COVID-19-associated headache
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Fahimeh Shojaei, M.D.
Synonyms and keywords:
Overview
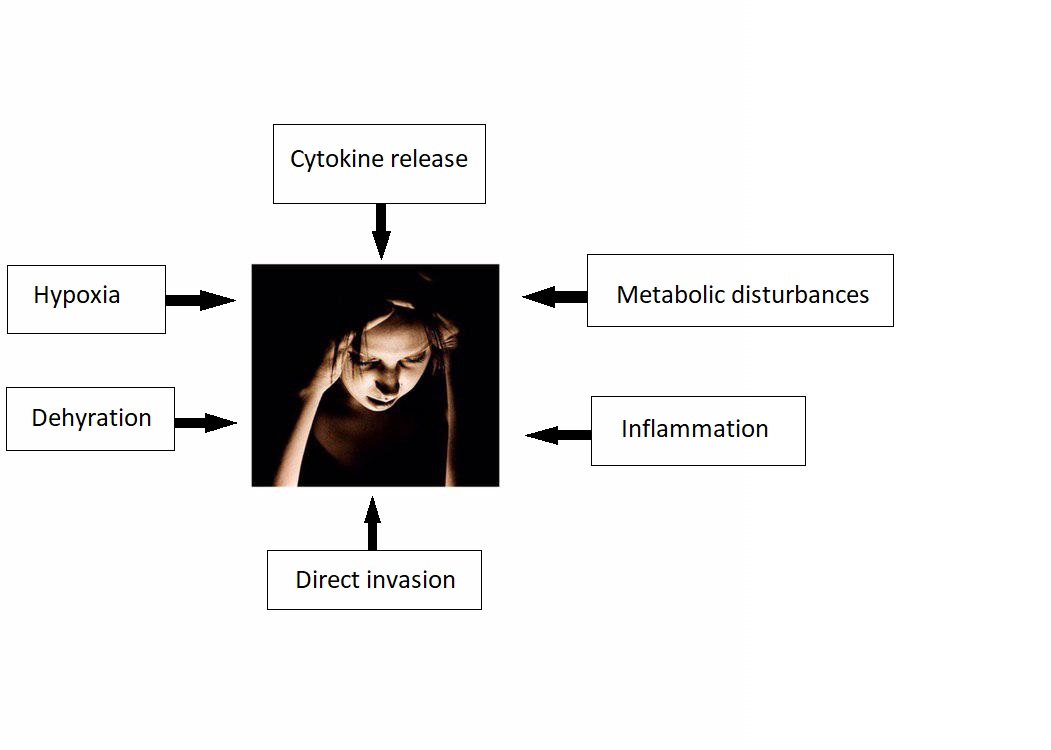
The association between COVID-19 and headache was made in 2020. COVID-19 associated headache may be caused by SARS-CoV-2 virus. There is no established system for the classification of COVID-19 associated headache. The exact pathogenesis of headache in COVID 19 patients is not fully understood. It is thought that headache is the result of cytokine release, direct invasion, metabolic disturbances, inflammation, dehydration, and hypoxia.
Historical Perspective
- The association between COVID-19 and headache was made in 2020.
Classification
- There is no established system for the classification of COVID-19 associated headache.
Pathophysiology
- The exact pathogenesis of headache in COVID 19 patients is not fully understood.
- It is thought that headache is the result of:[1][2][3][4]
- Cytokine release
- There is higher concentration on IL-6 and INF-gamma in patients infected with SARS/ CoV2.
- Cytokines can disrupt blood brain barrier and cause tissue injury and cerebral edema.
- Direct invasion
- Metabolic disturbances
- Inflammation
- Dehydration
- Hypoxia
- Cytokine release
Causes
- COVID-19 associated headache may be caused by SARS-CoV-2 virus.
Differentiating COVID-19-associated headache from other Diseases
COVID-19-associated headache must be differentiated from other diseases that cause headache, such as: [5][6][7][8][9][10][11][12][13][14][15][16][17][18][19][20][21][22][23]
- Migraine
- Tension-type headache
- Cluster headache
- Seizure
- Meningitis
- Encephalitis
- Neurosyphilis
- SAH
- Subdural hematoma
- Brain tumor
- Hypertensive encephalopathy
- Brain abscess
- Hemorrhagic stroke
- Wernickes encephalopathy
- Drug toxicity
Epidemiology and Demographics
The incidence/prevalence of [disease name] is approximately [number range] per 100,000 individuals worldwide.
