COVID-19-associated headache: Difference between revisions
No edit summary |
No edit summary |
||
| Line 9: | Line 9: | ||
==Historical Perspective== | ==Historical Perspective== | ||
The association between COVID-19 and [[headache]] was made in 2020. | |||
The association between [ | |||
==Classification== | ==Classification== | ||
There is no established system for the classification of COVID-19 associated headache. | There is no established system for the [[classification]] of COVID-19 associated headache. | ||
==Pathophysiology== | ==Pathophysiology== | ||
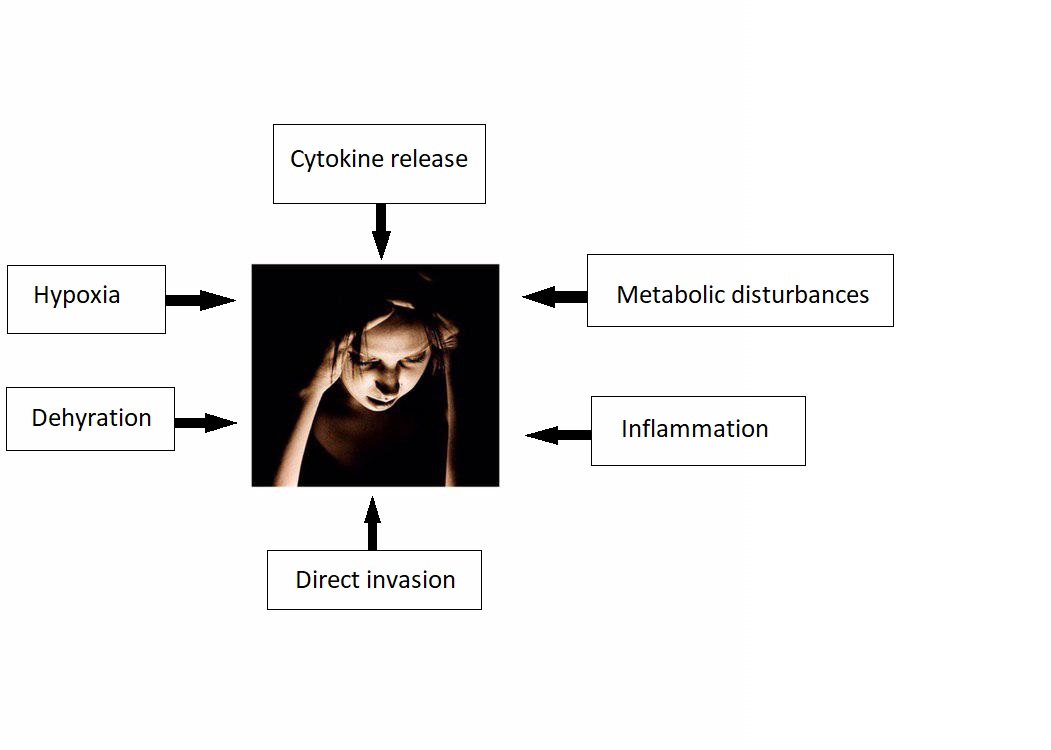
*The exact pathogenesis of headache in COVID 19 patients is not fully understood. | *The exact [[pathogenesis]] of [[headache]] in COVID 19 patients is not fully understood. | ||
*It is thought that headache is the result of:<ref name="BaigKhaleeq2020">{{cite journal|last1=Baig|first1=Abdul Mannan|last2=Khaleeq|first2=Areeba|last3=Ali|first3=Usman|last4=Syeda|first4=Hira|title=Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host–Virus Interaction, and Proposed Neurotropic Mechanisms|journal=ACS Chemical Neuroscience|volume=11|issue=7|year=2020|pages=995–998|issn=1948-7193|doi=10.1021/acschemneuro.0c00122}}</ref><ref name="pmid15280490">{{cite journal |vauthors=St-Jean JR, Jacomy H, Desforges M, Vabret A, Freymuth F, Talbot PJ |title=Human respiratory coronavirus OC43: genetic stability and neuroinvasion |journal=J. Virol. |volume=78 |issue=16 |pages=8824–34 |date=August 2004 |pmid=15280490 |pmc=479063 |doi=10.1128/JVI.78.16.8824-8834.2004 |url=}}</ref><ref name="Rossi2008">{{cite journal|last1=Rossi|first1=Andrea|title=Imaging of Acute Disseminated Encephalomyelitis|journal=Neuroimaging Clinics of North America|volume=18|issue=1|year=2008|pages=149–161|issn=10525149|doi=10.1016/j.nic.2007.12.007}}</ref><ref name="St-JeanJacomy2004">{{cite journal|last1=St-Jean|first1=Julien R.|last2=Jacomy|first2=Hélène|last3=Desforges|first3=Marc|last4=Vabret|first4=Astrid|last5=Freymuth|first5=François|last6=Talbot|first6=Pierre J.|title=Human Respiratory Coronavirus OC43: Genetic Stability and Neuroinvasion|journal=Journal of Virology|volume=78|issue=16|year=2004|pages=8824–8834|issn=0022-538X|doi=10.1128/JVI.78.16.8824-8834.2004}}</ref> | *It is thought that headache is the result of:<ref name="BaigKhaleeq2020">{{cite journal|last1=Baig|first1=Abdul Mannan|last2=Khaleeq|first2=Areeba|last3=Ali|first3=Usman|last4=Syeda|first4=Hira|title=Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host–Virus Interaction, and Proposed Neurotropic Mechanisms|journal=ACS Chemical Neuroscience|volume=11|issue=7|year=2020|pages=995–998|issn=1948-7193|doi=10.1021/acschemneuro.0c00122}}</ref><ref name="pmid15280490">{{cite journal |vauthors=St-Jean JR, Jacomy H, Desforges M, Vabret A, Freymuth F, Talbot PJ |title=Human respiratory coronavirus OC43: genetic stability and neuroinvasion |journal=J. Virol. |volume=78 |issue=16 |pages=8824–34 |date=August 2004 |pmid=15280490 |pmc=479063 |doi=10.1128/JVI.78.16.8824-8834.2004 |url=}}</ref><ref name="Rossi2008">{{cite journal|last1=Rossi|first1=Andrea|title=Imaging of Acute Disseminated Encephalomyelitis|journal=Neuroimaging Clinics of North America|volume=18|issue=1|year=2008|pages=149–161|issn=10525149|doi=10.1016/j.nic.2007.12.007}}</ref><ref name="St-JeanJacomy2004">{{cite journal|last1=St-Jean|first1=Julien R.