Cobicistat
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Gloria Picoy [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Cobicistat is an anti-infective agent that is FDA approved for the treatment of HIV-1 infection. Common adverse reactions include jaundice, ocular icterus, and nausea.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
TYBOST is a CYP3A inhibitor indicated to increase systemic exposure of atazanavir or darunavir (once daily dosing regimen) in combination with other antiretroviral agents in the treatment of HIV-1 infection.
- Dosage:
- Cobicistat 150 mg orally once daily plus atazanavir 300 mg orally once daily; or
- Cobicistat 150 mg orally once daily plus darunavir 800 mg orally once daily
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Cobicistat in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Cobicistat in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Safety and effectiveness not established in pediatric patients younger than 18 years
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Cobicistat in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Cobicistat in pediatric patients.
Contraindications
The concomitant use of TYBOST with atazanavir or darunavir and the following drugs (see TABLE 2) is contraindicated due to the potential for serious and/or life-threatening events or loss of therapeutic effect

Warnings
Effects on Serum Creatinine
TYBOST decreases estimated creatinine clearance due to inhibition of tubular secretion of creatinine without affecting actual renal glomerular function. This effect should be considered when interpreting changes in estimated creatinine clearance in patients initiating TYBOST, particularly in patients with medical conditions or receiving drugs needing monitoring with estimated creatinine clearance.
Prior to initiating therapy with TYBOST, assess estimated creatinine clearance. Dosage recommendations are not available for drugs that require dosage adjustments in TYBOST-treated patients with renal impairment. Consider alternative medications that do not require dosage adjustments in patients with renal impairment.
Although TYBOST may cause modest increases in serum creatinine and modest declines in estimated creatinine clearance without affecting renal glomerular function, patients who experience a confirmed increase in serum creatinine of greater than 0.4 mg/dL from baseline should be closely monitored for renal safety.
New Onset or Worsening Renal Impairment When Used with Tenofovir Disoproxil Fumarate
Renal impairment, including cases of acute renal failure and Fanconi syndrome, has been reported when TYBOST was used in an antiretroviral regimen that contained tenofovir DF.
- Coadministration of TYBOST and tenofovir DF is not recommended in patients who have an estimated creatinine clearance below 70 mL/min because dose adjustment of tenofovir DF is required below 50 mL/min and such dose adjustments have not been established for coadministration with TYBOST.
- Document urine glucose and urine protein at baseline and perform routine monitoring of estimated creatinine clearance, urine glucose, and urine protein during treatment when TYBOST is used with tenofovir DF. Measure serum phosphorus in patients with or at risk for renal impairment when used with tenofovir DF.
- Coadministration of TYBOST and tenofovir DF in combination with concomitant or recent use of a nephrotoxic agent is not recommended.
In the clinical trials of TYBOST over 48 weeks (N=771), 6 (1.5%) subjects treated with TYBOST coadministered with atazanavir and TRUVADA® and 6 (1.6%) subjects treated with ritonavir coadministered with atazanavir and TRUVADA discontinued study drug due to a renal adverse event. Five of the 6 subjects (1.3% overall) in the TYBOST group had laboratory findings consistent with proximal renal tubulopathy leading to study drug discontinuation compared to 2 of 6 subjects (0.5% overall) in the ritonavir group. None of the 5 subjects in the TYBOST group had renal impairment at baseline (i.e., estimated creatinine clearance less than 70 mL/min). The laboratory findings in these 5 subjects with evidence of proximal tubulopathy improved but did not completely resolve in all subjects upon discontinuation of TYBOST coadministered with atazanavir and TRUVADA. Renal replacement therapy was not required in any subject.
Risk of Serious Adverse Reactions or Loss of Virologic Response Due to Drug Interactions
Initiation of TYBOST, a CYP3A inhibitor, in patients receiving medications metabolized by CYP3A, or initiation of medications metabolized by CYP3A in patients already receiving TYBOST may increase plasma concentration of these medications which may increase the risk of clinically significant adverse reactions (including life-threatening or fatal reactions) associated with the concomitant medications. Coadministration of TYBOST with atazanavir or darunavir in combination with CYP3A inducers may lead to lower exposure of cobicistat and atazanavir or darunavir and loss of efficacy of atazanavir or darunavir and possible resistance. Therefore, consider the potential for drug interactions prior to and during TYBOST therapy; review concomitant medications during TYBOST therapy; and monitor for the adverse reactions associated with the concomitant drugs.