OR
In [year], the incidence/prevalence of [disease name] was estimated to be [number range] cases per 100,000 individuals worldwide.
OR
In [year], the incidence of [disease name] is approximately [number range] per 100,000 individuals with a case-fatality rate of [number range]%.
Patients of all age groups may develop [disease name].
OR
The incidence of [disease name] increases with age; the median age at diagnosis is [#] years.
OR
[Disease name] commonly affects individuals younger than/older than [number of years] years of age.
OR
[Chronic disease name] is usually first diagnosed among [age group].
OR
[Acute disease name] commonly affects [age group].
There is no racial predilection to [disease name].
OR
[Disease name] usually affects individuals of the [race 1] race. [Race 2] individuals are less likely to develop [disease name].
[Disease name] affects men and women equally.
OR
[Gender 1] are more commonly affected by [disease name] than [gender 2]. The [gender 1] to [gender 2] ratio is approximately [number > 1] to 1.
The majority of [disease name] cases are reported in [geographical region].
OR
[Disease name] is a common/rare disease that tends to affect [patient population 1] and [patient population 2].
Risk Factors
- There are no established risk factors for COVID-19-associated headache.
Screening
- There is insufficient evidence to recommend routine screening for COVID-19 associated headache.
Natural History, Complications, and Prognosis
If left untreated, [#]% of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
OR
Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
OR
Prognosis is generally excellent/good/poor, and the 1/5/10-year mortality/survival rate of patients with [disease name] is approximately [#]%.
Diagnosis
Diagnostic Study of Choice
- The diagnosis of COVID-19-associated headache is based on the clinical presentation
- There are no established criteria for the diagnosis of COVID-19-associated headache.
History and Symptoms
- The hallmark of COVID-19-associated headache is headache.
- A positive history of fever and cough in addition to headache is suggestive of COVID-19-associated headache.
Physical Examination
- Patients with COVID-19-associated headache usually appear normal. Physical examination of patients with COVID-19-associated headache is usually remarkable for fever, cough, and malaise.
Laboratory Findings
An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name].
OR
Laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
OR
[Test] is usually normal among patients with [disease name].
OR
Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication].
OR
There are no diagnostic laboratory findings associated with [disease name].
Electrocardiogram
There are no ECG findings associated with [disease name].
OR
An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
X-ray
There are no x-ray findings associated with [disease name].
OR
An x-ray may be helpful in the diagnosis of [disease name]. Findings on an x-ray suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no x-ray findings associated with [disease name]. However, an x-ray may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with [disease name].
OR
Echocardiography/ultrasound may be helpful in the diagnosis of [disease name]. Findings on an echocardiography/ultrasound suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no echocardiography/ultrasound findings associated with [disease name]. However, an echocardiography/ultrasound may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
CT scan
There are no CT scan findings associated with [disease name].
OR
[Location] CT scan may be helpful in the diagnosis of [disease name]. Findings on CT scan suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no CT scan findings associated with [disease name]. However, a CT scan may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
MRI
There are no MRI findings associated with [disease name].
OR
[Location] MRI may be helpful in the diagnosis of [disease name]. Findings on MRI suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no MRI findings associated with [disease name]. However, a MRI may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Other Imaging Findings
There are no other imaging findings associated with [disease name].
OR
[Imaging modality] may be helpful in the diagnosis of [disease name]. Findings on an [imaging modality] suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
There are no other diagnostic studies associated with [disease name].
OR
[Diagnostic study] may be helpful in the diagnosis of [disease name]. Findings suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
There is no treatment for [disease name]; the mainstay of therapy is supportive care.
OR
Supportive therapy for [disease name] includes [therapy 1], [therapy 2], and [therapy 3].
OR
The majority of cases of [disease name] are self-limited and require only supportive care.
OR
[Disease name] is a medical emergency and requires prompt treatment.
OR
The mainstay of treatment for [disease name] is [therapy].
