Candida vulvovaginitis
| Candidiasis | |
 | |
|---|---|
| Agar plate culture of Candida albicans | |
| ICD-10 | B37 |
| ICD-9 | 112 |
| DiseasesDB | 1929 |
| MedlinePlus | 001511 |
| eMedicine | med/264 emerg/76 ped/312 derm/67 |
| MeSH | D002177 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Candidiasis, commonly called yeast infection or thrush, is a fungal infection (mycosis) of any of the Candida species, of which Candida albicans is the most common.[1][2] Candidiasis thereby encompasses infections that range from superficial, such as oral thrush and vaginitis, to systemic and potentially life-threatening diseases. Candida infections of the latter category are also referred to as candidemia and are usually confined to severely immunocompromised persons, such as cancer, transplant, and AIDS patients, whereas superficial infections of skin and mucosal membranes by Candida causing local inflammation and discomfort is common in many human populations.[2][3][4] While clearly attributable to the presence of the opportunistic pathogens of the genus Candida, candidiasis describes a number of different disease syndromes that often differ in their causes and outcomes.[2][3]
History and taxonomic classification
B. Lagenbeck in 1839 in Germany was the first to demonstrate that a yeast-like fungus existed in the human oral infection "thrush." He also found that a fungus was able to cause thrush.
The genera Candida, species albicans was described by botanist Christine Marie Berkhout. She described the fungus in her doctoral thesis, at the University of Utrecht in 1923. Over the years the classification of the genera and species has evolved. Obsolete names for this genus include Mycotorula and Torulopsis. The species has also been known in the past as Monilia albicans and Oidium albicans. The current classification is nomen conservandum, which means the name is authorized for use by the International Botanical Congress (IBC).
The full current taxonomic classification is available at Candida albicans.
The genus Candida includes about 150 different species. However, only a few of those are known to cause human infections. C. albicans is the most significant pathogenic (=disease-causing) species. Other Candida species causing diseases in humans include C. tropicalis, C. glabrata, C. krusei, C. parapsilosis, C. dubliniensis, and C. lusitaniae.
Manifestation
In immunocompetent people, candidiasis can usually only be found in exposed and moist parts of the body[1], such as:
- the oral cavity (oral thrush)
- the vagina and/or vulva (vaginal candidiasis or thrush)
- folds of skin in the diaper area (diaper rash)
- the nipples while breastfeeding
- the penis or foreskin
- the armpit
- the ear
- the skin around the nostrils or in the nostrils
Candidiasis is the second most common cause of vaginal irritation, or vaginitis, and can also occur on the male genitals. In immunocompromised patients, the Candida infection can involve the esophagus and can become systemic, causing a much more serious condition: fungemia. [4][3]
Children, mostly between the ages of 3 and 9 years, can be affected by chronic mouth yeast infections, normally seen around the mouth as white patches. However, this is not a common condition.
Causes
Candida yeasts are usually present in most people, but uncontrolled multiplication resulting in disease symptoms is kept in check by other naturally occurring microorganisms, e.g., bacteria co-existing with the yeasts in the same locations, and by the human immune system.
In a study of 1009 women in New Zealand, the fungus, Candida albicans, was isolated from the vaginas of 19% of apparently healthy women. Carriers experienced few or no symptoms. However, external use of irritants (such as some detergents or douches) or internal disturbances (hormonal or physiological) can perturb the normal flora, constituting lactic acid bacteria, such as lactobacilli, and an overgrowth of yeast can result in noticeable symptoms. Pregnancy, the use of oral contraceptives, engaging in vaginal sex immediately and without cleansing after anal sex, and using lubricants containing glycerin have been found to be causally related to yeast infections. Diabetes mellitus and the use of antibiotics are also linked to an increased incidence of yeast infections. Candidiasis can be sexually transmitted from men to women, but not from a woman to a man. Diet has been found to be the cause in some animals. Hormone Replacement Therapy and infertility treatments may also be predisposing factors.
Symptoms
Symptoms include severe itching, burning, and soreness, irritation of the vagina and/or vulva, and a whitish or whitish-gray discharge, often with a curd-like appearance.
Many women mistake the symptoms of the more common bacterial vaginosis for a yeast infection. In a 2002 study published in the Journal of Obstetrics and Gynecology, only 33 percent of women who were self treating for a yeast infection actually had a yeast infection. Instead they had either bacterial vaginosis or a mixed-type infection.
