Caspofungin
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Caspofungin is {{{aOrAn}}} {{{drugClass}}} that is FDA approved for the {{{indicationType}}} of {{{indication}}}. Common adverse reactions include {{{adverseReactions}}}.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
CANCIDAS® is indicated in adults and pediatric patients (3 months and older) for:
- Empirical therapy for presumed fungal infections in febrile, neutropenic patients
- Treatment of candidemia and the following Candida infections: intra-abdominal abscesses, peritonitis and pleural space infections. CANCIDAS has not been studied in endocarditis, osteomyelitis, and meningitis due to Candida.
- Treatment of esophageal candidiasis.
- Treatment of invasive aspergillosis in patients who are refractory to or intolerant of other therapies (e.g., amphotericin B, lipid formulations of amphotericin B, itraconazole). CANCIDAS has not been studied as initial therapy for invasive aspergillosis.
Dosage
Recommended Dosing in Adult Patients [≥18 years of age]
- The usual dose is 50 mg once daily (following a 70-mg loading dose for most indications). The safety and efficacy of a dose of 150 mg daily (range: 1 to 51 days; median: 14 days) have been studied in 100 adult patients with candidemia and other Candida infections. The efficacy of CANCIDAS at this higher dose was not significantly better than the efficacy of the 50-mg daily dose of CANCIDAS. The efficacy of doses higher than 50 mg daily in the other adult patients for whom CANCIDAS is indicated is not known.
Empirical Therapy
A single 70-mg loading dose should be administered on Day 1, followed by 50 mg once daily thereafter. Duration of treatment should be based on the patient's clinical response. Empirical therapy should be continued until resolution of neutropenia. Patients found to have a fungal infection should be treated for a minimum of 14 days; treatment should continue for at least 7 days after both neutropenia and clinical symptoms are resolved. If the 50-mg dose is well tolerated but does not provide an adequate clinical response, the daily dose can be increased to 70 mg.
Candidemia and Other Candida Infections
A single 70-mg loading dose should be administered on Day 1, followed by 50 mg once daily thereafter. Duration of treatment should be dictated by the patient's clinical and microbiological response. In general, antifungal therapy should continue for at least 14 days after the last positive culture. Patients who remain persistently neutropenic may warrant a longer course of therapy pending resolution of the neutropenia.
Esophageal Candidiasis
The dose is 50 mg once daily for 7 to 14 days after symptom resolution. A 70-mg loading dose has not been studied for this indication. Because of the risk of relapse of oropharyngeal candidiasis in patients with HIV infections, suppressive oral therapy could be considered.
Invasive Aspergillosis
A single 70-mg loading dose should be administered on Day 1, followed by 50 mg once daily thereafter. Duration of treatment should be based upon the severity of the patient's underlying disease, recovery from immunosuppression, and clinical response.
Patients with Hepatic Impairment
Adult patients with mild hepatic impairment (Child-Pugh score 5 to 6) do not need a dosage adjustment. For adult patients with moderate hepatic impairment (Child-Pugh score 7 to 9), CANCIDAS 35 mg once daily is recommended based upon pharmacokinetic data. However, where recommended, a 70-mg loading dose should still be administered on Day 1. There is no clinical experience in adult patients with severe hepatic impairment (Child-Pugh score >9) and in pediatric patients with any degree of hepatic impairment.
Patients Receiving Concomitant Inducers of Drug Clearance
- Adult patients on rifampin should receive 70 mg of CANCIDAS once daily. Adult patients on nevirapine, efavirenz, carbamazepine, dexamethasone, or phenytoin may require an increase in dose to 70 mg of CANCIDAS once daily.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Caspofungin in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Caspofungin in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Recommended Dosing in Pediatric Patients [3 months to 17 years of age]
- For all indications, a single 70-mg/m2 loading dose should be administered on Day 1, followed by 50 mg/m2 once daily thereafter. The maximum loading dose and the daily maintenance dose should not exceed 70 mg, regardless of the patient's calculated dose. Dosing in pediatric patients (3 months to 17 years of age) should be based on the patient's body surface area (BSA) as calculated by the Mosteller Formula
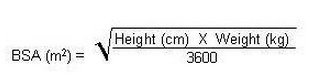
- Following calculation of the patient's BSA, the loading dose in milligrams should be calculated as BSA (m2) X 70 mg/m2. The maintenance dose in milligrams should be calculated as BSA (m2) X 50 mg/m2.