|last2=Jacomy|first2=Hélène|last3=Desforges|first3=Marc|last4=Vabret|first4=Astrid|last5=Freymuth|first5=François|last6=Talbot|first6=Pierre J.|title=Human Respiratory Coronavirus OC43: Genetic Stability and Neuroinvasion|journal=Journal of Virology|volume=78|issue=16|year=2004|pages=8824–8834|issn=0022-538X|doi=10.1128/JVI.78.16.8824-8834.2004}}</ref> | ||
**Cytokine release | **[[Cytokine release syndrome|Cytokine release]] | ||
***There is higher concentration on IL-6 and INF-gamma in patients infected with SARS/ CoV2. | ***There is higher concentration on [[IL-6]] and [[Interferon-gamma|INF-gamma]] in [[Patient|patients]] infected with [[SARS-CoV-2|SARS/ CoV2]]. | ||
***Cytokines can disrupt blood brain barrier and cause tissue injury and cerebral edema. | ***[[Cytokine|Cytokines]] can disrupt [[Blood-brain barrier|blood brain barrier]] and cause [[tissue]] injury and [[cerebral edema]]. | ||
*** | *** | ||
*** | *** | ||
**Direct invasion | **Direct [[invasion]] | ||
**Metabolic disturbances | **Metabolic disturbances | ||
**Inflammation | **[[Inflammation]] | ||
**Dehydration | **[[Dehydration]] | ||
**Hypoxia | **[[Hypoxia]] | ||
[[File:Photo 2020-06-24 15-35-07.jpg|500px|none|thumb|By {{Fs}} / https://en.wikipedia.org/wiki/File:Migraine.jpg]] | [[File:Photo 2020-06-24 15-35-07.jpg|500px|none|thumb|By {{Fs}} / https://en.wikipedia.org/wiki/File:Migraine.jpg]] | ||
==Causes== | ==Causes== | ||
COVID-19 associated headache may be caused by SARS-CoV-2 virus. | COVID-19 associated headache may be caused by [[SARS-CoV-2|SARS-CoV-2 virus]]. | ||
==Differentiating COVID-19-associated headache from other Diseases== | ==Differentiating COVID-19-associated headache from other Diseases== | ||
COVID-19-associated headache must be differentiated from other diseases that cause headache, such as: <ref name="pmid14503985">{{cite journal |vauthors= |title=National guidelines for analysis of cerebrospinal fluid for bilirubin in suspected subarachnoid haemorrhage |journal=Ann. Clin. Biochem. |volume=40 |issue=Pt 5 |pages=481–8 |date=September 2003 |pmid=14503985 |doi=10.1258/000456303322326399 |url=}}</ref><ref name="pmid23717798">{{cite journal| author=Le Rhun E, Taillibert S, Chamberlain MC| title=Carcinomatous meningitis: Leptomeningeal metastases in solid tumors. | journal=Surg Neurol Int | year= 2013 | volume= 4 | issue= Suppl 4 | pages= S265-88 | pmid=23717798 | doi=10.4103/2152-7806.111304 | pmc=3656567 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23717798 }}</ref><ref name="pmid24326618">{{cite journal| author=Chow E, Troy SB| title=The differential