TYBOST or ritonavir when administered with either atazanavir or darunavir may result in different drug interactions when used with concomitant medications. Complex or unknown mechanisms of drug interactions preclude extrapolation of ritonavir drug interactions to certain TYBOST interactions.
Antiretrovirals that are Not Recommended
The following antiretrovirals are not recommended in combination with TYBOST because dosing recommendations for such combinations have not been established and coadministration may result in decreased plasma concentrations of the antiretroviral agents, leading to loss of therapeutic effect and development of resistance:
- More than one antiretroviral that requires pharmacokinetic enhancement (i.e., two protease inhibitors or a protease inhibitor in combination with elvitegravir)
- Darunavir in combination with efavirenz, nevirapine, or etravirine
- Atazanavir in combination with etravirine
- Atazanavir in combination with efavirenz in treatment-experienced patients
- Darunavir 600 mg twice daily
- Other HIV-1 protease inhibitors including fosamprenavir, saquinavir, or tipranavir
TYBOST in combination with STRIBILD® fixed-dose combination tablets (elvitegravir, cobicistat, emtricitabine, tenofovir DF) is not recommended because cobicistat is a component of STRIBILD.
TYBOST in combination with lopinavir/ritonavir or regimens containing ritonavir is not recommended due to similar effects of TYBOST and ritonavir on CYP3A.
Adverse Reactions
Clinical Trials Experience
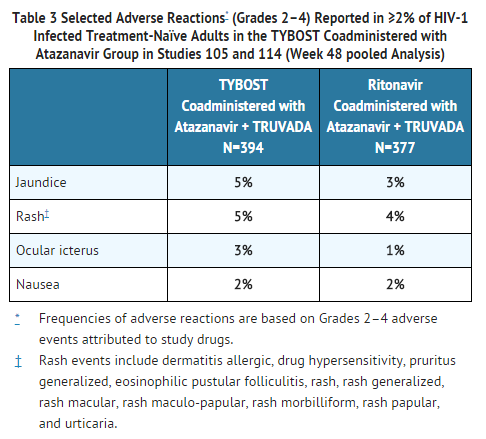
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of TYBOST has been established from a Phase 2 trial, Study 105, and a Phase 3 trial, Study 114. In the pooled analysis, 771 HIV-1 infected, antiretroviral treatment-naïve adults received for at least 48 weeks:
- TYBOST coadministered with atazanavir and tenofovir DF/emtricitabine (administered as TRUVADA) (N=394) or;
- ritonavir coadministered with atazanavir and tenofovir DF/emtricitabine (administered as TRUVADA ) (N=377).
The most common adverse reactions (all Grades) and reported in >10% of subjects in the TYBOST group were jaundice (13%), ocular icterus (15%), and nausea (12%); the most common adverse reactions in the ritonavir group were jaundice (11%), ocular icterus (17%), nausea (11%), and diarrhea (11%). The proportion of subjects who discontinued study treatment due to adverse events, regardless of severity, was 7% in both the TYBOST and ritonavir group. Table 3 displays the frequency of adverse reactions (Grades 2–4) occurring in at least 2% of subjects in the TYBOST group in pooled Studies 105 and 114.
Nephrolithiasis
Nephrolithiasis has previously been identified in patients receiving atazanavir. In the pooled analysis of Studies 105 and 114 through 48 weeks, 8 subjects (2%) receiving TYBOST coadministered with atazanavir and TRUVADA developed nephrolithiasis compared with no subjects receiving ritonavir coadministered with atazanavir and TRUVADA. Median time to onset of nephrolithiasis in the TYBOST group was 24 weeks. Causality in these cases could not be determined with certainty, but the majority of renal stone events were not serious and no subject discontinued study drug.
Less Common Adverse Reactions
Selected adverse reactions of at least moderate severity (≥ Grade 2) occurring in less than 2% of subjects receiving TYBOST coadministered with atazanavir and TRUVADA are listed below. These events have been included because of the investigator's assessment of potential causal relationship and were considered serious or have been reported in more than one subject treated with TYBOST and with greater frequency compared with ritonavir.
- Gastrointestinal Disorders: diarrhea, vomiting, upper abdominal pain
- General Disorders and Administration Site Conditions: fatigue
- Musculoskeletal and Connective Tissue Disorders: rhabdomyolysis
- Nervous System Disorders: headache
- Psychiatric Disorders: depression, abnormal dreams, insomnia
- Renal and Urinary Disorders: nephropathy, Fanconi syndrome acquired
Refer to the prescribing information for atazanavir or darunavir for information regarding adverse reactions with these drugs.
