Cervical cancer pathophysiology: Difference between revisions
No edit summary |
|||
| Line 6: | Line 6: | ||
Cervical cancer arises at squamous-columnar junction. It could happen as a primary malignant tumor or as a metastasis from other tumors. | Cervical cancer arises at squamous-columnar junction. It could happen as a primary malignant tumor or as a metastasis from other tumors. | ||
==Pathogenesis | ==Pathophysiology== | ||
=== '''Pathogenesis:''' === | |||
* [[HPV|Human papillomaviruses]] subtypes 16 and 18 (High risk) play an essential role in the pathogenesis of cervical cancer. Once [[HPV]] enters an epithelial cell, the virus begins to make the proteins it encodes. Two of the proteins made by high-risk HPVs (E6 and E7) interfere with cell functions that normally prevent excessive growth, helping the cell to grow in an uncontrolled manner and to avoid cell death. Many times these infected cells are recognized by the immune system and eliminated. Sometimes, however, these infected cells are not destroyed, and a persistent infection results. As the persistently infected cells continue to grow, they may develop mutations in cellular genes that promote even more abnormal cell growth, leading to the formation of an area of precancerous cells and, ultimately, a cancerous tumor.<ref>http://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-fact-sheet</ref> | * [[HPV|Human papillomaviruses]] subtypes 16 and 18 (High risk) play an essential role in the pathogenesis of cervical cancer. Once [[HPV]] enters an epithelial cell, the virus begins to make the proteins it encodes. Two of the proteins made by high-risk HPVs (E6 and E7) interfere with cell functions that normally prevent excessive growth, helping the cell to grow in an uncontrolled manner and to avoid cell death. Many times these infected cells are recognized by the immune system and eliminated. Sometimes, however, these infected cells are not destroyed, and a persistent infection results. As the persistently infected cells continue to grow, they may develop mutations in cellular genes that promote even more abnormal cell growth, leading to the formation of an area of precancerous cells and, ultimately, a cancerous tumor.<ref>http://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-fact-sheet</ref> | ||
* Cervical carcinoma has its origins at the squamous-columnar junction; it can involve the outer squamous cells, the inner glandular cells, or both. The precursor lesion is [[dysplasia]]: [[cervical intraepithelial neoplasia]] (CIN) or adenocarcinoma in situ, which can subsequently become invasive cancer. This process can be quite slow. Longitudinal studies have shown that in patients with untreated in situ cervical cancer, 30% to 70% will develop invasive carcinoma over a period of 10 to 12 years. However, in about 10% of patients, lesions can progress from in situ to invasive in a period of less than 1 year. As it becomes invasive, the tumor breaks through the basement membrane and invades the cervical stroma. Extension of the tumor in the cervix may ultimately manifest as ulceration, exophytic tumor, or extensive infiltration of underlying tissue, including the bladder or rectum.<ref>http://www.cancer.gov/types/cervical/hp/cervical-treatment-pdq#link/_532_toc</ref> | * Cervical carcinoma has its origins at the squamous-columnar junction; it can involve the outer squamous cells, the inner glandular cells, or both. The precursor lesion is [[dysplasia]]: [[cervical intraepithelial neoplasia]] (CIN) or adenocarcinoma in situ, which can subsequently become invasive cancer. This process can be quite slow. Longitudinal studies have shown that in patients with untreated in situ cervical cancer, 30% to 70% will develop invasive carcinoma over a period of 10 to 12 years. However, in about 10% of patients, lesions can progress from in situ to invasive in a period of less than 1 year. As it becomes invasive, the tumor breaks through the basement membrane and invades the cervical stroma. Extension of the tumor in the cervix may ultimately manifest as ulceration, exophytic tumor, or extensive infiltration of underlying tissue, including the bladder or rectum.<ref>http://www.cancer.gov/types/cervical/hp/cervical-treatment-pdq#link/_532_toc</ref> | ||
Revision as of 14:22, 27 September 2018
|
Cervical cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cervical cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Cervical cancer pathophysiology |
|
Risk calculators and risk factors for Cervical cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]}Associate Editor(s)-in-Chief: Monalisa Dmello, M.B,B.S., M.D. [2] Aida Javanbakht, M.D.
Overview
Cervical cancer arises at squamous-columnar junction. It could happen as a primary malignant tumor or as a metastasis from other tumors.
