Copanlisib
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sonya Gelfand
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Copanlisib is a kinase inhibitor that is FDA approved for the treatment of adult patients with relapsed follicular lymphoma (FL) who have received at least two prior systemic therapies. Common adverse reactions include hyperglycemia, diarrhea, decreased general strength and energy, hypertension, leukopenia, neutropenia, nausea, lower respiratory tract infections, and thrombocytopenia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Condition 1
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Condition 2
- Developed by: (Organisation)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- (Dosage)
Condition 2
- Dosing Information
- (Dosage)
Condition 3
- Dosing Information
- (Dosage)
Contraindications
CONTRAINDICATIONS
Warnings
Conidition 1
(Description)
Conidition 2
(Description)
Conidition 3
(Description)
Adverse Reactions
Clinical Trials Experience
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Condition 2
Central Nervous System
- (list/description of adverse reactions)
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- (list/description of adverse reactions)
Gastrointestinal
- (list/description of adverse reactions)
Hypersensitive Reactions
- (list/description of adverse reactions)
Miscellaneous
- (list/description of adverse reactions)
Postmarketing Experience
(Description)
Drug Interactions
- Drug 1
- Drug 2
- Drug 3
- Drug 4
- Drug 5
Drug 1
(Description)
Drug 2
(Description)
Drug 3
(Description)
Drug 4
(Description)
Drug 5
(Description)
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
(Description)
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Copanlisib in women who are pregnant.
Labor and Delivery
(Description)
Nursing Mothers
(Description)g
Pediatric Use
(Description)
Geriatic Use
(Description)
Gender
(Description)
Race
(Description)
Renal Impairment
(Description)
Hepatic Impairment
(Description)
Females of Reproductive Potential and Males
(Description)
Immunocompromised Patients
(Description)
Others
(Description)
Administration and Monitoring
Administration
(Oral/Intravenous/etc)
Monitoring
Condition 1
(Description regarding monitoring, from Warnings section)
Condition 2
(Description regarding monitoring, from Warnings section)
Condition 3
(Description regarding monitoring, from Warnings section)
IV Compatibility
There is limited information regarding the compatibility of Copanlisib and IV administrations.
Overdosage
Acute Overdose
Signs and Symptoms
(Description)
Management
(Description)
Chronic Overdose
Signs and Symptoms
(Description)
Management
(Description)
Pharmacology
Mechanism of Action
- Copanlisib is an inhibitor of phosphatidylinositol-3-kinase (PI3K) with inhibitory activity predominantly against PI3K-α and PI3K-δ isoforms expressed in malignant B cells. Copanlisib has been shown to induce tumor cell death by apoptosis and inhibition of proliferation of primary malignant B cell lines. Copanlisib inhibits several key cell-signaling pathways, including B-cell receptor (BCR) signaling, CXCR12 mediated chemotaxis of malignant B cells, and NFκB signaling in lymphoma cell lines.
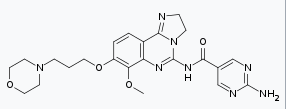
Structure