diagnosis of hypoglycorrhachia in adult patients. | journal=Am J Med Sci | year= 2014 | volume= 348 | issue= 3 | pages= 186-90 | pmid=24326618 | doi=10.1097/MAJ.0000000000000217 | pmc=4065645 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24326618 }}</ref><ref name="pmid22880096">{{cite journal| author=Leen WG, Willemsen MA, Wevers RA, Verbeek MM| title=Cerebrospinal fluid glucose and lactate: age-specific reference values and implications for clinical practice. | journal=PLoS One | year= 2012 | volume= 7 | issue= 8 | pages= e42745 | pmid=22880096 | doi=10.1371/journal.pone.0042745 | pmc=3412827 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22880096 }}</ref><ref name="pmid10654948">{{cite journal| author=Negrini B, Kelleher KJ, Wald ER| title=Cerebrospinal fluid findings in aseptic versus bacterial meningitis. | journal=Pediatrics | year= 2000 | volume= 105 | issue= 2 | pages= 316-9 | pmid=10654948 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10654948 }}</ref><ref name="pmid20610819">{{cite journal| author=Brouwer MC, Tunkel AR, van de Beek D| title=Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis. | journal=Clin Microbiol Rev | year= 2010 | volume= 23 | issue= 3 | pages= 467-92 | pmid=20610819 | doi=10.1128/CMR.00070-09 | pmc=2901656 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20610819 }}</ref><ref name="pmid2769274">{{cite journal |vauthors=Vermeulen M, Hasan D, Blijenberg BG, Hijdra A, van Gijn J |title=Xanthochromia after subarachnoid haemorrhage needs no revisitation |journal=J. Neurol. Neurosurg. Psychiatry |volume=52 |issue=7 |pages=826–8 |date=July 1989 |pmid=2769274 |pmc=1031927 |doi=10.1136/jnnp.52.7.826 |url=}}</ref><ref name="pmid15885053">{{cite journal |vauthors=Wasay M, Mekan SF, Khelaeni B, Saeed Z, Hassan A, Cheema Z, Bakshi R |title=Extra temporal involvement in herpes simplex encephalitis |journal=Eur. J. Neurol. |volume=12 |issue=6 |pages=475–9 |date=June 2005 |pmid=15885053 |doi=10.1111/j.1468-1331.2005.00999.x |url=}}</ref><ref name="pmid17109290">{{cite journal |vauthors=Glaser CA, Honarmand S, Anderson LJ, Schnurr DP, Forghani B, Cossen CK, Schuster FL, Christie LJ, Tureen JH |title=Beyond viruses: clinical profiles and etiologies associated with encephalitis |journal=Clin. Infect. Dis. |volume=43 |issue=12 |pages=1565–77 |date=December 2006 |pmid=17109290 |doi=10.1086/509330 |url=}}</ref><ref name="pmid21490181">{{cite journal |vauthors=Meltzer EO, Hamilos DL |title=Rhinosinusitis diagnosis and management for the clinician: a synopsis of recent consensus guidelines |journal=Mayo Clin. Proc. |volume=86 |issue=5 |pages=427–43 |date=May 2011 |pmid=21490181 |pmc=3084646 |doi=10.4065/mcp.2010.0392 |url=}}</ref><ref name="pmid1941010">{{cite journal |vauthors=Rasmussen BK, Jensen R, Schroll M, Olesen J |title=Epidemiology of headache in a general population--a prevalence study |journal=J Clin Epidemiol |volume=44 |issue=11 |pages=1147–57 |date=1991 |pmid=1941010 |doi=10.1016/0895-4356(91)90147-2 |url=}}</ref><ref name="pmid15447695">{{cite journal |vauthors=Kelman L |title=The premonitory symptoms (prodrome): a tertiary care study of 893 migraineurs |journal=Headache |volume=44 |issue=9 |pages=865–72 |date=October 2004 |pmid=15447695 |doi=10.1111/j.1526-4610.2004.04168.x |url=}}</ref><ref name="pmid26643378">{{cite journal |vauthors=Laurell K, Artto V, Bendtsen L, Hagen K, Häggström J, Linde M, Söderström L, Tronvik E, Wessman M, Zwart JA, Kallela M |title=Premonitory symptoms in migraine: A cross-sectional study in 2714 persons |journal=Cephalalgia |volume=36 |issue=10 |pages=951–9 |date=September 2016 |pmid=26643378 |doi=10.1177/0333102415620251 |url=}}</ref><ref>{{cite web | author=Charlotte E. Grayson and The Cleveland Clinic Neuroscience Center | title=Cluster Headaches |url=http://www.webmd.com/content/article/46/1826_50688.htm | date=October 2004 | publisher=WebMD | accessdate=2006-09-22}}</ref><ref name="pmid7888747">{{cite journal |vauthors=Drummond PD |title=Sweating and vascular responses in the face: normal regulation and dysfunction in migraine, cluster headache and harlequin syndrome |journal=Clin. Auton. Res. |volume=4 |issue=5 |pages=273–85 |date=October 1994 |pmid=7888747 |doi=10.1007/BF01827433 |url=}}</ref><ref name="pmid16686902">{{cite journal |vauthors=Drummond PD |title=Mechanisms of autonomic disturbance in the face during and between attacks of cluster headache |journal=Cephalalgia |volume=26 |issue=6 |pages=633–41 |date=June 2006 |pmid=16686902 |doi=10.1111/j.1468-2982.2006.01106.x |url=}}</ref><ref name="pmid2245469">{{cite journal |vauthors=Ekbom K |title=Evaluation of clinical criteria for cluster headache with special reference to the classification of the International Headache Society |journal=Cephalalgia |volume=10 |issue=4 |pages=195–7 |date=August 1990 |pmid=2245469 |doi=10.1046/j.1468-2982.1990.1004195.x |url=}}</ref><ref name="pmid7697707">{{cite journal |vauthors=Sandrini G, Antonaci F, Pucci E, Bono G, Nappi G |title=Comparative study with EMG, pressure algometry and manual palpation in tension-type headache and migraine |journal=Cephalalgia |volume=14 |issue=6 |pages=451–7; discussion 394–5 |date=December 1994 |pmid=7697707 |doi=10.1046/j.1468-2982.1994.1406451.x |url=}}</ref><ref name="pmid7515793">{{cite journal |vauthors=Jensen R, Fuglsang-Frederiksen A |title=Quantitative surface EMG of pericranial muscles. Relation to age and sex in a general population |journal=Electroencephalogr Clin Neurophysiol |volume=93 |issue=3 |pages=175–83 |date=June 1994 |pmid=7515793 |doi=10.1016/0168-5597(94)90038-8 |url=}}</ref> | |||
[ | * [[Migraine]] | ||
* [[Tension-type headache]] | |||
* [[Cluster headache]] | |||
* [[Seizure]] | |||
* [[Meningitis]] | |||
* [[Encephalitis]] | |||
* [[Neurosyphilis]] | |||
* [[SAH]] | |||
* [[Subdural hematoma]] | |||
* [[Brain tumor]] | |||
