Bifascicular block: Difference between revisions
Jump to navigation
Jump to search
Dima Nimri (talk | contribs) (/* 2012 ACC/AHA/HRS Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities (DO NOT EDIT) Epstein AE, DiMarco JP, Ellenbogen KA, Estes NAM III, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Pa...) |
No edit summary |
||
| Line 11: | Line 11: | ||
Bifascicular block is a conduction abnormality in the [[heart]] where two of the three main [[fascicle]]s of the [[Electrical conduction system of the heart|His-Purkinje system]] are blocked. Most commonly, it refers to a combination of [[right bundle branch block]] ([[RBBB]]) and either [[left anterior fascicular block]] ([[LAFB]]) or [[left posterior fascicular block]] ([[LPFB]]). Some authors consider [[left bundle branch block]] ([[LBBB]]) to be a technical bifascicular block, since the block occurs above the bifurcation of the left anterior and left posterior fascicles of the left bundle branch. | Bifascicular block is a conduction abnormality in the [[heart]] where two of the three main [[fascicle]]s of the [[Electrical conduction system of the heart|His-Purkinje system]] are blocked. Most commonly, it refers to a combination of [[right bundle branch block]] ([[RBBB]]) and either [[left anterior fascicular block]] ([[LAFB]]) or [[left posterior fascicular block]] ([[LPFB]]). Some authors consider [[left bundle branch block]] ([[LBBB]]) to be a technical bifascicular block, since the block occurs above the bifurcation of the left anterior and left posterior fascicles of the left bundle branch. | ||
== | ==Historical Perspective== | ||
=== | *[Disease name] was first discovered by [scientist name], a [nationality + occupation], in [year] during/following [event]. | ||
*In [year], [gene] mutations were first identified in the pathogenesis of [disease name]. | |||
*In [year], the first [discovery] was developed by [scientist] to treat/diagnose [disease name]. | |||
==Classification== | |||
*[Disease name] may be classified according to [classification method] into [number] subtypes/groups: | |||
:*[group1] | |||
:*[group2] | |||
:*[group3] | |||
*Other variants of [disease name] include [disease subtype 1], [disease subtype 2], and [disease subtype 3]. | |||
==Pathophysiology== | |||
*The pathogenesis of [disease name] is characterized by [feature1], [feature2], and [feature3]. | |||
*The [gene name] gene/Mutation in [gene name] has been associated with the development of [disease name], involving the [molecular pathway] pathway. | |||