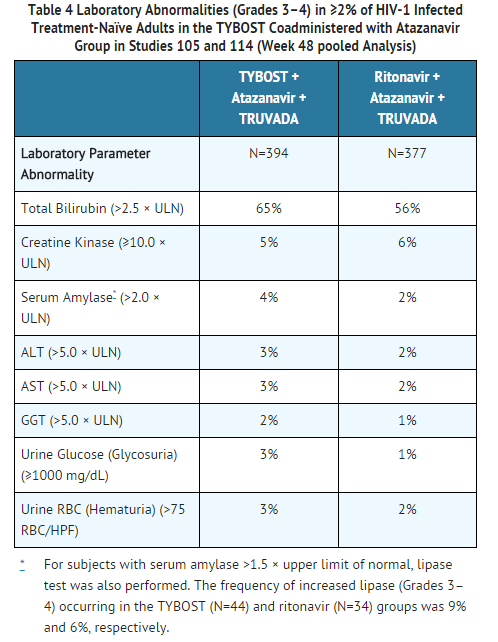
Laboratory Abnormalities
The frequency of laboratory abnormalities (Grades 3–4) occurring in at least 2% of subjects in the TYBOST group in Studies 105 and 114 is presented in Table 4.
Increase in Serum Creatinine: TYBOST causes increases in serum creatinine and decreases in estimated creatinine clearance due to inhibition of tubular secretion of creatinine without affecting actual renal glomerular function. In Studies 105 and 114, increases in serum creatinine and decreases in estimated creatinine clearance occurred early in treatment with TYBOST, after which they stabilized. The mean (± SD) change in estimated glomerular filtration rate (eGFR) by Cockcroft-Gault method after 48 weeks of treatment was -13.4 ± 15.2 mL/min in the TYBOST group and -9.1 ± 14.7 mL/min in the ritonavir group.
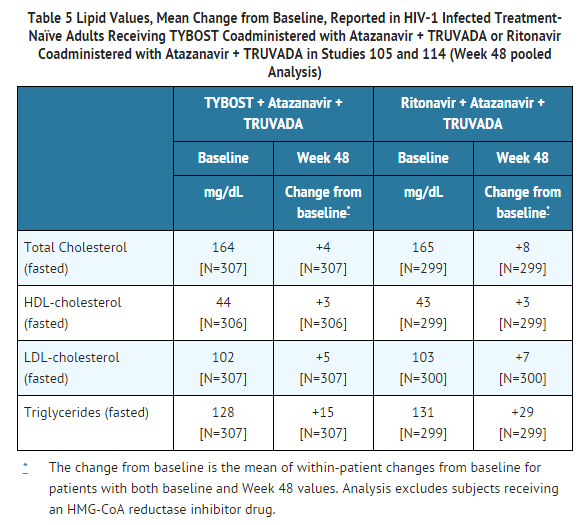
Serum Lipids: Changes from baseline in total cholesterol, HDL-cholesterol, LDL-cholesterol, and triglycerides are presented in Table 5. In both groups, mean values for serum lipids remained within the study reference range for each laboratory test. The clinical significance of these changes is unknown.
Postmarketing Experience
There is limited information regarding Cobicistat Postmarketing Experience in the drug label.
Drug Interactions
Cobicistat is an inhibitor of CYP3A and CYP2D6. The transporters that cobicistat inhibits include p-glycoprotein (P-gp), BCRP, OATP1B1 and OATP1B3. The plasma concentration of drugs that are primarily metabolized by CYP3A or CYP2D6, or are substrates of P-gp, BCRP, OATP1B1 or OATP1B3 may be increased if those drugs are coadministered with TYBOST.
Based on in vitro data, cobicistat is not expected to induce CYP1A2 or CYP2B6 and based on in vivo data, cobicistat is not expected to induce MDR1 or, in general, CYP3A to a clinically significant extent. The induction effect of cobicistat on CYP2C9, CYP2C19, or UGT1A1 is unknown, but is expected to be low based on CYP3A in vitro induction data.