OR
The optimal therapy for [malignancy name] depends on the stage at diagnosis.
OR
[Therapy] is recommended among all patients who develop [disease name].
OR
Pharmacologic medical therapy is recommended among patients with [disease subclass 1], [disease subclass 2], and [disease subclass 3].
OR
Pharmacologic medical therapies for [disease name] include (either) [therapy 1], [therapy 2], and/or [therapy 3].
OR
Empiric therapy for [disease name] depends on [disease factor 1] and [disease factor 2].
OR
Patients with [disease subclass 1] are treated with [therapy 1], whereas patients with [disease subclass 2] are treated with [therapy 2].
Surgery
Surgical intervention is not recommended for the management of [disease name].
OR
Surgery is not the first-line treatment option for patients with [disease name]. Surgery is usually reserved for patients with either [indication 1], [indication 2], and [indication 3]
OR
The mainstay of treatment for [disease name] is medical therapy. Surgery is usually reserved for patients with either [indication 1], [indication 2], and/or [indication 3].
OR
The feasibility of surgery depends on the stage of [malignancy] at diagnosis.
OR
Surgery is the mainstay of treatment for [disease or malignancy].
Primary Prevention
There are no established measures for the primary prevention of COVID-19 associated headache.
Secondary Prevention
There are no established measures for the secondary prevention of [disease name].
OR
Effective measures for the secondary prevention of [disease name] include [strategy 1], [strategy 2], and [strategy 3].
References
- ↑ Baig, Abdul Mannan; Khaleeq, Areeba; Ali, Usman; Syeda, Hira (2020). "Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host–Virus Interaction, and Proposed Neurotropic Mechanisms". ACS Chemical Neuroscience. 11 (7): 995–998. doi:10.1021/acschemneuro.0c00122. ISSN 1948-7193.
- ↑ St-Jean JR, Jacomy H, Desforges M, Vabret A, Freymuth F, Talbot PJ (August 2004). "Human respiratory coronavirus OC43: genetic stability and neuroinvasion". J. Virol. 78 (16): 8824–34. doi:10.1128/JVI.78.16.8824-8834.2004. PMC 479063. PMID 15280490.
- ↑ Rossi, Andrea (2008). "Imaging of Acute Disseminated Encephalomyelitis". Neuroimaging Clinics of North America. 18 (1): 149–161. doi:10.1016/j.nic.2007.12.007. ISSN 1052-5149.
- ↑ St-Jean, Julien R.; Jacomy, Hélène; Desforges, Marc; Vabret, Astrid; Freymuth, François; Talbot, Pierre J. (2004). "Human Respiratory Coronavirus OC43: Genetic Stability and Neuroinvasion". Journal of Virology. 78 (16): 8824–8834. doi:10.1128/JVI.78.16.8824-8834.2004. ISSN 0022-538X.
- ↑ "National guidelines for analysis of cerebrospinal fluid for bilirubin in suspected subarachnoid haemorrhage". Ann. Clin. Biochem. 40 (Pt 5): 481–8. September 2003. doi:10.1258/000456303322326399. PMID 14503985.
- ↑ Le Rhun E, Taillibert S, Chamberlain MC (2013). "Carcinomatous meningitis: Leptomeningeal metastases in solid tumors". Surg Neurol Int. 4 (Suppl 4): S265–88. doi:10.4103/2152-7806.111304. PMC 3656567. PMID 23717798.
- ↑ Chow E, Troy SB (2014). "The differential diagnosis of hypoglycorrhachia in adult patients". Am J Med Sci. 348 (3): 186–90. doi:10.1097/MAJ.0000000000000217. PMC 4065645. PMID 24326618.
- ↑ Leen WG, Willemsen MA, Wevers RA, Verbeek MM (2012). "Cerebrospinal fluid glucose and lactate: age-specific reference values and implications for clinical practice". PLoS One. 7 (8): e42745. doi:10.1371/journal.pone.0042745. PMC 3412827. PMID 22880096.
- ↑ Negrini B, Kelleher KJ, Wald ER (2000). "Cerebrospinal fluid findings in aseptic versus bacterial meningitis". Pediatrics. 105 (2): 316–9. PMID 10654948.