*On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name]. | |||
*On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name]. | |||
==Clinical Features== | |||
==Differentiating [disease name] from other Diseases== | |||
*[Disease name] must be differentiated from other diseases that cause [clinical feature 1], [clinical feature 2], and [clinical feature 3], such as: | |||
:*[Differential dx1] | |||
:*[Differential dx2] | |||
:*[Differential dx3] | |||
==Epidemiology and Demographics== | |||
* The prevalence of [disease name] is approximately [number or range] per 100,000 individuals worldwide. | |||
* In [year], the incidence of [disease name] was estimated to be [number or range] cases per 100,000 individuals in [location]. | |||
===Age=== | |||
*Patients of all age groups may develop [disease name]. | |||
*[Disease name] is more commonly observed among patients aged [age range] years old. | |||
*[Disease name] is more commonly observed among [elderly patients/young patients/children]. | |||
===Gender=== | |||
*[Disease name] affects men and women equally. | |||
*[Gender 1] are more commonly affected with [disease name] than [gender 2]. | |||
* The [gender 1] to [Gender 2] ratio is approximately [number > 1] to 1. | |||
===Race=== | |||
*There is no racial predilection for [disease name]. | |||
*[Disease name] usually affects individuals of the [race 1] race. | |||
*[Race 2] individuals are less likely to develop [disease name]. | |||
==Risk Factors== | |||
*Common risk factors in the development of [disease name] are [risk factor 1], [risk factor 2], [risk factor 3], and [risk factor 4]. | |||
== Natural History, Complications and Prognosis== | |||
*The majority of patients with [disease name] remain asymptomatic for [duration/years]. | |||
*Early clinical features include [manifestation 1], [manifestation 2], and [manifestation 3]. | |||
*If left untreated, [#%] of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3]. | |||
*Common complications of [disease name] include [complication 1], [complication 2], and [complication 3]. | |||
*Prognosis is generally [excellent/good/poor], and the [1/5/10year mortality/survival rate] of patients with [disease name] is approximately [#%]. | |||
== Diagnosis == | |||
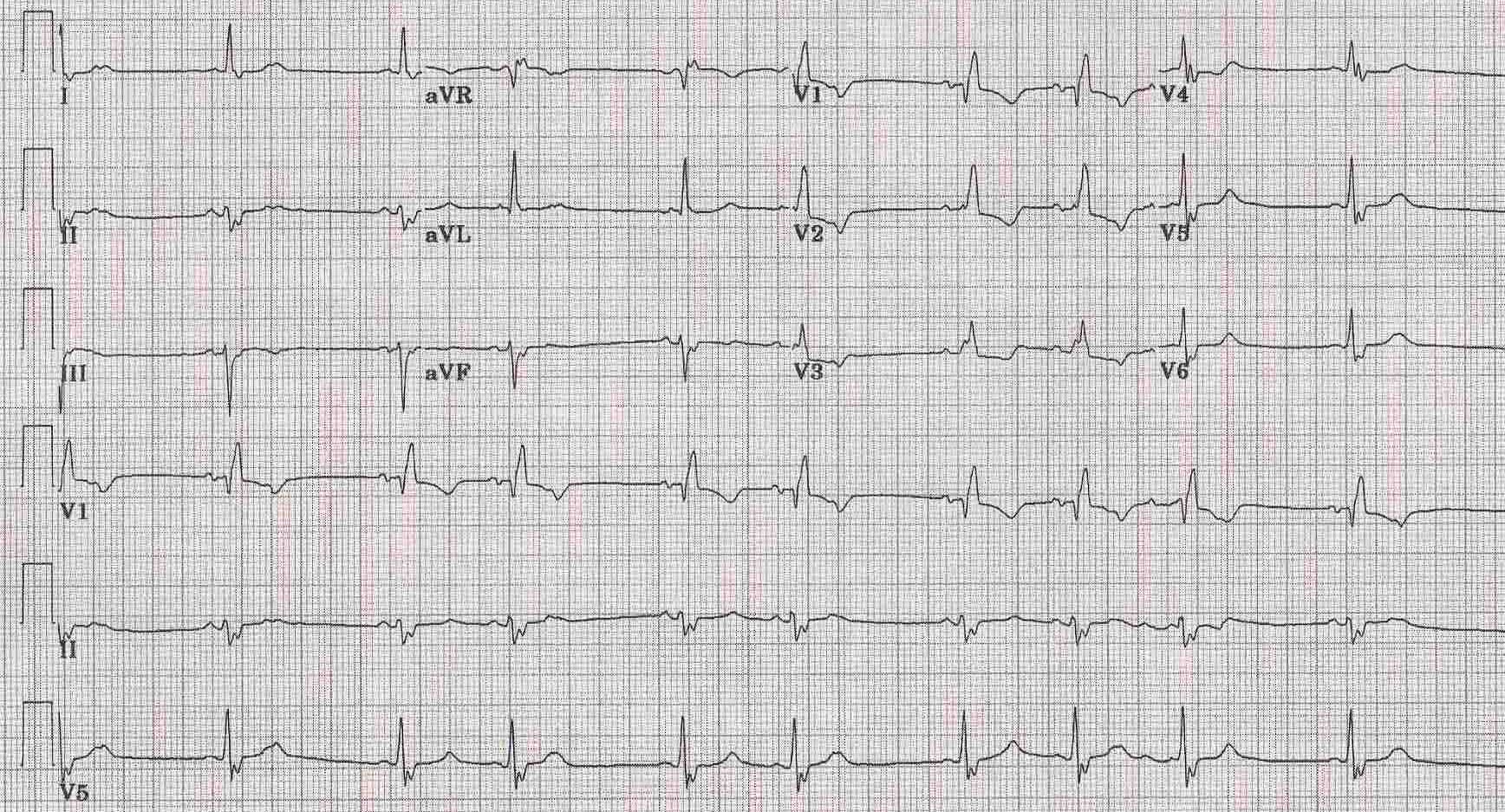
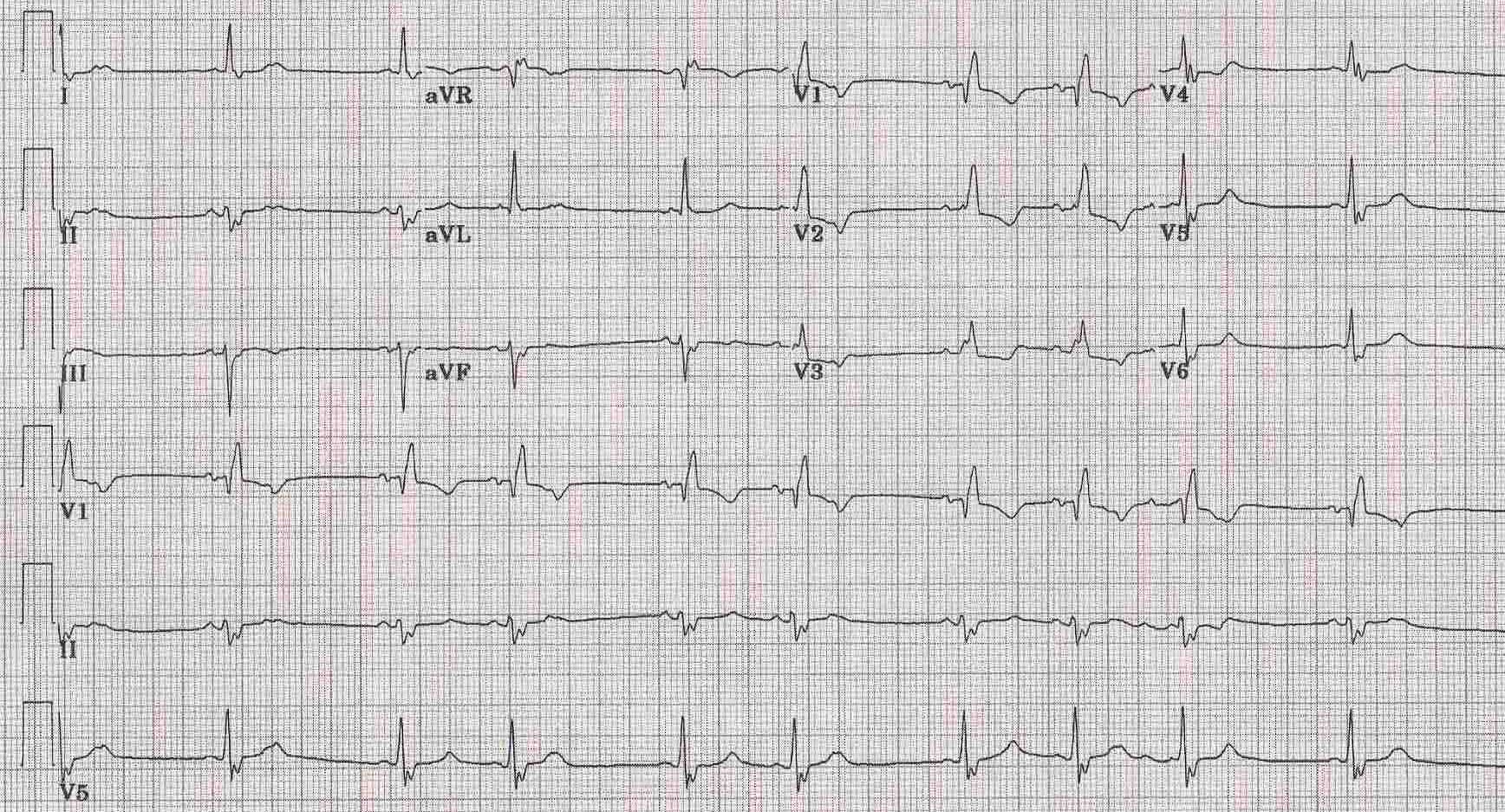
[[Image:Bifascicular1.jpg|center|500px]] | [[Image:Bifascicular1.jpg|center|500px]] | ||