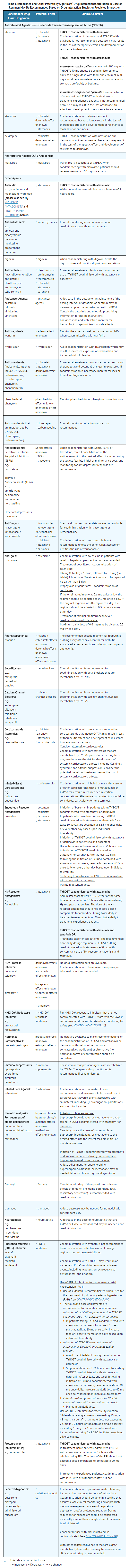
Coadministration of TYBOST with atazanavir or darunavir with drugs highly dependent on CYP3A for clearance and for which elevated plasma concentrations are associated with serious and/or life-threatening events is contraindicated. Coadministration with other CYP3A substrates may require a dose adjustment or additional monitoring as shown in Table 6.
Cobicistat is metabolized by CYP3A, and to a minor extent, by CYP2D6. Atazanavir and darunavir are also metabolized by CYP3A.
Coadministration of TYBOST with atazanavir or darunavir in combination with drugs that induce CYP3A activity have the potential to decrease plasma concentrations of cobicistat, atazanavir and darunavir, which may lead to loss of therapeutic effect and development of resistance (see TABLE 6).
Coadministration of TYBOST with atazanavir or darunavir in combination with other drugs that inhibit CYP3A may further increase the plasma concentrations of cobicistat, atazanavir and darunavir (see TABLE 6).
Established and Other Potentially Significant Interactions
Coadministration of TYBOST with fosamprenavir, saquinavir, or tipranavir is not recommended because pharmacokinetic data are not available to provide appropriate dosing recommendations. Use of TYBOST with lopinavir is not recommended because lopinavir is co-formulated with ritonavir.
Drug interaction trials were not conducted for TYBOST in combination with atazanavir or darunavir. As a single entity, drug interaction trials were conducted with TYBOST and desipramine, digoxin, and efavirenz. Drug interaction trials of TYBOST coadministered with elvitegravir were conducted that included rosuvastatin and rifabutin.
Table 6 provides dosing recommendations as a result of drug interactions with TYBOST. These recommendations are based on either drug interaction trials or predicted interactions due to the expected magnitude of the interaction and potential for serious adverse events or loss of therapeutic effect.
In Table 6, if not specifically stated, the drug interaction information applies to both coadministered agents: TYBOST coadministered with atazanavir or darunavir.
In addition to the drug interactions noted in Table 6, TYBOST is not recommended for use in combination with STRIBILD tablets, lopinavir/ritonavir or regimens containing ritonavir, or in combination with more than one antiretroviral agent that requires pharmacokinetic enhancement.
Evaluate whether dosing adjustments of concomitant medications or coadministered antiretroviral drugs are necessary in:
- Patients on a stable concomitant medication who initiate or switch to a TYBOST-containing regimen
- Patients on a TYBOST-containing regimen who initiate a new concomitant medication
- Patients initiating a TYBOST-containing regimen and a new concomitant medication simultaneously
Under these circumstances, also monitor for adverse events and/or monitor concentrations of concomitant medications if appropriate.
No dose adjustment is required when tenofovir DF or rilpivirine are coadministered with TYBOST and atazanavir or darunavir.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): B There are no adequate and well-controlled trials of TYBOST in pregnant women. Because animal reproduction studies are not always predictive of human response, TYBOST should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Animal Data
Studies of cobicistat in animals have shown no evidence of teratogenicity or an effect on reproductive function. In offspring from rat and rabbit dams treated with cobicistat during pregnancy, there were no toxicologically significant effects on developmental endpoints. The exposures at the embryo-fetal No Observed Adverse Effects Levels (NOAELs) in rats and rabbits were respectively 1.4 and 3.3 times higher than the exposure in humans at the recommended daily dose of 150 mg.
Pregnancy Category (AUS): B1
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Cobicistat in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Cobicistat during labor and delivery.
Nursing Mothers
The Centers for Disease Control and Prevention recommend that HIV-infected mothers not breastfeed their infants, to avoid risking postnatal transmission of HIV. Studies in rats have demonstrated that cobicistat is secreted in milk. It is not known whether cobicistat is excreted in human milk. Because of both the potential for HIV transmission and the potential for serious adverse reactions in nursing infants, instruct mothers not to breastfeed.
Pediatric Use
Safety and effectiveness of TYBOST in pediatric patients less than 18 years of age have not been established.
Geriatic Use
Clinical trials of TYBOST did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects.