** [[Astrocytoma]] | |||
** [[Oligodendroglioma]] | |||
** [[Meningioma]] | |||
** [[Hemangioblastoma]] | |||
** [[Pituitary adenoma]] | |||
** [[Schwannoma]] | |||
** [[Primary CNS lymphoma]] | |||
** [[Medulloblastoma]] | |||
** [[Ependymoma]] | |||
** [[Craniopharyngioma]] | |||
** [[Pinealoma]] | |||
** [[Brain metastasis]] | |||
* [[Hypertensive encephalopathy]] | |||
* [[Brain abscess]] | |||
* [[Hemorrhagic stroke]] | |||
* [[Wernicke's encephalopathy|Wernickes encephalopathy]] | |||
* [[Drug toxicity]] | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
Revision as of 18:00, 2 July 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Fahimeh Shojaei, M.D.
Synonyms and keywords:
Overview
Historical Perspective
The association between COVID-19 and headache was made in 2020.
Classification
There is no established system for the classification of COVID-19 associated headache.
Pathophysiology
- The exact pathogenesis of headache in COVID 19 patients is not fully understood.
- It is thought that headache is the result of:[1][2][3][4]
- Cytokine release
- There is higher concentration on IL-6 and INF-gamma in patients infected with SARS/ CoV2.
- Cytokines can disrupt blood brain barrier and cause tissue injury and cerebral edema.
- Direct invasion
- Metabolic disturbances
- Inflammation
- Dehydration
- Hypoxia
- Cytokine release
Causes
COVID-19 associated headache may be caused by SARS-CoV-2 virus.
Differentiating COVID-19-associated headache from other Diseases
COVID-19-associated headache must be differentiated from other diseases that cause headache, such as: [5][6][7][8][9][10][11][12][13][14][15][16][17][18][19][20][21][22][23]
- Migraine
- Tension-type headache
- Cluster headache
- Seizure
- Meningitis
- Encephalitis
- Neurosyphilis
- SAH
- Subdural hematoma
- Brain tumor
- Hypertensive encephalopathy
- Brain abscess
- Hemorrhagic stroke
- Wernickes encephalopathy
- Drug toxicity
Epidemiology and Demographics
The incidence/prevalence of [disease name] is approximately [number range] per 100,000 individuals worldwide.
OR
In [year], the incidence/prevalence of [disease name] was estimated to be [number range] cases per 100,000 individuals worldwide.
OR
In [year], the incidence of [disease name] is approximately [number range] per 100,000 individuals with a case-fatality rate of [number range]%.
Patients of all age groups may develop [disease name].
OR
The incidence of [disease name] increases with age; the median age at diagnosis is [#] years.
OR
[Disease name] commonly affects individuals younger than/older than [number of years] years of age.
OR
[Chronic disease name] is usually first diagnosed among [age group].
OR
[Acute disease name] commonly affects [age group].
There is no racial predilection to [disease name].
OR
[Disease name] usually affects individuals of the [race 1] race. [Race 2] individuals are less likely to develop [disease name].
[Disease name] affects men and women equally.
OR
[Gender 1] are more commonly affected by [disease name] than [gender 2]. The [gender 1] to [gender 2] ratio is approximately [number > 1] to 1.