===Diagnostic Criteria=== | |||
*The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met: | |||
:*[criterion 1] | |||
:*[criterion 2] | |||
:*[criterion 3] | |||
:*[criterion 4] | |||
=== Symptoms === | |||
*[Disease name] is usually asymptomatic. | |||
*Symptoms of [disease name] may include the following: | |||
:*[symptom 1] | |||
:*[symptom 2] | |||
:*[symptom 3] | |||
:*[symptom 4] | |||
:*[symptom 5] | |||
:*[symptom 6] | |||
=== Physical Examination === | |||
*Patients with [disease name] usually appear [general appearance]. | |||
*Physical examination may be remarkable for: | |||
:*[finding 1] | |||
:*[finding 2] | |||
:*[finding 3] | |||
:*[finding 4] | |||
:*[finding 5] | |||
:*[finding 6] | |||
=== Laboratory Findings === | |||
*There are no specific laboratory findings associated with [disease name]. | |||
*A [positive/negative] [test name] is diagnostic of [disease name]. | |||
*An [elevated/reduced] concentration of [serum/blood/urinary/CSF/other] [lab test] is diagnostic of [disease name]. | |||
*Other laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3]. | |||
===Imaging Findings=== | |||
*There are no [imaging study] findings associated with [disease name]. | |||
*[Imaging study 1] is the imaging modality of choice for [disease name]. | |||
*On [imaging study 1], [disease name] is characterized by [finding 1], [finding 2], and [finding 3]. | |||
*[Imaging study 2] may demonstrate [finding 1], [finding 2], and [finding 3]. | |||
=== Other Diagnostic Studies === | |||
*[Disease name] may also be diagnosed using [diagnostic study name]. | |||
*Findings on [diagnostic study name] include [finding 1], [finding 2], and [finding 3]. | |||
== Treatment == | |||
=== Medical Therapy === | |||
*There is no treatment for [disease name]; the mainstay of therapy is supportive care. | |||
*The mainstay of therapy for [disease name] is [medical therapy 1] and [medical therapy 2]. | |||
*[Medical therapy 1] acts by [mechanism of action 1]. | |||
*Response to [medical therapy 1] can be monitored with [test/physical finding/imaging] every [frequency/duration]. | |||
=== Surgery === | |||
*Surgery is the mainstay of therapy for [disease name]. | |||
*[Surgical procedure] in conjunction with [chemotherapy/radiation] is the most common approach to the treatment of [disease name]. | |||
*[Surgical procedure] can only be performed for patients with [disease stage] [disease name]. | |||
=== Prevention === | |||
*There are no primary preventive measures available for [disease name]. | |||
*Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3]. | |||
*Once diagnosed and successfully treated, patients with [disease name] are followed-up every [duration]. Follow-up testing includes [test 1], [test 2], and [test 3]. | |||
==2012 ACC/AHA/HRS Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities (DO NOT EDIT)<ref name="pmid23265327">{{cite journal |vauthors=Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO, Tracy CM, Epstein AE, Darbar D, DiMarco JP, Dunbar SB, Estes NA, Ferguson TB, Hammill SC, Karasik PE, Link MS, Marine JE, Schoenfeld MH, Shanker AJ, Silka MJ, Stevenson LW, Stevenson WG, Varosy PD |title=2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society |journal=J. Am. Coll. Cardiol. |volume=61 |issue=3 |pages=e6–75 |year=2013 |pmid=23265327 |doi=10.1016/j.jacc.2012.11.007 |url=}}</ref><ref name="Epstein"> Epstein AE, DiMarco JP, Ellenbogen KA, Estes NAM III, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices). Circulation. 2008; 117: 2820–2840. PMID 18483207 </ref>== | ==2012 ACC/AHA/HRS Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities (DO NOT EDIT)<ref name="pmid23265327">{{cite journal |vauthors=Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO, Tracy CM, Epstein AE, Darbar D, DiMarco JP, Dunbar SB, Estes NA, Ferguson TB, Hammill SC, Karasik PE, Link MS, Marine JE, Schoenfeld MH, Shanker AJ, Silka MJ, Stevenson LW, Stevenson WG, Varosy PD |title=2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society |journal=J. Am. Coll. Cardiol. |volume=61 |issue=3 |pages=e6–75 |year=2013 |pmid=23265327 |doi=10.1016/j.jacc.2012.11.007 |url=}}</ref><ref name="Epstein"> Epstein AE, DiMarco JP, Ellenbogen KA, Estes NAM III, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices). Circulation. 2008; 117: 2820–2840. PMID 18483207 </ref>== | ||
Revision as of 18:23, 7 April 2020
| Bifascicular block | |
 |
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Bifascicular block is a conduction abnormality in the heart where two of the three main fascicles of the His-Purkinje system are blocked. Most commonly, it refers to a combination of right bundle branch block (RBBB) and either left anterior fascicular block (LAFB) or left posterior fascicular block (LPFB). Some authors consider left bundle branch block (LBBB) to be a technical bifascicular block, since the block occurs above the bifurcation of the left anterior and left posterior fascicles of the left bundle branch.