Gender
No clinically relevant pharmacokinetic differences have been observed between men and women for cobicistat.
Race
Population pharmacokinetic analysis of cobicistat in HIV-1 infected subjects indicated that race had no clinically relevant effect on the exposure of cobicistat.
Renal Impairment
No dosage adjustment of TYBOST is required in patients with renal impairment, including those with severe renal impairment. No clinically relevant differences in cobicistat pharmacokinetics were observed between subjects with severe renal impairment and healthy subjects. TYBOST is coadministered with atazanavir or darunavir; therefore, refer to the prescribing information for atazanavir or darunavir for information regarding dosing recommendations of these drugs in patients with renal impairment.
TYBOST has been shown to decrease estimated creatinine clearance without affecting actual renal glomerular function. Dosing recommendations are not available for drugs that require dosing adjustment for renal impairment when used in combination with TYBOST.
Hepatic Impairment
No dosing adjustment of TYBOST is necessary for patients with mild-to-moderate hepatic impairment. No data are available in patients with severe hepatic impairment. TYBOST is coadministered with atazanavir or darunavir and other antiretroviral drugs; therefore, refer to the prescribing information of these other drugs for information regarding dosing recommendations in patients with hepatic impairment.
Females of Reproductive Potential and Males
Cobicistat did not affect fertility in male or female rats at daily exposures (AUC) approximately 3-fold higher than human exposures at the recommended 150 mg daily dose.
Fertility was normal in the offspring of rats exposed daily from before birth (in utero) through sexual maturity at daily exposures (AUC) of approximately similar human exposures at the recommended 150 mg daily dose.
Immunocompromised Patients
There is no FDA guidance one the use of Cobicistat in patients who are immunocompromised.
Administration and Monitoring
Administration
Oral
Monitoring
There is limited information regarding Cobicistat Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Cobicistat and IV administrations.
Overdosage
If overdose occurs, the patient must be monitored for evidence of toxicity. Treatment of overdose with TYBOST consists of general supportive measures including monitoring of vital signs, as well as observation of the clinical status of the patient.
As cobicistat is highly bound to plasma proteins, it is unlikely that it will be significantly removed by hemodialysis or peritoneal dialysis.
Pharmacology
There is limited information regarding Cobicistat Pharmacology in the drug label.
Mechanism of Action
Cobicistat is a mechanism-based inhibitor of cytochrome P450 3A (CYP3A). Inhibition of CYP3A-mediated metabolism by cobicistat increases the systemic exposure of CYP3A substrates atazanavir and darunavir.
Structure
It has the following structural formula:

Pharmacodynamics
=Effects on Pharmacokinetic Enhancement=
The effect of TYBOST on atazanavir pharmacokinetics was evaluated in the pharmacokinetic substudy (N=48) of Study 114 in which HIV-1 infected subjects received atazanavir 300 mg coadministered with TYBOST 150 mg or atazanavir 300 mg coadministered with ritonavir 100 mg, both in combination with TRUVADA. The steady-state pharmacokinetic parameters of atazanavir were comparable when coadministered with TYBOST versus ritonavir groups as shown in Table 7.

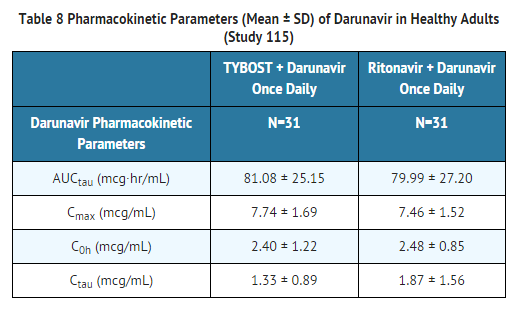
The effect of TYBOST on darunavir was evaluated in a clinical study (Study 115) in 31 healthy subjects who received darunavir 800 mg in combination with TYBOST 150 mg or ritonavir 100 mg, all once daily, for 10 days. With the exception of Ctau, the steady-state pharmacokinetic parameters of darunavir were comparable when coadministered with TYBOST versus ritonavir as shown in Table 8, and these results were similar to those reported in previous clinical trials of darunavir 800 mg with ritonavir 100 mg once daily (refer to prescribing information for darunavir).