The majority of [disease name] cases are reported in [geographical region].
OR
[Disease name] is a common/rare disease that tends to affect [patient population 1] and [patient population 2].
Risk Factors
There are no established risk factors for [disease name].
OR
The most potent risk factor in the development of [disease name] is [risk factor 1]. Other risk factors include [risk factor 2], [risk factor 3], and [risk factor 4].
OR
Common risk factors in the development of [disease name] include [risk factor 1], [risk factor 2], [risk factor 3], and [risk factor 4].
OR
Common risk factors in the development of [disease name] may be occupational, environmental, genetic, and viral.
Screening
There is insufficient evidence to recommend routine screening for COVID-19 associated headache.
Natural History, Complications, and Prognosis
If left untreated, [#]% of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
OR
Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
OR
Prognosis is generally excellent/good/poor, and the 1/5/10-year mortality/survival rate of patients with [disease name] is approximately [#]%.
Diagnosis
Diagnostic Study of Choice
The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met: [criterion 1], [criterion 2], [criterion 3], and [criterion 4].
OR
The diagnosis of [disease name] is based on the [criteria name] criteria, which include [criterion 1], [criterion 2], and [criterion 3].
OR
The diagnosis of [disease name] is based on the [definition name] definition, which includes [criterion 1], [criterion 2], and [criterion 3].
OR
There are no established criteria for the diagnosis of [disease name].
History and Symptoms
The majority of patients with [disease name] are asymptomatic.
OR
The hallmark of [disease name] is [finding]. A positive history of [finding 1] and [finding 2] is suggestive of [disease name]. The most common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3]. Common symptoms of [disease] include [symptom 1], [symptom 2], and [symptom 3]. Less common symptoms of [disease name] include [symptom 1], [symptom 2], and [symptom 3].
Physical Examination
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Laboratory Findings
An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name].
OR
Laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
OR
[Test] is usually normal among patients with [disease name].
OR
Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication].
OR
There are no diagnostic laboratory findings associated with [disease name].
Electrocardiogram
There are no ECG findings associated with [disease name].
OR
An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
X-ray
There are no x-ray findings associated with [disease name].
OR
An x-ray may be helpful in the diagnosis of [disease name]. Findings on an x-ray suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no x-ray findings associated with [disease name]. However, an x-ray may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with [disease name].
OR
Echocardiography/ultrasound may be helpful in the diagnosis of [disease name]. Findings on an echocardiography/ultrasound suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no echocardiography/ultrasound findings associated with [disease name]. However, an echocardiography/ultrasound may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
CT scan
There are no CT scan findings associated with [disease name].
OR
[Location] CT scan may be helpful in the diagnosis of [disease name]. Findings on CT scan suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no CT scan findings associated with [disease name]. However, a CT scan may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
MRI
There are no MRI findings associated with [disease name].
OR
[Location] MRI may be helpful in the diagnosis of [disease name]. Findings on MRI suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no MRI findings associated with [disease name]. However, a MRI may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Other Imaging Findings
There are no other imaging findings associated with [disease name].
OR
[Imaging modality] may be helpful in the diagnosis of [disease name]. Findings on an [imaging modality] suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
There are no other diagnostic studies associated with [disease name].
OR
[Diagnostic study] may be helpful in the diagnosis of [disease name]. Findings suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
There is no treatment for [disease name]; the mainstay of therapy is supportive care.
OR
Supportive therapy for [disease name] includes [therapy 1], [therapy 2], and [therapy 3].
OR
The majority of cases of [disease name] are self-limited and require only supportive care.
OR
[Disease name] is a medical emergency and requires prompt treatment.
OR
The mainstay of treatment for [disease name] is [therapy].
OR
The optimal therapy for [malignancy name] depends on the stage at diagnosis.
OR
[Therapy] is recommended among all patients who develop [disease name].
OR
Pharmacologic medical therapy is recommended among patients with [disease subclass 1], [disease subclass 2], and [disease subclass 3].