Historical Perspective
- [Disease name] was first discovered by [scientist name], a [nationality + occupation], in [year] during/following [event].
- In [year], [gene] mutations were first identified in the pathogenesis of [disease name].
- In [year], the first [discovery] was developed by [scientist] to treat/diagnose [disease name].
Classification
- [Disease name] may be classified according to [classification method] into [number] subtypes/groups:
- [group1]
- [group2]
- [group3]
- Other variants of [disease name] include [disease subtype 1], [disease subtype 2], and [disease subtype 3].
Pathophysiology
- The pathogenesis of [disease name] is characterized by [feature1], [feature2], and [feature3].
- The [gene name] gene/Mutation in [gene name] has been associated with the development of [disease name], involving the [molecular pathway] pathway.
- On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
- On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Clinical Features
Differentiating [disease name] from other Diseases
- [Disease name] must be differentiated from other diseases that cause [clinical feature 1], [clinical feature 2], and [clinical feature 3], such as:
- [Differential dx1]
- [Differential dx2]
- [Differential dx3]
Epidemiology and Demographics
- The prevalence of [disease name] is approximately [number or range] per 100,000 individuals worldwide.
- In [year], the incidence of [disease name] was estimated to be [number or range] cases per 100,000 individuals in [location].
Age
- Patients of all age groups may develop [disease name].
- [Disease name] is more commonly observed among patients aged [age range] years old.
- [Disease name] is more commonly observed among [elderly patients/young patients/children].
Gender
- [Disease name] affects men and women equally.
- [Gender 1] are more commonly affected with [disease name] than [gender 2].
- The [gender 1] to [Gender 2] ratio is approximately [number > 1] to 1.
Race
- There is no racial predilection for [disease name].
- [Disease name] usually affects individuals of the [race 1] race.
- [Race 2] individuals are less likely to develop [disease name].
Risk Factors
- Common risk factors in the development of [disease name] are [risk factor 1], [risk factor 2], [risk factor 3], and [risk factor 4].
Natural History, Complications and Prognosis
- The majority of patients with [disease name] remain asymptomatic for [duration/years].
- Early clinical features include [manifestation 1], [manifestation 2], and [manifestation 3].
- If left untreated, [#%] of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
- Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
- Prognosis is generally [excellent/good/poor], and the [1/5/10year mortality/survival rate] of patients with [disease name] is approximately [#%].
Diagnosis
Diagnostic Criteria
- The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met:
- [criterion 1]
- [criterion 2]
- [criterion 3]
- [criterion 4]
Symptoms
- [Disease name] is usually asymptomatic.
- Symptoms of [disease name] may include the following:
- [symptom 1]
- [symptom 2]
- [symptom 3]
- [symptom 4]
- [symptom 5]
- [symptom 6]
Physical Examination
- Patients with [disease name] usually appear [general appearance].