Cardiac Electrophysiology
The effect of a single dose of cobicistat 250 mg and 400 mg (approximately 1.7 and 2.7 times the recommended dose) on QTc interval was evaluated in a randomized, placebo- and active-controlled (moxifloxacin 400 mg) four-period crossover thorough QT study in 48 healthy subjects. In this study, no significant QTc prolongation effect of cobicistat was detected. The dose of 400 mg TYBOST is expected to cover a high exposure clinical scenario. Prolongation of the PR interval was noted in subjects receiving TYBOST in the same study. The maximum mean (95% upper confidence bound) difference in PR from placebo after baseline-correction was 9.5 (12.1) msec for 250 mg and 20.2 (22.8) msec for 400 mg of cobicistat.
Effects on Serum Creatinine
The effect of TYBOST on serum creatinine was investigated in a trial in subjects with normal renal function (eGFR ≥80 mL/min, N=12) and mild-to-moderate renal impairment (eGFR 50–79 mL/min, N=18). A statistically significant decrease in the estimated glomerular filtration rate, calculated by Cockcroft-Gault method (eGFRCG) from baseline, was observed after 7 days of treatment with cobicistat 150 mg among subjects with normal renal function (-9.9 ± 13.1 mL/min) and mild-to-moderate renal impairment (-11.9 ± 7.0 mL/min). No statistically significant changes in eGFRCG were observed compared to baseline for subjects with normal renal function or mild-to-moderate renal impairment 7 days after cobicistat was discontinued. The actual glomerular filtration rate, as determined by the clearance of probe drug iohexol, was not altered from baseline following treatment of TYBOST among subjects with normal renal function and mild-to-moderate renal impairment, indicating that cobicistat inhibits tubular secretion of creatinine, reflected as a reduction in eGFRCG, without affecting the actual glomerular filtration rate.
Pharmacokinetics
Absorption
A trial where subjects were instructed to take coadministered TYBOST and darunavir with food, median cobicistat peak plasma concentrations were observed was approximately 3.5 hours post-dose. Steady-state cobicistat Cmax, AUCtau, and Ctau (mean ± SD), values were 0.99 ± 0.3 mcg/mL (n=60), 7.6 ± 3.7 mcg*hr/mL (n=59), and 0.03 ± 0.1 mcg/mL (n=59), respectively.
Effect of Food on Oral Absorption
A food effect trial was not conducted for TYBOST. In clinical trials, TYBOST was coadministered with other antiretroviral agents [see CLINICAL STUDIES (14)] under fed conditions, in accordance with the prescribing information for these agents. It is recommended that TYBOST coadministered with atazanavir or darunavir be administered with food.
Distribution
Cobicistat is 97–98% bound to human plasma proteins and the mean blood-to-plasma ratio was approximately 0.5.
Metabolism
Cobicistat is metabolized by CYP3A and to a minor extent by CYP2D6 enzymes and does not undergo glucuronidation.
Elimination
The terminal plasma half-life of cobicistat following administration of TYBOST is approximately 3 to 4 hours. With single dose administration of [14C] cobicistat after multiple dosing of cobicistat for six days, the mean percent of the administered dose excreted in feces and urine was 86.2% and 8.2%, respectively.
Nonclinical Toxicology
=Antiviral Activity=
Cobicistat does not inhibit recombinant HIV-1 protease in a biochemical assay and has no detectable antiviral activity in cell culture against HIV-1, HBV, or HCV. The antiviral activity in cell culture of selected HIV-1 antiretroviral drugs was not antagonized by cobicistat.
=Resistance=
In an analysis of treatment-failure subjects who received TYBOST coadministered with atazanavir and TRUVADA in Study 114 through Week 48, evaluable genotypic data from paired baseline and treatment-failure isolates were available for 11 of the 12 virologic failures in the TYBOST group [3%, 11/344]. Among the 11 subjects, 2 developed the emtricitabine-associated resistance substitution M184V. No subject developed the tenofovir-associated resistance substitution K65R or any primary resistance substitution associated with protease inhibitors. In the ritonavir group, evaluable genotypic data was available for all 12 virologic failures [3%, 12/348] and no subject had emergent resistance to any component of the regimen.
