 grams per deciliter, transfusion of at least 4 units of blood, associated with hypotension requiring the use of intravenous inotropic agents, or necessitating surgical intervention. Intracranial hemorrhage included intracerebral (hemorrhagic stroke), subarachnoid, and subdural bleeds.
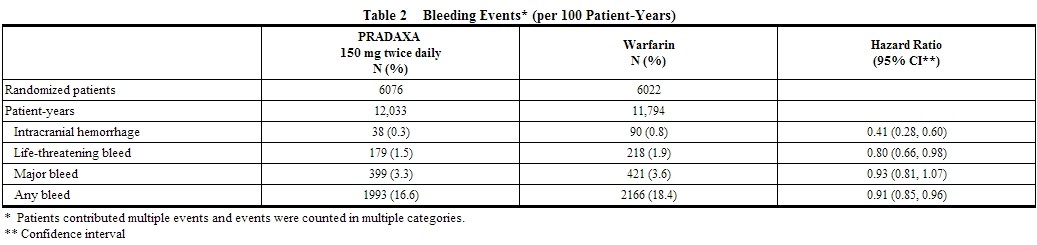 |
The risk of major bleeds was similar with PRADAXA 150 mg and warfarin across major subgroups defined by baseline characteristics, with the exception of age, where there was a trend towards a higher incidence of major bleeding on PRADAXA (hazard ratio 1.2, 95% CI: 1.0 to 1.4) for patients ≥75 years of age.
There was a higher rate of major gastrointestinal bleeds in patients receiving PRADAXA 150 mg than in patients receiving warfarin (1.6% vs. 1.1%, respectively, with a hazard ratio vs. warfarin of 1.5, 95% CI, 1.2 to 1.9), and a higher rate of any gastrointestinal bleeds (6.1% vs. 4.0%, respectively).
Gastrointestinal Adverse Reactions
Patients on PRADAXA 150 mg had an increased incidence of gastrointestinal adverse reactions (35% vs. 24% on warfarin). These were commonly dyspepsia (including abdominal pain upper, abdominal pain, abdominal discomfort, and epigastric discomfort) and gastritis-like symptoms (including GERD, esophagitis, erosive gastritis, gastric hemorrhage, hemorrhagic gastritis, hemorrhagic erosive gastritis, and gastrointestinal ulcer).
Hypersensitivity Reactions
In the RE-LY study, drug hypersensitivity (including urticaria, rash, and pruritus), allergic edema, anaphylactic reaction, and anaphylactic shock were reported in <0.1% of patients receiving PRADAXA. |postmarketing=The following adverse reactions have been identified during post approval use of PRADAXA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The following adverse reactions have been identified during post approval use of PRADAXA: angioedema, thrombocytopenia, esophageal ulcer. |drugInteractions=The concomitant use of PRADAXA with [P-gp inducers] (e.g., rifampin) reduces exposure to dabigatran and should generally be avoided [see Clinical Pharmacology(12.3)].
P-gp inhibition and impaired renal function are the major independent factors that result in increased exposure to dabigatran [see Clinical Pharmacology (12.3)]. Concomitant use of P-gp inhibitors in patients with renal impairment is expected to produce increased exposure of dabigatran compared to that seen with either factor alone.
In patients with moderate renal impairment (CrCl 30-50 mL/min), consider reducing the dose of PRADAXA to 75 mg twice daily when administered concomitantly with the P-gp inhibitor dronedarone or systemic ketoconazole. The use of P-gp inhibitors (verapamil, amiodarone, quinidine, and clarithromycin) does not require a dose adjustment of PRADAXA. These results should not be extrapolated to other P-gp inhibitors [see Warnings and Precautions (5.4), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
The concomitant use of PRADAXA and P-gp inhibitors in patients with severe renal impairment (CrCl 15-30 mL/min) should be avoided [see Warnings and Precautions(5.4), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)]. |useInPregnancyFDA=Pregnancy Category C
There are no adequate and well-controlled studies in pregnant women.
Dabigatran has been shown to decrease the number of implantations when male and female rats were treated at a dosage of 70 mg/kg (about 2.6 to 3.0 times the human exposure at maximum recommended human dose [MRHD] of 300 mg/day based on area under the curve [AUC] comparisons) prior to mating and up to implantation (gestation Day 6). Treatment of pregnant rats after implantation with dabigatran at the same dose increased the number of dead offspring and caused excess vaginal/uterine bleeding close to parturition. Although dabigatran increased the incidence of delayed or irregular ossification of fetal skull bones and vertebrae in the rat, it did not induce major malformations in rats or rabbits. |useInLaborDelivery=Safety and effectiveness of PRADAXA during labor and delivery have not been studied in clinical trials. Consider the risks of bleeding and of stroke in using PRADAXA in this setting [see Warnings and Precautions (5.2)].