In men, symptoms include red patchy sores near the head of the penis or on the foreskin. The sores may feel irritated and itchy, and sometimes they will burn as well.
Pathological Findings
Gross Images
-
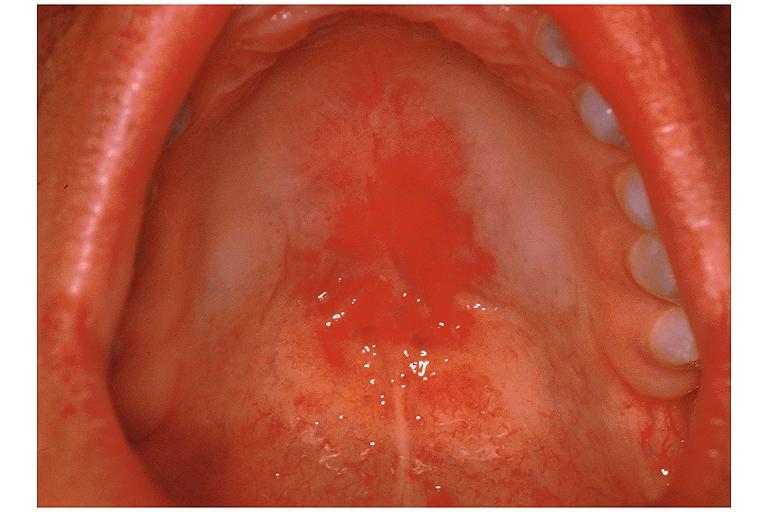
Oral manifestations of HIV infection and AIDS. Chronic oral candidiasis in patient with AIDS. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Soft palate showing extensive oral candidiasis in patient with AIDS. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Oral candidiasis Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
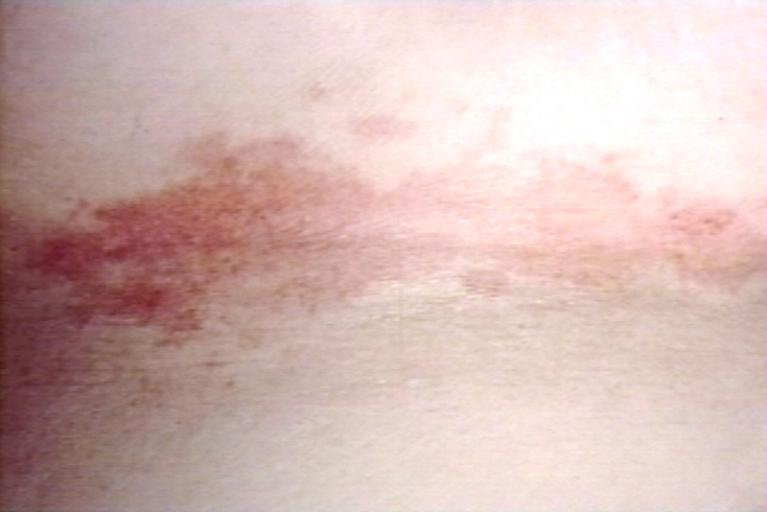
Eczema secondary to candidiasis. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Candidiasis; skinfold. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Erythematous candidiasis. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Genital candidiasis. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Paronychia: Another manifestation of candidiasis. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Interdigital candidiasis. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Candidiasis of umblical cord. White spots of colonies are present. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
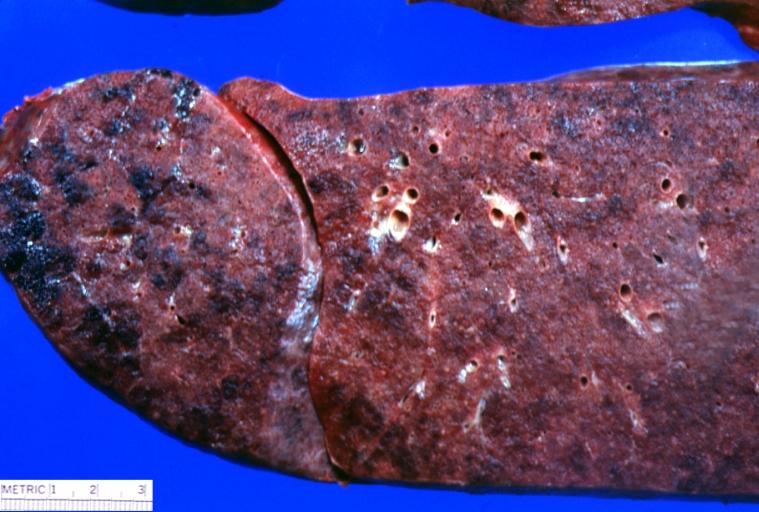
Lung: Candidiasis. Postmortem findings. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
Histopathology
Candidiasis of Esophagus & Colon
<youtube v=-E-HwjCm2h8/>
Diagnosis
Medical professionals use two primary methods to diagnose yeast infections: microscopic examination, and culturing.