Pharmacodynamics
- At 60 mg (or 0.8 mg/kg) of Copanlisib dose, the elevation of plasma glucose was associated with higher Copanlisib exposure.
Pharmacokinetics
- The area under the plasma concentration-time curve (AUC) and maximum plasma concentration (Cmax) of Copanlisib increase dose-proportionally over 5 to 93 mg (0.08 to 1.55 times the approved recommended dose) absolute dose range and exhibit linear pharmacokinetics. There is no time-dependency and no accumulation in the pharmacokinetics of Copanlisib.
- The geometric mean (range) steady state Copanlisib exposure at 0.8 mg/kg (approximately the approved recommended dose of 60 mg) are 463 (range: 105 to 1670; SD: 584) ng/mL for Cmax and 1570 (range: 536 to 3410; SD: 338) ng.hr/mL for AUC0-25h.
Distribution
- The in vitro human plasma protein binding of Copanlisib is 84.2%. Albumin is the main binding protein. The in vitro mean blood-to-plasma ratio is 1.7 (range: 1.5 to 2.1). The geometric mean volume of distribution is 871 (range: 423 to 2150; SD: 479) L.
Elimination
- The geometric mean terminal elimination half-life of Copanlisib is 39.1 (range: 14.6 to 82.4; SD: 15.0) hours. The geometric mean clearance is 17.9 (range: 7.3 to 51.4; SD: 8.5) L/hr.
Metabolism
- Approximately >90% of Copanlisib metabolism is mediated by CYP3A and <10% by CYP1A1. The M-1 metabolite accounts for 5% of total radioactivity AUC and its pharmacological activity is comparable to the parent compound Copanlisib for the tested kinases PI3KandPI3K.
Excretion
Copanlisib is excreted approximately 50% as unchanged compound and 50% as metabolites in humans. Following a single intravenous dose of 12 mg (0.2 times the recommended approved dose) radiolabeled Copanlisib, approximately 64% of the administered dose was recovered in feces and 22% in urine within 20 to 34 days. Unchanged Copanlisib represented approximately 30% of the administered dose in feces and 15% in urine. Metabolites resulting from CYP450-mediated oxidation metabolism accounted for 41% of the administered dose.
Specific Populations
- Copanlisib pharmacokinetic differences in the subpopulations listed below are assessed using population pharmacokinetic analyses.
- Age (20 to 90 years), gender, race (White, Asian, Hispanic, and Black), smoking status, body weight (41 to 130 kg), mild hepatic impairment [total bilirubin (TB) ≤ upper limit of normal (ULN) and aspartate aminotransferase (AST) > ULN, or TB < 1-1.5 x ULN and any AST], and mild to moderate renal impairment [CLcr ≥ 30 mL/min as estimated by Cockcroft-Gault (C-G) equation] had no clinically significant effect on the pharmacokinetics of Copanlisib. The pharmacokinetics of Copanlisib in patients with moderate to severe hepatic impairment (TB ≥ 1.5 x ULN, any AST), severe renal impairment (CLcr = 15-29 mL/min by C-G equation), or end stage renal disease (CLcr < 15 mL/min by C-G equation) with or without dialysis is unknown.
Drug Interaction Studies
Clinical Studies
Effect of CYP3A and P-gp Inducers on Copanlisib
- Rifampin, a strong CYP3A and a P-glycoprotein (P-gp) transporter inducer, administered at a dose of 600 mg once daily for 12 days with a single intravenous dose of 60 mg Copanlisib in patients with cancer resulted in a 63% decrease in the mean AUC and a 15% decrease in Cmax of Copanlisib.
Effect of CYP3A, P-gp and BCRP Inhibitors on Copanlisib
- Itraconazole, a strong CYP3A inhibitor and a P-gp and Breast Cancer Resistance Protein (BCRP) transporter inhibitor, administered at a dose of 200 mg once daily for 10 days increased the mean AUC of a single intravenous dose of 60 mg Copanlisib by 53% (or 1.53-fold) with no effect on Cmax (1.03-fold) in patients with cancer.
In Vitro Studies
Effect of Transporters on Copanlisib:
- Copanlisib is a substrate of P-gp and BCRP, but not a substrate for organic cation transporter (OCT) 1, OCT2, and OCT3, organic anion transporter (OAT) 1 and OAT3, organic anion-transporting polypeptide (OATP) 1B1 and OATP1B3, multidrug and toxin extrusion protein 1(MATE1) or MATE2-K.
Effect of Copanlisib on CYP and non-CYP Enzymes
- Copanlisib is not an inhibitor of the metabolism of drugs that are substrates of the major CYP isoforms (CYP1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, and 3A4) or uridine diphosphate-glucuronosyltransferase isoforms (UGT) or dihydropyrimidine dehydrogenase (DPD) at therapeutic 60 mg dose plasma concentrations. Copanlisib is not an inducer of CYP1A2, CYP2B6 and CYP3A.
Effect of Copanlisib on Drug Transporter Substrates
- Copanlisib is not an inhibitor of P-gp, BCRP, multi-drug resistance-associated protein (MRP2), bile salt export pump (BSEP), OATP1B1, OATP1B3, OAT1, OAT3, OCT1, OCT2, and MATE1 at therapeutic 60 mg dose plasma concentrations.
- Copanlisib is an inhibitor of MATE2-K (IC50: 0.09 μM). Based on the PK of Copanlisib,inhibition may occur after Copanlisib infusion at approved recommended dosage. The clinical significance of this potential inhibition on plasma concentrations of concomitantly administered drugs that are MATE2-K substrates is unknown.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Carcinogenicity studies have not been conducted with Copanlisib.
- Copanlisib did not cause genetic damage in in vitro or in vivo assays.
- Fertility studies with Copanlisib were not conducted; however, adverse findings in male and female reproductive systems were observed in the repeat dose toxicity studies. Findings in the male rats and/or dogs included effects on the testes (germinal epithelial degeneration, decreased weight, and/or tubular atrophy), epididymides (spermatic debris, decreased weight, and/or oligospermia/aspermia), and prostate (reduced secretion and/or decreased weight). Findings in female rats included effects on ovaries (hemorrhage, hemorrhagic cysts, and decreased weight), uterus (atrophy, decreased weight), vagina (mononuclear infiltration), and a dose-related reduction in the numbers of female rats in estrus.
Clinical Studies
Relapsed Follicular Lymphoma
- The efficacy of Copanlisib was evaluated in a single-arm, multicenter, phase 2 clinical trial (NCT 01660451) CHRONOS-1 in a total of 142 subjects, which included 104 subjects with follicular B-cell non-Hodgkin lymphoma who had relapsed disease following at least two prior treatments. Patients must have received rituximab and an alkylating agent. Baseline patient characteristics are summarized in Table 4. The most common prior systemic therapies were chemotherapy in combination with anti-CD20 immunotherapy (89%), chemotherapy alone (41%), and anti-CD20 immunotherapy alone (37%). In CHRONOS-1, 34% of patients received two prior lines of therapy and 36% received three prior lines of therapy.