=Carcinogenesis=
In a long-term carcinogenicity study in mice, no drug-related increases in tumor incidence were observed at doses up to 50 and 100 mg/kg/day (males and females, respectively). Cobicistat exposures at these doses were approximately 7 (male) and 16 (females) times, respectively, the human systemic exposure at the therapeutic daily dose. In a long-term carcinogenicity study of cobicistat in rats, an increased incidence of follicular cell adenomas and/or carcinomas in the thyroid gland was observed at doses of 25 and 50 mg/kg/day in males, and at 30 mg/kg/day in females. The follicular cell findings are considered to be rat-specific, secondary to hepatic microsomal enzyme induction and thyroid hormone imbalance, and are not relevant for humans. At the highest doses tested in the rat carcinogenicity study, systemic exposures were approximately 2 times the human systemic exposure at the therapeutic daily dose.
=Mutagenesis=
Cobicistat was not genotoxic in the reverse mutation bacterial test (Ames test), mouse lymphoma or rat micronucleus assays.
Clinical Studies
The activity of TYBOST as a CYP3A inhibitor to increase the systemic exposures of atazanavir or darunavir has been demonstrated in pharmacokinetic trials. In these trials, the exposure of atazanavir or darunavir coadministered with TYBOST 150 mg was consistent with those observed with ritonavir 100 mg. For clinical efficacy of darunavir/ritonavir 800/100 mg once daily, refer to the prescribing information for darunavir.
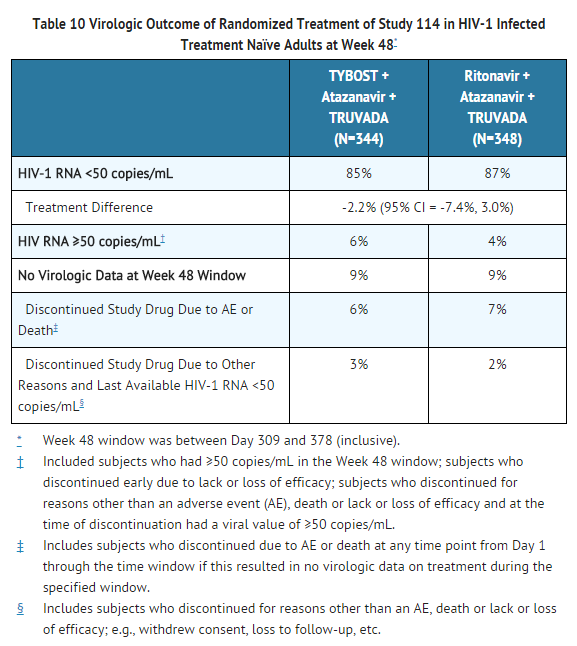
The safety and efficacy of TYBOST coadministered with atazanavir were evaluated in a randomized, double-blind, active-controlled trial (Study 114) in HIV-1 infected treatment-naïve subjects with baseline estimated creatinine clearance above 70 mL/min (N=692). In Study 114, subjects were randomized in a 1:1 ratio to receive either atazanavir 300 mg + TYBOST 150 mg once daily or atazanavir 300 mg + ritonavir 100 mg once daily. All subjects received concomitant treatment with 300 mg of tenofovir DF and 200 mg of emtricitabine once a day administered as single tablet TRUVADA. Randomization was stratified by screening HIV-1 RNA level (≤100,000 copies/mL or >100,000 copies/mL).
The mean age of subjects was 37 years (range 19–70); 83% were male, 60% were White, 18% were Black and 12% were Asian. The mean baseline plasma HIV-1 RNA was 4.8 log10 copies/mL (range 3.2–6.4). Forty percent of patients had baseline viral loads >100,000 copies/mL. The mean baseline CD4+ cell count was 352 cells/mm3 (range 1–1455) and 17% had CD4+ cell counts ≤200 cells/mm3.
Virologic outcomes in Study 114 through Week 48 are presented in Table 10. In Study 114, the mean increase from baseline in CD4+ cell count at Week 48 was 213 cells/mm3 in the TYBOST group and 219 cells/mm3 in the ritonavir group.
How Supplied
- Cobicistat tablets, 150 mg
- Each bottle contains 30 tablets (NDC 61958-1401-1)
Storage
Store at 25 °C (77 °F)
Images
Drug Images
{{#ask: Page Name::Cobicistat |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

{{#ask: Label Page::Cobicistat |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
A statement to patients and healthcare providers is included on the product's bottle label: ALERT: Find out about medicines that should NOT be taken with TYBOST. A Patient Package Insert for TYBOST is available for patient information.
- Inform patients that they should remain under the care of a healthcare provider when using TYBOST.
- Inform patients that TYBOST must be taken at the same time as atazanavir or darunavir and with food once daily as prescribed. It is important to take TYBOST and atazanavir or darunavir together on a regular dosing schedule and to avoid missing doses. Patients should be counseled about the risks of developing resistance to their HIV-1 medications.