For the microscope method, a scraping or swab of the affected area is placed on a microscope slide. A single drop of 10% potassium hydroxide (KOH) solution is then also placed on the slide. The KOH dissolves the skin cells but leaves the Candida untouched, so that when the slide is viewed under a microscope, the hyphae and pseudo spores of Candida are visible. Their presence in large numbers strongly suggests a yeast infection.
For the culturing method, a sterile swab is rubbed on the infected skin surface. The swab is then rubbed across a culture medium. The medium is incubated for several days, during which time colonies of yeast and/or bacteria develop. The characteristics of the colonies provide a presumptive diagnosis of the organism causing symptoms.
Treatment
It is important to consider that Candida species are frequently part of the human body's normal oral and intestinal flora. Candidiasis is occasionally misdiagnosed by medical personnel as bacterial in nature, and treated with antibiotics against bacteria. This can lead to eliminating the yeast's natural competitors for resources, and increase the severity of the condition.
In clinical settings, candidiasis is commonly treated with antimycotics - the antifungal drugs commonly used to treat candidiasis are topical clotrimazole, topical nystatin, fluconazole, and topical ketoconazole. In severe infections (generally in hospitalized patients), amphotericin B, caspofungin, or voriconazole may be used. Local treatment may include vaginal suppositories or medicated douches. Gentian violet can be used for breastfeeding thrush, but pediatrician recommends using it sparingly, since in large quantities it can cause mouth and throat ulcerations in nursing babies, and has been linked to mouth cancer in humans and to cancer in the digestive tract of other animals. [5]
One of the most potent nondrug or natural yeast-fighting substances is caprylic acid, a medium-chain fatty acid derived from coconut oil. Caprylic acid in capsule form is commonly sold as a dietary supplement in health food stores. It is very effective against Candida and other forms of fungi. It is even effective mixed with a little coconut oil or vitamin E oil as a topical application for fungal skin infections. Some cases of fungal infections that have lasted for months clear up in a matter of days using caprylic acid and a little coconut oil. It works just as effectively inside the body, killing fungi without the least bit of harm.
Polynesian women who eat their traditional coconut-based diet rarely, if ever, get yeast infections. Only in more temperate climates where processed vegetable oils are the main source of dietary fat are yeast infections, skin fungus, acne, and other skin infections big problems. Lauric acid, found in coconut oil, kills lipid-coated bacteria but does not appear to harm the friendly intestinal bacteria. Medium-Chain Fatty Acids (MCFA)s also have antifungal properties, so not only will they kill disease-causing bacteria and leave good bacteria alone but also they will kill Candida and other fungi in the intestinal tract, further supporting a healthy intestinal environment. Eating coconut oil on a regular basis, as the Polynesians do, helps to keep Candida and other harmful microorganisms at bay.
Some home remedies for candidiasis include the consumption or direct application of yogurt (which contains lactobacillus), probiotics, acidophilus tablets or salves, Pau d'arco tea, and even lightly crushed cloves of garlic, which yield allicin, an antifungal agent. Boric acid has also been used to treat yeast infections (by inserting gelcaps filled with boric acid powder into the vagina at bedtime for three to four consecutive nights). Eating a diet consisting primarily of green, fresh, raw vegetables also may give relief. Other alternative treatments consist in consuming a fermented beverage called Kefir.
While home remedies may offer relief in minor cases of infection (although a peer-reviewed study in Australia found yogurt ineffective as treatment for Candida albicans), seeking medical attention may be necessary, especially if the extent of the infection cannot be judged accurately by the patient. For instance, oral thrush is visible only at the upper digestive tract, but it may be that the lower digestive tract is likewise colonized by Candida species.