- Refractory: No response or progression of disease within six months of last treatment.
- One hundred forty-two patients received 60 mg Copanlisib; 130 patients received fixed dose 60 mg Copanlisib and 12 patients received 0.8 mg/kg equivalent Copanlisib administered as a 1-hour intravenous infusion on Days 1, 8, and 15 of a 28-day treatment cycle on an intermittent schedule (three weeks on and one week off). Treatment continued until disease progression or unacceptable toxicity. Tumor response was assessed according to the International Working Group response criteria for malignant lymphoma. Efficacy based on overall response rate (ORR) was assessed by an Independent Review Committee. Efficacy results from CHRONOS-1 are summarized in Table 5.

How Supplied
- Copanlisib is contained in a colorless glass vial closed with bromobutyl stopper with a flanged closure. Each vial of Copanlisib contains Copanlisib as a lyophilized solid.

Storage
Product as packaged for sale
- Copanlisib vials must be refrigerated at 2°C to 8°C (36°F to 46°F).
Product after reconstitution
- Administer reconstituted and diluted solution immediately. If not, refrigerate at 2°C to 8°C (36°F to 46°F) and use within 24 hours. After refrigeration, allow the product to adapt to room temperature before use. Avoid exposure of the diluted solution to direct sunlight.
- Mix only with 0.9% NaCl solution. Do not mix or inject Copanlisib with other drugs or other diluents.
Images
Drug Images
{{#ask: Page Name::Copanlisib |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

{{#ask: Label Page::Copanlisib |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Infections – Advise patients that Copanlisib can cause serious infections that may be fatal. Advise patients to immediately report symptoms of infection
- Hyperglycemia – Advise patients that an infusion-related increase in blood glucose may occur, and to notify their healthcare provider of any symptoms such as pronounced hunger, excessive thirst, headaches, or frequently urinating. Blood glucose levels should be well controlled prior to infusion
- Hypertension – Advise patients that an infusion-related increase in blood pressure may occur, and to notify their healthcare provider of any symptoms such as dizziness, passing out, headache, and/or a pounding heart. Blood pressure should be normal or well controlled prior to infusion
- Non-infectious pneumonitis – Advise patients of the possibility of pneumonitis, and to report any new or worsening respiratory symptoms including cough or difficulty breathing
- Neutropenia – Advise patients of the need for periodic monitoring of blood counts and to notify their healthcare provider immediately if they develop a fever or any signs of infection
- Severe cutaneous reactions – Advise patients that a severe cutaneous reaction may occur, and to notify their healthcare provider if they develop skin reactions (rash, redness, swelling, itching or peeling of the skin)
- Pregnancy – Advise females of reproductive potential to use effective contraceptive methods and to avoid becoming pregnant during treatment with Copanlisib and for at least one month after the last dose. Advise patients to notify their healthcare provider immediately in the event of a pregnancy or if pregnancy is suspected during Copanlisib treatment. Advise males with female partners of reproductive potential to use effective contraception during treatment with Copanlisib and for at least one month after the last dose
- Lactation – Advise women not to breastfeed during treatment with Copanlisib and for at least 1 month after the last dose

Precautions with Alcohol
Alcohol-Copanlisib interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Aliqopa
Look-Alike Drug Names
There is limited information regarding Copanlisib Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.