OR
Pharmacologic medical therapies for [disease name] include (either) [therapy 1], [therapy 2], and/or [therapy 3].
OR
Empiric therapy for [disease name] depends on [disease factor 1] and [disease factor 2].
OR
Patients with [disease subclass 1] are treated with [therapy 1], whereas patients with [disease subclass 2] are treated with [therapy 2].
Surgery
Surgical intervention is not recommended for the management of [disease name].
OR
Surgery is not the first-line treatment option for patients with [disease name]. Surgery is usually reserved for patients with either [indication 1], [indication 2], and [indication 3]
OR
The mainstay of treatment for [disease name] is medical therapy. Surgery is usually reserved for patients with either [indication 1], [indication 2], and/or [indication 3].
OR
The feasibility of surgery depends on the stage of [malignancy] at diagnosis.
OR
Surgery is the mainstay of treatment for [disease or malignancy].
Primary Prevention
There are no established measures for the primary prevention of COVID-19 associated headache.
Secondary Prevention
There are no established measures for the secondary prevention of [disease name].
OR
Effective measures for the secondary prevention of [disease name] include [strategy 1], [strategy 2], and [strategy 3].
References
- ↑ Baig, Abdul Mannan; Khaleeq, Areeba; Ali, Usman; Syeda, Hira (2020). "Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host–Virus Interaction, and Proposed Neurotropic Mechanisms". ACS Chemical Neuroscience. 11 (7): 995–998. doi:10.1021/acschemneuro.0c00122. ISSN 1948-7193.
- ↑ St-Jean JR, Jacomy H, Desforges M, Vabret A, Freymuth F, Talbot PJ (August 2004). "Human respiratory coronavirus OC43: genetic stability and neuroinvasion". J. Virol. 78 (16): 8824–34. doi:10.1128/JVI.78.16.8824-8834.2004. PMC 479063. PMID 15280490.
- ↑ Rossi, Andrea (2008). "Imaging of Acute Disseminated Encephalomyelitis". Neuroimaging Clinics of North America. 18 (1): 149–161. doi:10.1016/j.nic.2007.12.007. ISSN 1052-5149.
- ↑ St-Jean, Julien R.; Jacomy, Hélène; Desforges, Marc; Vabret, Astrid; Freymuth, François; Talbot, Pierre J. (2004). "Human Respiratory Coronavirus OC43: Genetic Stability and Neuroinvasion". Journal of Virology. 78 (16): 8824–8834. doi:10.1128/JVI.78.16.8824-8834.2004. ISSN 0022-538X.
- ↑ "National guidelines for analysis of cerebrospinal fluid for bilirubin in suspected subarachnoid haemorrhage". Ann. Clin. Biochem. 40 (Pt 5): 481–8. September 2003. doi:10.1258/000456303322326399. PMID 14503985.
- ↑ Le Rhun E, Taillibert S, Chamberlain MC (2013). "Carcinomatous meningitis: Leptomeningeal metastases in solid tumors". Surg Neurol Int. 4 (Suppl 4): S265–88. doi:10.4103/2152-7806.111304. PMC 3656567. PMID 23717798.
- ↑ Chow E, Troy SB (2014). "The differential diagnosis of hypoglycorrhachia in adult patients". Am J Med Sci. 348 (3): 186–90. doi:10.1097/MAJ.0000000000000217. PMC 4065645. PMID 24326618.
- ↑ Leen WG, Willemsen MA, Wevers RA, Verbeek MM (2012). "Cerebrospinal fluid glucose and lactate: age-specific reference values and implications for clinical practice". PLoS One. 7 (8): e42745. doi:10.1371/journal.pone.0042745. PMC 3412827. PMID 22880096.
- ↑ Negrini B, Kelleher KJ, Wald ER (2000). "Cerebrospinal fluid findings in aseptic versus bacterial meningitis". Pediatrics. 105 (2): 316–9. PMID 10654948.
- ↑ Brouwer MC, Tunkel AR, van de Beek D (2010). "Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis". Clin Microbiol Rev. 23 (3): 467–92. doi:10.1128/CMR.00070-09. PMC 2901656. PMID 20610819.
