Chronic pancreatitis: Difference between revisions
Iqra Qamar (talk | contribs) No edit summary |
|||
| (42 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Infobox_Disease | {{Infobox_Disease | ||
| Name = | | Name = Chronic pancreatitis | ||
| Image = | | Image = Blausen 0699 PancreasAnatomy2.png | ||
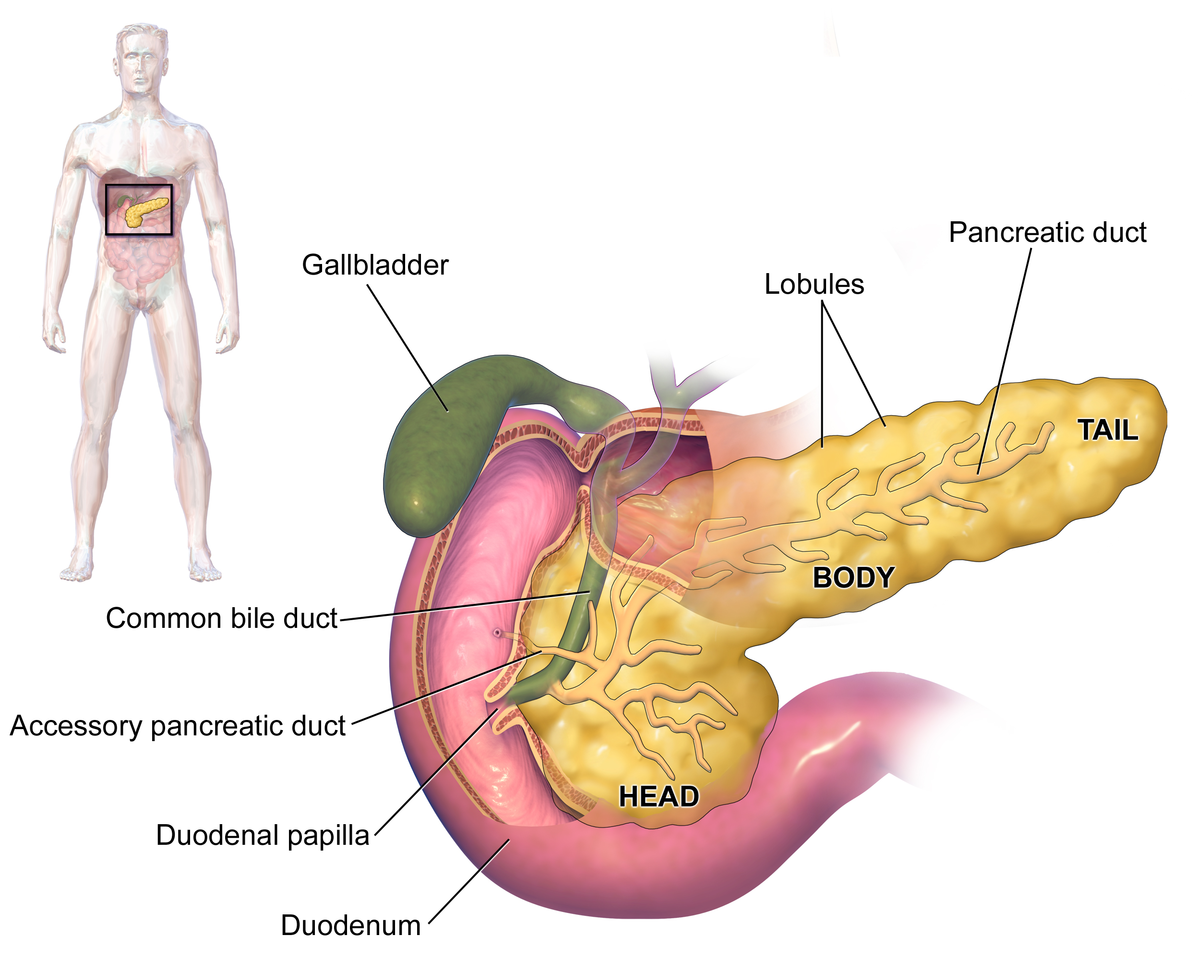
| Caption = | | Caption = Pancreas<ref><https://en.wikipedia.org/wiki/Pancreas#/media/File:Blausen_0699_PancreasAnatomy2.png></ref> | ||
}} | }} | ||
{{ | {{Chronic pancreatitis}} | ||
{{ | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | ||
'''For full discussion on Pancreatitis click [[Pancreatitis|here]].''' | |||
{{CMG}}, {{AE}}: {{IQ}} | |||
{{SK}} Pancreatitis, chronic; | |||
==[[Chronic pancreatitis overview|Overview]]== | |||
[[ | ==[[Chronic pancreatitis historical perspective|Historical Perspective]]== | ||
== | ==[[Chronic pancreatitis classification|Classification]]== | ||
==[[Chronic pancreatitis pathophysiology|Pathophysiology]]== | |||
==[[Chronic pancreatitis causes|Causes]]== | |||
==[[Chronic pancreatitis differential diagnosis|Differentiating Chronic pancreatitis from other Diseases]]== | |||
==[[Chronic pancreatitis epidemiology and demographics|Epidemiology and Demographics]]== | |||
==[[Chronic pancreatitis risk factors|Risk Factors]]== | |||
==[[Chronic pancreatitis screening|Screening]]== | |||
==[[Chronic pancreatitis natural history, complications and prognosis|Natural History, Complications and Prognosis]]== | |||
==Diagnosis== | ==Diagnosis== | ||
[[Chronic pancreatitis diagnostic study of choice|Diagnostic Study of Choice]] | [[Chronic pancreatitis history and symptoms|History and Symptoms ]] | [[ Chronic pancreatitis physical examination|Physical Examination]] | [[Chronic pancreatitis laboratory findings|Laboratory Findings]] | [[Chronic pancreatitis abdominal x ray|Abdominal X Ray]] | [[Chronic pancreatitis CT|CT]] | [[Chronic pancreatitis MRI|MRI]] | [[Chronic pancreatitis ultrasound|Ultrasound]] | [[Chronic pancreatitis other imaging findings|Other Imaging Findings]] | [[Chronic pancreatitis other diagnostic studies|Other Diagnostic Studies]] | |||