- Duration of treatment should be individualized to the indication, as described for each indication in adults. If the 50-mg/m2 daily dose is well tolerated but does not provide an adequate clinical response, the daily dose can be increased to 70 mg/m2 daily (not to exceed 70 mg).
Patients Receiving Concomitant Inducers of Drug Clearance
When CANCIDAS is co-administered to pediatric patients with inducers of drug clearance, such as rifampin, efavirenz, nevirapine, phenytoin, dexamethasone, or carbamazepine, a CANCIDAS dose of 70 mg/m2 once daily (not to exceed 70 mg) should be considered
Special Considerations for Pediatric Patients >3 Months of Age
- Follow the reconstitution procedures described above using either the 70-mg or 50-mg vial to create the reconstituted solution. From the reconstituted solution in the vial, remove the volume of drug equal to the calculated loading dose or calculated maintenance dose based on a concentration of 7 mg/mL (if reconstituted from the 70-mg vial) or a concentration of 5 mg/mL (if reconstituted from the 50-mg vial).
- The choice of vial should be based on total milligram dose of drug to be administered to the pediatric patient. To help ensure accurate dosing, it is recommended for pediatric doses less than 50 mg that 50-mg vials (with a concentration of 5 mg/mL) be used if available. The 70-mg vial should be reserved for pediatric patients requiring doses greater than 50 mg.
The maximum loading dose and the daily maintenance dose should not exceed 70 mg, regardless of the patient's calculated dose.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Caspofungin in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Caspofungin in pediatric patients.
Contraindications
CANCIDAS is contraindicated in patients with hypersensitivity (e.g., anaphylaxis) to any component of this product.
Warnings
Hypersensitivity
- Anaphylaxis has been reported during administration of CANCIDAS. If this occurs, CANCIDAS should be discontinued and appropriate treatment administered.
- Possible histamine-mediated adverse reactions, including rash, facial swelling, angioedema, pruritus, sensation of warmth or bronchospasm have been reported and may require discontinuation and/or administration of appropriate treatment.
Concomitant Use with Cyclosporine
- Concomitant use of CANCIDAS with cyclosporine should be limited to patients for whom the potential benefit outweighs the potential risk. In one clinical study, 3 of 4 healthy adult subjects who received CANCIDAS 70 mg on Days 1 through 10, and also received two 3 mg/kg doses of cyclosporine 12 hours apart on day 10, developed transient elevations of alanine transaminase (ALT) on day 11 that were 2 to 3 times the upper limit of normal (ULN). In a separate panel of adult subjects in the same study, 2 of 8 who received CANCIDAS 35 mg daily for 3 days and cyclosporine (two 3 mg/kg doses administered 12 hours apart) on day 1 had small increases in ALT (slightly above the ULN) on day 2. In both groups, elevations in aspartate transaminase (AST) paralleled ALT elevations, but were of lesser magnitude. In another clinical study, 2 of 8 healthy men developed transient ALT elevations of less than 2X ULN. In this study, cyclosporine (4 mg/kg) was administered on Days 1 and 12, and CANCIDAS was administered (70 mg) daily on Days 3 through 13. In one subject, the ALT elevation occurred on days 7 and 9 and, in the other subject, the ALT elevation occurred on Day 19. These elevations returned to normal by Day 27. In all groups, elevations in AST paralleled ALT elevations but were of lesser magnitude. In these clinical studies, cyclosporine (one 4 mg/kg dose or two 3 mg/kg doses) increased the AUC of caspofungin by approximately 35%.
- In a retrospective postmarketing study, 40 immunocompromised patients, including 37 transplant recipients, were treated with CANCIDAS and cyclosporine for 1 to 290 days (median 17.5 days). Fourteen patients (35%) developed transaminase elevations >5X upper limit of normal or >3X baseline during concomitant therapy or the 14-day follow-up period; five were considered possibly related to concomitant therapy. One patient had elevated bilirubin considered possibly related to concomitant therapy. No patient developed clinical evidence of hepatotoxicity or serious hepatic events. Discontinuations due to laboratory abnormalities in hepatic enzymes from any cause occurred in four patients. Of these, 2 were considered possibly related to therapy with CANCIDAS and/or cyclosporine as well as to other possible causes.
- In the prospective invasive aspergillosis and compassionate use studies, there were 4 adult patients treated with CANCIDAS (50 mg/day) and cyclosporine for 2 to 56 days. None of these patients experienced increases in hepatic enzymes.