Pathophysiology
Pathogenesis:
- Human papillomaviruses subtypes 16 and 18 (High risk) play an essential role in the pathogenesis of cervical cancer. Once HPV enters an epithelial cell, the virus begins to make the proteins it encodes. Two of the proteins made by high-risk HPVs (E6 and E7) interfere with cell functions that normally prevent excessive growth, helping the cell to grow in an uncontrolled manner and to avoid cell death. Many times these infected cells are recognized by the immune system and eliminated. Sometimes, however, these infected cells are not destroyed, and a persistent infection results. As the persistently infected cells continue to grow, they may develop mutations in cellular genes that promote even more abnormal cell growth, leading to the formation of an area of precancerous cells and, ultimately, a cancerous tumor.[1]
- Cervical carcinoma has its origins at the squamous-columnar junction; it can involve the outer squamous cells, the inner glandular cells, or both. The precursor lesion is dysplasia: cervical intraepithelial neoplasia (CIN) or adenocarcinoma in situ, which can subsequently become invasive cancer. This process can be quite slow. Longitudinal studies have shown that in patients with untreated in situ cervical cancer, 30% to 70% will develop invasive carcinoma over a period of 10 to 12 years. However, in about 10% of patients, lesions can progress from in situ to invasive in a period of less than 1 year. As it becomes invasive, the tumor breaks through the basement membrane and invades the cervical stroma. Extension of the tumor in the cervix may ultimately manifest as ulceration, exophytic tumor, or extensive infiltration of underlying tissue, including the bladder or rectum.[2]
Microscopic pathology
-
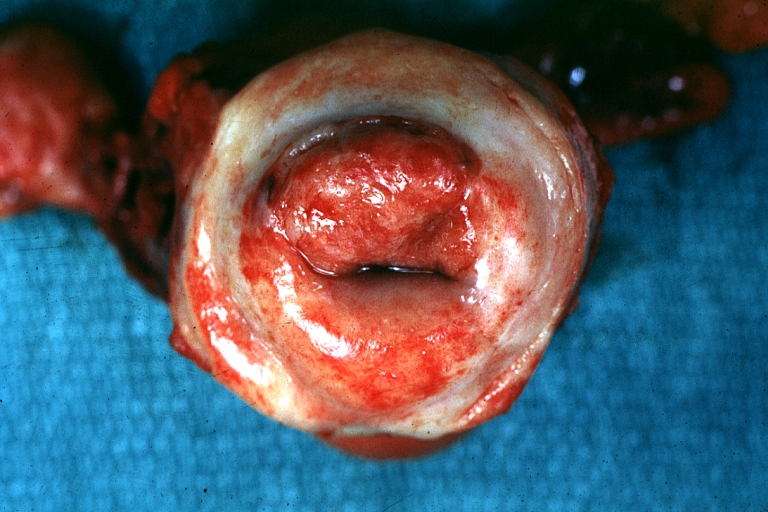
Uterus: Cervical Carcinoma: Gross, an excellent example of tumor (labeled as invasive)
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology -
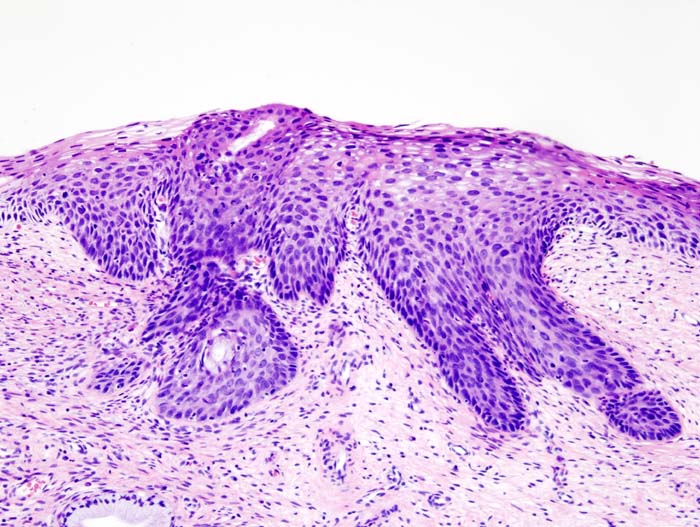
Histopathologic image (H&E stain) of cervical intraepithelial neoplasia.
Video
{{#ev:youtube|J3kULzKGzws}}