==Treatment== | |||
[[Chronic pancreatitis medical therapy|Medical Therapy]] | [[Chronic pancreatitis surgery |Surgery]] | [[Chronic pancreatitis primary prevention|Primary Prevention]] | [[Chronic pancreatitis secondary prevention|Secondary Prevention]] | [[Chronic pancreatitis cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Chronic pancreatitis future or investigational therapies|Future or Investigational Therapies]] | |||
==Case Studies== | |||
[[Chronic pancreatitis case study one|Case #1]] | |||
== Related Chapters == | |||
* [[Acute pancreatitis]] | |||
* [[Exocrine pancreatic insufficiency]] | |||
{{Gastroenterology}} | |||
[[Category:Gastroenterology]] | |||
[[Category:Surgery]] | |||
[[fr:Pancréatite chronique]] | |||
[[it:Pancreatite cronica]] | |||
[[pl:Przewlekłe zapalenie trzustki]] | |||
[[pt:Pancreatite crônica]] | |||
[[ru:Хронический панкреатит]] | |||
[[fi:Krooninen haimatulehdus]] | |||
[[tr:Kronik pankreatit]] | |||
Latest revision as of 16:03, 15 December 2017
| Chronic pancreatitis | |
 | |
|---|---|
| Pancreas[1] |
|
Chronic pancreatitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
American Pancreatic Association Practice Guidelines |
|
Chronic pancreatitis On the Web |
|
American Roentgen Ray Society Images of Chronic pancreatitis |
For patient information click here
For full discussion on Pancreatitis click here.
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Associate Editor(s)-in-Chief: : Iqra Qamar M.D.[2]
Synonyms and keywords: Pancreatitis, chronic;
Overview
Historical Perspective
Classification
Pathophysiology
Causes
Differentiating Chronic pancreatitis from other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications and Prognosis
Diagnosis
Diagnostic Study of Choice | History and Symptoms | Physical Examination | Laboratory Findings | Abdominal X Ray | CT | MRI | Ultrasound | Other Imaging Findings | Other Diagnostic Studies
Treatment
Medical Therapy | Surgery | Primary Prevention | Secondary Prevention | Cost-Effectiveness of Therapy | Future or Investigational Therapies
Case Studies
Related Chapters
Template:Gastroenterology it:Pancreatite cronica fi:Krooninen haimatulehdus