- Given the limitations of these data, CANCIDAS and cyclosporine should only be used concomitantly in those patients for whom the potential benefit outweighs the potential risk. Patients who develop abnormal liver function tests during concomitant therapy should be monitored and the risk/benefit of continuing therapy should be evaluated.
Hepatic Effects
- Laboratory abnormalities in liver function tests have been seen in healthy volunteers and in adult and pediatric patients treated with CANCIDAS. In some adult and pediatric patients with serious underlying conditions who were receiving multiple concomitant medications with CANCIDAS, isolated cases of clinically significant hepatic dysfunction, hepatitis, and hepatic failure have been reported; a causal relationship to CANCIDAS has not been established.
- Patients who develop abnormal liver function tests during CANCIDAS therapy should be monitored for evidence of worsening hepatic function and evaluated for risk/benefit of continuing CANCIDAS therapy
Adverse Reactions
Clinical Trials Experience
- The following serious adverse reactions are discussed in detail in another section of the labeling:
- Hepatic effects
- Hypersensitivity
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of CANCIDAS cannot be directly compared to rates in clinical trials of another drug and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does provide a basis for identifying adverse reactions that appear to be related to drug use and for approximating rates.
Clinical Trials Experience in Adults
The overall safety of CANCIDAS was assessed in 1865 adult individuals who received single or multiple doses of CANCIDAS: 564 febrile, neutropenic patients (empirical therapy study); 382 patients with candidemia and/or intra-abdominal abscesses, peritonitis, or pleural space infections (including 4 patients with chronic disseminated candidiasis); 297 patients with esophageal and/or oropharyngeal candidiasis; 228 patients with invasive aspergillosis; and 394 individuals in phase I studies. In the empirical therapy study patients had undergone hematopoietic stem-cell transplantation or chemotherapy. In the studies involving patients with documented Candida infections, the majority of the patients had serious underlying medical conditions (e.g., hematologic or other malignancy, recent major surgery, HIV) requiring multiple concomitant medications. Patients in the noncomparative Aspergillus studies often had serious predisposing medical conditions (e.g., bone marrow or peripheral stem cell transplants, hematologic malignancy, solid tumors or organ transplants) requiring multiple concomitant medications.
Empirical Therapy
- In the randomized, double-blinded empirical therapy study, patients received either CANCIDAS 50 mg/day (following a 70-mg loading dose) or AmBisome® (amphotericin B liposome for injection, 3 mg/kg/day). In this study clinical or laboratory hepatic adverse reactions were reported in 39% and 45% of patients in the CANCIDAS and AmBisome groups, respectively. Also reported was an isolated, serious adverse reaction of hyperbilirubinemia considered possibly related to CANCIDAS. Adverse reactions occurring in ≥7.5% of the patients in either treatment group are presented in Table 2

- The proportion of patients who experienced an infusion-related adverse reaction (defined as a systemic event, such as pyrexia, chills, flushing, hypotension, hypertension, tachycardia, dyspnea, tachypnea, rash, or anaphylaxis, that developed during the study therapy infusion and one hour following infusion) was significantly lower in the group treated with CANCIDAS (35%) than in the group treated with AmBisome (52%).
- To evaluate the effect of CANCIDAS and AmBisome on renal function, nephrotoxicity was defined as doubling of serum creatinine relative to baseline or an increase of ≥1 mg/dL in serum creatinine if baseline serum creatinine was above the upper limit of the normal range. Among patients whose baseline creatinine clearance was >30 mL/min, the incidence of nephrotoxicity was significantly lower in the group treated with CANCIDAS (3%) than in the group treated with AmBisome (12%). Clinical renal events, regardless of causality, were similar between CANCIDAS (75/564, 13%) and AmBisome (85/547, 16%).
Candidemia and Other Candida Infections
- In the randomized, double-blinded invasive candidiasis study, patients received either CANCIDAS 50 mg/day (following a 70-mg loading dose) or amphotericin B 0.6 to 1 mg/kg/day. Adverse reactions occurring in ≥10% of the patients in either treatment group are presented in Table 3.

- The proportion of patients who experienced an infusion-related adverse reaction (defined as a systemic event, such as pyrexia, chills, flushing, hypotension, hypertension, tachycardia, dyspnea, tachypnea, rash, or anaphylaxis, that developed during the study therapy infusion and one hour following infusion) was significantly lower in the group treated with CANCIDAS (20%) than in the group treated with amphotericin B (49%).