- ↑ Vermeulen M, Hasan D, Blijenberg BG, Hijdra A, van Gijn J (July 1989). "Xanthochromia after subarachnoid haemorrhage needs no revisitation". J. Neurol. Neurosurg. Psychiatry. 52 (7): 826–8. doi:10.1136/jnnp.52.7.826. PMC 1031927. PMID 2769274.
- ↑ Wasay M, Mekan SF, Khelaeni B, Saeed Z, Hassan A, Cheema Z, Bakshi R (June 2005). "Extra temporal involvement in herpes simplex encephalitis". Eur. J. Neurol. 12 (6): 475–9. doi:10.1111/j.1468-1331.2005.00999.x. PMID 15885053.
- ↑ Glaser CA, Honarmand S, Anderson LJ, Schnurr DP, Forghani B, Cossen CK, Schuster FL, Christie LJ, Tureen JH (December 2006). "Beyond viruses: clinical profiles and etiologies associated with encephalitis". Clin. Infect. Dis. 43 (12): 1565–77. doi:10.1086/509330. PMID 17109290.
- ↑ Meltzer EO, Hamilos DL (May 2011). "Rhinosinusitis diagnosis and management for the clinician: a synopsis of recent consensus guidelines". Mayo Clin. Proc. 86 (5): 427–43. doi:10.4065/mcp.2010.0392. PMC 3084646. PMID 21490181.
- ↑ Rasmussen BK, Jensen R, Schroll M, Olesen J (1991). "Epidemiology of headache in a general population--a prevalence study". J Clin Epidemiol. 44 (11): 1147–57. doi:10.1016/0895-4356(91)90147-2. PMID 1941010.
- ↑ Kelman L (October 2004). "The premonitory symptoms (prodrome): a tertiary care study of 893 migraineurs". Headache. 44 (9): 865–72. doi:10.1111/j.1526-4610.2004.04168.x. PMID 15447695.
- ↑ Laurell K, Artto V, Bendtsen L, Hagen K, Häggström J, Linde M, Söderström L, Tronvik E, Wessman M, Zwart JA, Kallela M (September 2016). "Premonitory symptoms in migraine: A cross-sectional study in 2714 persons". Cephalalgia. 36 (10): 951–9. doi:10.1177/0333102415620251. PMID 26643378.
- ↑ Charlotte E. Grayson and The Cleveland Clinic Neuroscience Center (October 2004). "Cluster Headaches". WebMD. Retrieved 2006-09-22.
- ↑ Drummond PD (October 1994). "Sweating and vascular responses in the face: normal regulation and dysfunction in migraine, cluster headache and harlequin syndrome". Clin. Auton. Res. 4 (5): 273–85. doi:10.1007/BF01827433. PMID 7888747.
- ↑ Drummond PD (June 2006). "Mechanisms of autonomic disturbance in the face during and between attacks of cluster headache". Cephalalgia. 26 (6): 633–41. doi:10.1111/j.1468-2982.2006.01106.x. PMID 16686902.
- ↑ Ekbom K (August 1990). "Evaluation of clinical criteria for cluster headache with special reference to the classification of the International Headache Society". Cephalalgia. 10 (4): 195–7. doi:10.1046/j.1468-2982.1990.1004195.x. PMID 2245469.
- ↑ Sandrini G, Antonaci F, Pucci E, Bono G, Nappi G (December 1994). "Comparative study with EMG, pressure algometry and manual palpation in tension-type headache and migraine". Cephalalgia. 14 (6): 451–7, discussion 394–5. doi:10.1046/j.1468-2982.1994.1406451.x. PMID 7697707.
- ↑ Jensen R, Fuglsang-Frederiksen A (June 1994). "Quantitative surface EMG of pericranial muscles. Relation to age and sex in a general population". Electroencephalogr Clin Neurophysiol. 93 (3): 175–83. doi:10.1016/0168-5597(94)90038-8. PMID 7515793.