Inform patients not to miss a dose of TYBOST with atazanavir taken together or TYBOST with darunavir taken together. If a dose of TYBOST and atazanavir or darunavir is missed by less than 12 hours, the missed dose of TYBOST with atazanavir or darunavir should be taken together right away. The next dose of TYBOST with atazanavir or darunavir should be taken together as usual. If a dose of TYBOST with atazanavir or darunavir is missed by more than 12 hours, the patient should wait and take the next dose at the usual time. If a dose of TYBOST with atazanavir or darunavir is skipped, the patient should not double the next dose of TYBOST with atazanavir or darunavir.
- Inform patients that renal impairment, including cases of acute renal failure and Fanconi syndrome, has been reported when TYBOST is used in combination with a tenofovir DF containing regimen.
- Inform patients that TYBOST may interact with many drugs with potential serious implications and that some drugs should not be taken with TYBOST. Patients should be advised to report to their healthcare provider the use of any other prescription or nonprescription medication or herbal products, including St. John's wort.
- Inform patients that if they must take acid modifying medications during treatment with TYBOST with atazanavir, the medications should be taken according to the following recommendations:
- an antacid medicine that contains aluminum or magnesium hydroxide: administer antacids at least 2 hours before or after TYBOST with atazanavir.
- H2-receptor antagonists (e.g., famotidine): administer either at the same time or take TYBOST with atazanavir a minimum of 10 hours after administering H2-receptor antagonists.
- Proton pump inhibitors (e.g.,omeprazole): take TYBOST with atazanavir a minimum of 12 hours after administering proton pump inhibitors.
Precautions with Alcohol
Alcohol-Cobicistat interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Tybost
Look-Alike Drug Names
There is limited information regarding Cobicistat Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
| File:Cobicistat.svg | |
| Clinical data | |
|---|---|
| ATC code | |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| ChEBI | |
| ChEMBL | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C40H53N7O5S2 |
| Molar mass | 776.023 g/mol |
| 3D model (JSmol) | |
| |
| |
| | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]; Associate Editor(s)-in-Chief: Alonso Alvarado, M.D. [4]
Overview
Cobicistat (formerly GS-9350) is a licensed drug for use in the treatment of infection with the human immunodeficiency virus (HIV).
Like ritonavir (Norvir), cobicistat is of interest for its ability to inhibit liver enzymes that metabolize other medications used to treat HIV, notably elvitegravir, an HIV integrase inhibitor. By combining cobicistat with elvitegravir, higher concentrations of the latter are achieved in the body with lower dosing, theoretically enhancing elvitegravir's viral suppression while diminishing its adverse side-effects. In contrast with ritonavir, the only other booster approved for use as a part of HAART, cobicistat has no anti-HIV activity of its own.[1]
Cobicistat is a component of the four-drug, fixed-dose combination HIV treatment elvitegravir/cobicistat/emtricitabine/tenofovir (marketed as Stribild, and also known as the "Quad Pill").[1][2] Stribild was approved by the FDA in August 2012 for use in the United States and is owned by Gilead Sciences.
Cobicistat is a potent inhibitor of cytochrome P450 3A enzymes, including the important CYP3A4 subtype. It also inhibits intestinal transport proteins, increasing the overall absorption of several HIV medications, including atazanavir, darunavir and tenofovir alafenamide fumarate.[3]
References
- ↑ 1.0 1.1 Highleyman, L. Elvitegravir "Quad" Single-tablet Regimen Shows Continued HIV Suppression at 48 Weeks. HIV and Hepatitis.com
- ↑ R Elion, J Gathe, B Rashbaum, and others. The Single-Tablet Regimen of Elvitegravir/Cobicistat/Emtricitabine/Tenofovir Disoproxil Fumarate (EVG/COBI/FTC/TDF; Quad) Maintains a High Rate of Virologic Suppression, and Cobicistat (COBI) is an Effective Pharmacoenhancer Through 48 Weeks. 50th Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC 2010). Boston, September 12–15, 2010.
- ↑ PMID 22850510 (PMID 22850510)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand
- Pages with script errors
- Pages with reference errors
- Pages with incomplete PMID references
- Pages with broken file links
- Articles with changed EBI identifier
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Drugs with no legal status
- Drugboxes which contain changes to verified fields
- Drugboxes which contain changes to watched fields