- To evaluate the effect of CANCIDAS and amphotericin B on renal function, nephrotoxicity was defined as doubling of serum creatinine relative to baseline or an increase of ≥1 mg/dL in serum creatinine if baseline serum creatinine was above the upper limit of the normal range. In a subgroup of patients whose baseline creatinine clearance was >30 mL/min, the incidence of nephrotoxicity was significantly lower in the group treated with CANCIDAS than in the group treated with amphotericin B.
- In a second randomized, double-blinded invasive candidiasis study, patients received either CANCIDAS 50 mg/day (following a 70-mg loading dose) or CANCIDAS 150 mg/day. The proportion of patients who experienced any adverse reaction was similar in the 2 treatment groups; however, this study was not large enough to detect differences in rare or unexpected adverse events. Adverse reactions occurring in ≥5% of the patients in either treatment group are presented in Table 4.
Postmarketing Experience
There is limited information regarding Caspofungin Postmarketing Experience in the drug label.
Drug Interactions
There is limited information regarding Caspofungin Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
There is no FDA guidance on usage of Caspofungin in women who are pregnant.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Caspofungin in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Caspofungin during labor and delivery.
Nursing Mothers
There is no FDA guidance on the use of Caspofungin in women who are nursing.
Pediatric Use
There is no FDA guidance on the use of Caspofungin in pediatric settings.
Geriatic Use
There is no FDA guidance on the use of Caspofungin in geriatric settings.
Gender
There is no FDA guidance on the use of Caspofungin with respect to specific gender populations.
Race
There is no FDA guidance on the use of Caspofungin with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Caspofungin in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Caspofungin in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Caspofungin in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Caspofungin in patients who are immunocompromised.
Administration and Monitoring
Administration
Instructions for Use in All Patients
- CANCIDAS should be administered by slow intravenous (IV) infusion over approximately 1 hour. CANCIDAS should not be administered by IV bolus administration.
- Do not mix or co-infuse CANCIDAS with other medications, as there are no data available on the compatibility of CANCIDAS with other intravenous substances, additives, or medications. DO NOT USE DILUENTS CONTAINING DEXTROSE (α-D-GLUCOSE), as CANCIDAS is not stable in diluents containing dextrose.
Monitoring
There is limited information regarding Caspofungin Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Caspofungin and IV administrations.
Overdosage
There is limited information regarding Caspofungin overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
There is limited information regarding Caspofungin Pharmacology in the drug label.
Mechanism of Action
There is limited information regarding Caspofungin Mechanism of Action in the drug label.
Structure
There is limited information regarding Caspofungin Structure in the drug label.
Pharmacodynamics
There is limited information regarding Caspofungin Pharmacodynamics in the drug label.
Pharmacokinetics
There is limited information regarding Caspofungin Pharmacokinetics in the drug label.
Nonclinical Toxicology
There is limited information regarding Caspofungin Nonclinical Toxicology in the drug label.
Clinical Studies
There is limited information regarding Caspofungin Clinical Studies in the drug label.
How Supplied
There is limited information regarding Caspofungin How Supplied in the drug label.
Storage
There is limited information regarding Caspofungin Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Caspofungin |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Caspofungin |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Caspofungin Patient Counseling Information in the drug label.
Precautions with Alcohol
Alcohol-Caspofungin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Caspofungin Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Caspofungin Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]; Associate Editor(s)-in-Chief: Ahmed Zaghw, M.D. [4]
Overview
Caspofungin (INN[1]) (brand name Cancidas worldwide) is a lipopeptide antifungal drug from Merck & Co., Inc.. It is a member of a new class of antifungals termed the echinocandins. It works by inhibiting the enzyme (1→3)-β-D-glucan synthase and thereby disturbing the integrity of the fungal cell wall. Caspofungin was the first inhibitor of fungal (1→3)-β-D-glucan synthesis to be approved by the United States Food and Drug Administration.[2] Caspofungin is administered intravenously.
Category
Antifungal
US Brand Names
CANCIDAS®
FDA Package Insert
Description | Clinical Pharmacology | Microbiology | Indications and Usage | Contraindications | Warnings and Precautions | Adverse Reactions | Drug Interactions | Overdosage | Clinical Studies | Dosage and Administration | How Supplied | Labels and Packages
Mechanism of Action
References
- ↑ European Medicines Agency's list of authorised medicines for human use (C)
- ↑ Deresinski SC; Stevens DA (2003). "Caspofungin". Clin Infect Dis. 36 (11): 1445&ndash, 1457. doi:10.1086/375080. PMID 12766841. Unknown parameter
|author-separator=ignored (help)