Death of offspring and mother rats during labor in association with uterine bleeding occurred during treatment of pregnant rats from implantation (gestation Day 7) to weaning (lactation Day 21) with dabigatran at a dose of 70 mg/kg (about 2.6 times the human exposure at MRHD of 300 mg/day based on AUC comparisons). |useInNursing=It is not known whether dabigatran is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when PRADAXA is administered to a nursing woman. |useInPed=Safety and effectiveness of PRADAXA in pediatric patients have not been established. |useInGeri=Of the total number of patients in the RE-LY study, 82% were 65 and over, while 40% were 75 and over. The risk of stroke and bleeding increases with age, but the risk-benefit profile is favorable in all age groups [see Warnings and Precautions (5), Adverse Reactions (6.1), and Clinical Studies (14)]. |useInRenalImpair=No dose adjustment of PRADAXA is recommended in patients with mild or moderate renal impairment [see Clinical Pharmacology (12.3)]. Reduce the dose of PRADAXA in patients with severe renal impairment (CrCl 15-30 mL/min) [see Dosage and Administration (2.1, 2.2) and Clinical Pharmacology (12.3)]. Dosing recommendations for patients with CrCl <15 mL/min or on dialysis cannot be provided.
Adjust dose appropriately in patients with renal impairment receiving concomitant P-gp inhibitors [see Warnings and Precautions (5.4), Drug Interactions (7), and Clinical Pharmacology (12.3)]. |administration=Route: Oral
Instructions to Patients
Instruct patients to swallow the capsules whole. PRADAXA should be taken with a full glass of water. Breaking, chewing, or emptying the contents of the capsule can result in increased exposure [see Clinical Pharmacology (12.3)].
If a dose of PRADAXA is not taken at the scheduled time, the dose should be taken as soon as possible on the same day; the missed dose should be skipped if it cannot be taken at least 6 hours before the next scheduled dose. The dose of PRADAXA should not be doubled to make up for a missed dose.
Converting from or to Warfarin
When converting patients from warfarin therapy to PRADAXA, discontinue warfarin and start PRADAXA when the INR is below 2.0.
When converting from PRADAXA to warfarin, adjust the starting time of warfarin based on creatinine clearance as follows:
For CrCl ≥50 mL/min, start warfarin 3 days before discontinuing PRADAXA. For CrCl 30-50 mL/min, start warfarin 2 days before discontinuing PRADAXA. For CrCl 15-30 mL/min, start warfarin 1 day before discontinuing PRADAXA. For CrCl <15 mL/min, no recommendations can be made.
Because PRADAXA can increase INR, the INR will better reflect warfarin’s effect only after PRADAXA has been stopped for at least 2 days [see Clinical Pharmacology (12.2)].
Converting from or to Parenteral Anticoagulants
For patients currently receiving a parenteral anticoagulant, start PRADAXA 0 to 2 hours before the time that the next dose of the parenteral drug was to have been administered or at the time of discontinuation of a continuously administered parenteral drug (e.g., intravenous unfractionated heparin).
For patients currently taking PRADAXA, wait 12 hours (CrCl ≥30 mL/min) or 24 hours (CrCl <30 mL/min) after the last dose of PRADAXA before initiating treatment with a parenteral anticoagulant [see Clinical Pharmacology (12.3)].
Surgery and Interventions
If possible, discontinue PRADAXA 1 to 2 days (CrCl ≥50 mL/min) or 3 to 5 days (CrCl <50 mL/min) before invasive or surgical procedures because of the increased risk of bleeding. Consider longer times for patients undergoing major surgery, spinal puncture, or placement of a spinal or epidural catheter or port, in whom complete hemostasis may be required [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
If surgery cannot be delayed, there is an increased risk of bleeding [see Warnings and Precautions (5.2)]. This risk of bleeding should be weighed against the urgency of intervention [see Warnings and Precautions (5.1)]. |monitoring=INR is relatively insensitive to the exposure to dabigatran and cannot be interpreted the same way as used for warfarin monitoring. |IVCompat=FDA Package Insert for Metoprolol tartrate contains no information regarding Black Box Warning. |overdose=Accidental overdose may lead to hemorrhagic complications. There is no reversal agent for dabigatran. In the event of hemorrhagic complications, initiate appropriate clinical support, discontinue treatment with PRADAXA, and investigate the source of bleeding. Dabigatran is primarily eliminated by the kidneys with a low plasma protein binding of approximately 35%. Hemodialysis can remove dabigatran; however, data supporting this approach are limited. Using a high-flux dialyzer, blood flow rate of 200 mL/min, and dialysate flow rate of 700 mL/min, approximately 49% of total dabigatran can be cleared from plasma over 4 hours. At the same dialysate flow rate, approximately 57% can be cleared using a dialyzer blood flow rate of 300 mL/min, with no appreciable increase in clearance observed at higher blood flow rates. Upon cessation of hemodialysis, a redistribution effect of approximately 7% to 15% is seen. The effect of dialysis on dabigatran’s plasma concentration would be expected to vary based on patient specific characteristics. Measurement of aPTT or ECT may help guide therapy. }}