Treating candidiasis solely with medication may not give desired results, and other underlying causes require consideration. As an example, oral candidiasis is often linked to the use of inhaled corticosteroids in asthma medication. Patients on long-term inhaled corticosteroids should rinse their mouths after each dose of steroids to counteract this effect. Oral candidiasis can also be the sign of a more serious condition, such as HIV infection, or other immunodeficiency diseases. Following the health tips at vulvovaginal health can help prevent vaginal candidiasis.
Babies with diaper rash should have their diaper areas kept clean, dry, and exposed to air as much as possible. Sugars assist the overgrowth of yeast, possibly explaining the increased prevalence of yeast infections in patients with diabetes mellitus, as noted above. As many Candida spp. reside in the digestive tract, dietary changes may be effective for preventing or during a Candida infection. Due to its requirement for readily fermentable carbon sources, such as mono- or dimeric sugars (e.g., sucrose, glucose, lactose) and starch, avoiding foods that contain these nutrients in high abundance may help to prevent excessive Candida growth. Breast milk is a suitable growth substrate for yeasts, and both nursing mother and baby need to be treated (even if both are not symptomatic) to prevent thrush from being passed between mother and child. [6]
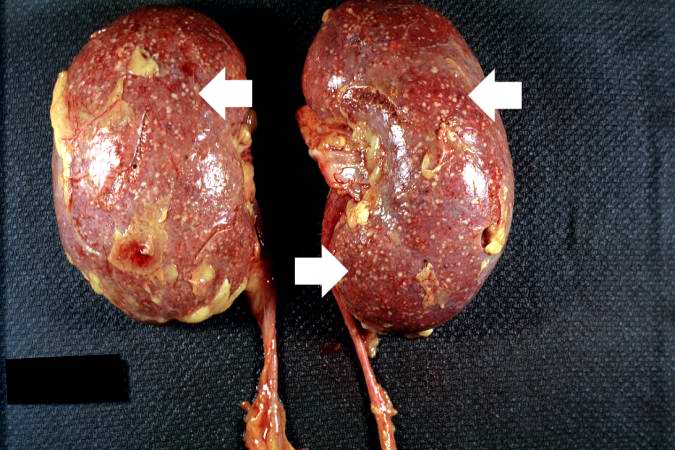
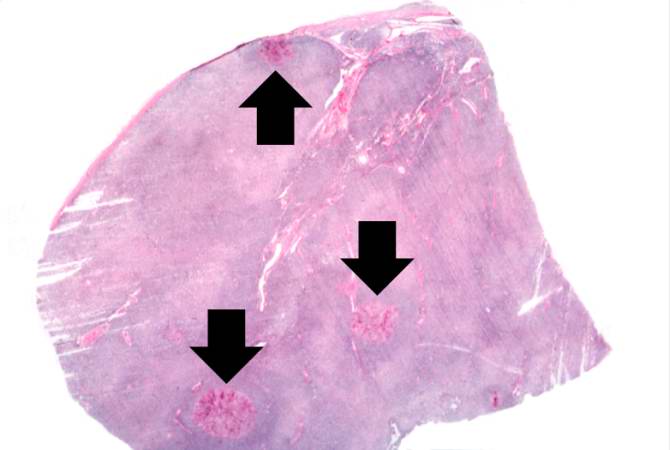
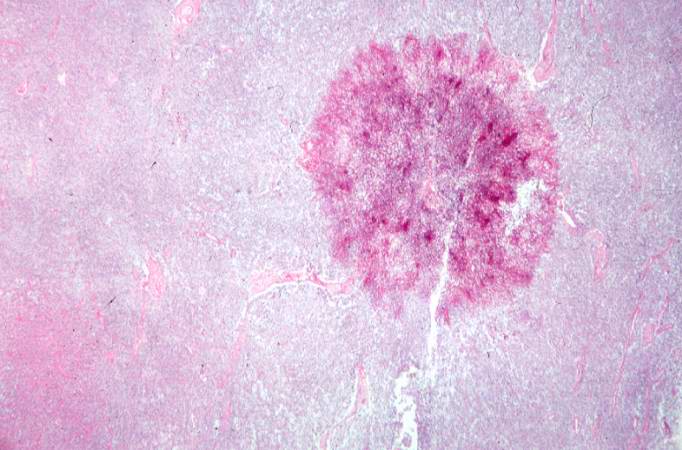
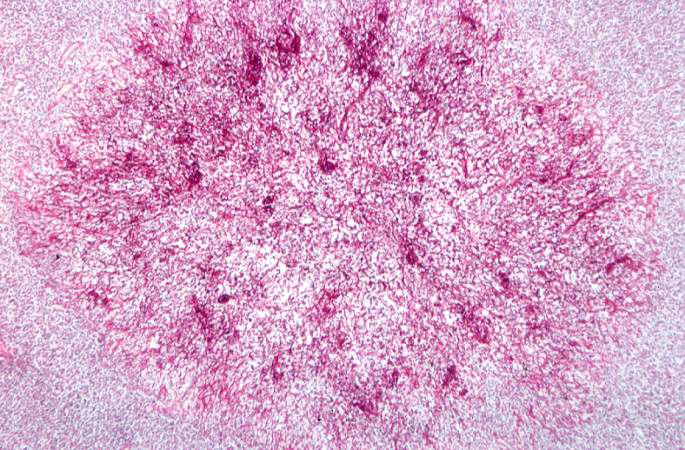
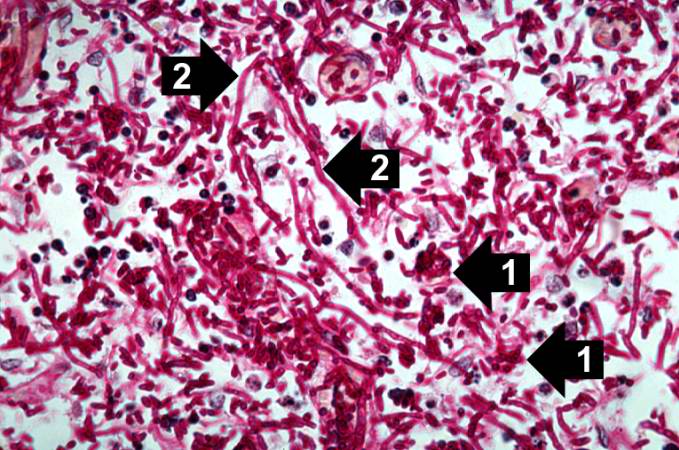
Case Example: Renal Candidiasis
Clinical Summary