- ↑ Brouwer MC, Tunkel AR, van de Beek D (2010). "Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis". Clin Microbiol Rev. 23 (3): 467–92. doi:10.1128/CMR.00070-09. PMC 2901656. PMID 20610819.
- ↑ Vermeulen M, Hasan D, Blijenberg BG, Hijdra A, van Gijn J (July 1989). "Xanthochromia after subarachnoid haemorrhage needs no revisitation". J. Neurol. Neurosurg. Psychiatry. 52 (7): 826–8. doi:10.1136/jnnp.52.7.826. PMC 1031927. PMID 2769274.
- ↑ Wasay M, Mekan SF, Khelaeni B, Saeed Z, Hassan A, Cheema Z, Bakshi R (June 2005). "Extra temporal involvement in herpes simplex encephalitis". Eur. J. Neurol. 12 (6): 475–9. doi:10.1111/j.1468-1331.2005.00999.x. PMID 15885053.
- ↑ Glaser CA, Honarmand S, Anderson LJ, Schnurr DP, Forghani B, Cossen CK, Schuster FL, Christie LJ, Tureen JH (December 2006). "Beyond viruses: clinical profiles and etiologies associated with encephalitis". Clin. Infect. Dis. 43 (12): 1565–77. doi:10.1086/509330. PMID 17109290.
- ↑ Meltzer EO, Hamilos DL (May 2011). "Rhinosinusitis diagnosis and management for the clinician: a synopsis of recent consensus guidelines". Mayo Clin. Proc. 86 (5): 427–43. doi:10.4065/mcp.2010.0392. PMC 3084646. PMID 21490181.
- ↑ Rasmussen BK, Jensen R, Schroll M, Olesen J (1991). "Epidemiology of headache in a general population--a prevalence study". J Clin Epidemiol. 44 (11): 1147–57. doi:10.1016/0895-4356(91)90147-2. PMID 1941010.
- ↑ Kelman L (October 2004). "The premonitory symptoms (prodrome): a tertiary care study of 893 migraineurs". Headache. 44 (9): 865–72. doi:10.1111/j.1526-4610.2004.04168.x. PMID 15447695.
- ↑ Laurell K, Artto V, Bendtsen L, Hagen K, Häggström J, Linde M, Söderström L, Tronvik E, Wessman M, Zwart JA, Kallela M (September 2016). "Premonitory symptoms in migraine: A cross-sectional study in 2714 persons". Cephalalgia. 36 (10): 951–9. doi:10.1177/0333102415620251. PMID 26643378.
- ↑ Charlotte E. Grayson and The Cleveland Clinic Neuroscience Center (October 2004). "Cluster Headaches". WebMD. Retrieved 2006-09-22.
- ↑ Drummond PD (October 1994). "Sweating and vascular responses in the face: normal regulation and dysfunction in migraine, cluster headache and harlequin syndrome". Clin. Auton. Res. 4 (5): 273–85. doi:10.1007/BF01827433. PMID 7888747.
- ↑ Drummond PD (June 2006). "Mechanisms of autonomic disturbance in the face during and between attacks of cluster headache". Cephalalgia. 26 (6): 633–41. doi:10.1111/j.1468-2982.2006.01106.x. PMID 16686902.
- ↑ Ekbom K (August 1990). "Evaluation of clinical criteria for cluster headache with special reference to the classification of the International Headache Society". Cephalalgia. 10 (4): 195–7. doi:10.1046/j.1468-2982.1990.1004195.x. PMID 2245469.
- ↑ Sandrini G, Antonaci F, Pucci E, Bono G, Nappi G (December 1994). "Comparative study with EMG, pressure algometry and manual palpation in tension-type headache and migraine". Cephalalgia. 14 (6): 451–7, discussion 394–5. doi:10.1046/j.1468-2982.1994.1406451.x. PMID 7697707.
- ↑ Jensen R, Fuglsang-Frederiksen A (June 1994). "Quantitative surface EMG of pericranial muscles. Relation to age and sex in a general population". Electroencephalogr Clin Neurophysiol. 93 (3): 175–83. doi:10.1016/0168-5597(94)90038-8. PMID 7515793.