A 73-year-old black male was in good health until about three months before his death when he noticed enlarged lymph nodes first in both inguinal regions and later elsewhere. Antileukemic therapy was begun. About two weeks prior to his death the patient presented to the emergency room with uncontrollable epistaxis. On physical examination, the liver was palpable but the spleen was not. The white blood count was below normal and consisted mainly of lymphocytes with many atypical cells. The patient's bone marrow was also found to be heavily loaded with lymphocytes. Platelets were extremely low and remained so despite platelet transfusions. Subsequently, the patient developed pneumonia which progressed until death. Antemortem cultures yielded Candida tropicalis and Pseudomonas aeruginosa.
Autopsy Findings
At autopsy, there was evidence of disseminated candidiasis.
Histopathological Findings



References
- ↑ 1.0 1.1 Walsh TJ, Dixon DM (1996). "Deep Mycoses". In Baron S et al eds. Baron's Medical Microbiology (via NCBI Bookshelf) (4th ed. ed.). Univ of Texas Medical Branch. ISBN 0-9631172-1-1.
- ↑ 2.0 2.1 2.2 MedlinePlus Encyclopedia Vaginal yeast infection
- ↑ 3.0 3.1 3.2 Fidel PL (2002). "Immunity to Candida". Oral Dis. 8: 69–75. PMID 12164664.
- ↑ 4.0 4.1 Pappas PG (2006). "Invasive candidiasis". Infect. Dis. Clin. North Am. 20 (3): 485–506. doi:10.1016/j.idc.2006.07.004. PMID 16984866.
- ↑ extoxnet.orst.edu
- ↑ PubMed Central Article
External links
- National Institute of Allergies and Infections (June 27, 2007). "Vaginitis". Retrieved 2008-02-21. - fact sheet on vaginitis/vaginal infections
- Oral Thrush Mayo Clinic
- DermAtlas candidiasis images
- InteliHealth page on candidiasis Presented by InteliHealth reviewed by Harvard Medical School
- Links to pictures of Yeast Infection (Hardin MD/Univ of Iowa)
- "Yeast Infections". VaginaPagina. - info on treatments
See Also