- Physical examination may be remarkable for:
- [finding 1]
- [finding 2]
- [finding 3]
- [finding 4]
- [finding 5]
- [finding 6]
Laboratory Findings
- There are no specific laboratory findings associated with [disease name].
- A [positive/negative] [test name] is diagnostic of [disease name].
- An [elevated/reduced] concentration of [serum/blood/urinary/CSF/other] [lab test] is diagnostic of [disease name].
- Other laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
Imaging Findings
- There are no [imaging study] findings associated with [disease name].
- [Imaging study 1] is the imaging modality of choice for [disease name].
- On [imaging study 1], [disease name] is characterized by [finding 1], [finding 2], and [finding 3].
- [Imaging study 2] may demonstrate [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
- [Disease name] may also be diagnosed using [diagnostic study name].
- Findings on [diagnostic study name] include [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
- There is no treatment for [disease name]; the mainstay of therapy is supportive care.
- The mainstay of therapy for [disease name] is [medical therapy 1] and [medical therapy 2].
- [Medical therapy 1] acts by [mechanism of action 1].
- Response to [medical therapy 1] can be monitored with [test/physical finding/imaging] every [frequency/duration].
Surgery
- Surgery is the mainstay of therapy for [disease name].
- [Surgical procedure] in conjunction with [chemotherapy/radiation] is the most common approach to the treatment of [disease name].
- [Surgical procedure] can only be performed for patients with [disease stage] [disease name].
Prevention
- There are no primary preventive measures available for [disease name].
- Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
- Once diagnosed and successfully treated, patients with [disease name] are followed-up every [duration]. Follow-up testing includes [test 1], [test 2], and [test 3].
2012 ACC/AHA/HRS Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities (DO NOT EDIT)[1][2]
Permanent Pacing in Chronic Bifascicular Block (DO NOT EDIT)[2]
| Class I |
| "1. Permanent pacemaker implantation is indicated for advanced second-degree AV block or intermittent third-degree AV block. (Level of Evidence: B)[3][4][5][6][7][8][9]" |
| "2. Permanent pacemaker implantation is indicated for type II second-degree AV block. (Level of Evidence: B)[10][11][12][13]" |
| "3. Permanent pacemaker implantation is indicated for alternating bundle-branch block. (Level of Evidence: C)" |
| Class III (No Benefit) |
| "1. Permanent pacemaker implantation is not indicated for fascicular block without AV block or symptoms. (Level of Evidence: B)[14][15][16][17]" |
| "2. Permanent pacemaker implantation is not indicated for fascicular block with first-degree AV block without symptoms. (Level of Evidence: B)[14][15][16][17]" |
| Class IIa |
| "1. Permanent pacemaker implantation is reasonable for syncope not demonstrated to be due to AV block when other likely causes have been excluded, specifically ventricular tachycardia (VT). (Level of Evidence: B)[13][18][19][14][20][15][21][22][16][17][23][24][25][26][27][28][29][30][31]" |
| "2. Permanent pacemaker implantation is reasonable for an incidental finding at electrophysiological study of a markedly prolonged HV interval (greater than or equal to 100 milliseconds) in asymptomatic patients. (Level of Evidence: B)[17]" |
| "3. Permanent pacemaker implantation is reasonable for an incidental finding at electrophysiological study of pacing-induced infra-His block that is not physiological. (Level of Evidence: B)[29]" |
| Class IIb |
| "1. Permanent pacemaker implantation may be considered in the setting of neuromuscular diseases such as myotonic muscular dystrophy, Erb dystrophy (limb-girdle muscular dystrophy), and peroneal muscular atrophy with bifascicular block or any fascicular block, with or without symptoms. (Level of Evidence: C)[32][33][34][35][36][37][38]" |
Sources
- The ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities [2]
References
- ↑ Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO, Tracy CM, Epstein AE, Darbar D, DiMarco JP, Dunbar SB, Estes NA, Ferguson TB, Hammill SC, Karasik PE, Link MS, Marine JE, Schoenfeld MH, Shanker AJ, Silka MJ, Stevenson LW, Stevenson WG, Varosy PD (2013). "2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society". J. Am. Coll. Cardiol. 61 (3): e6–75. doi:10.1016/j.jacc.2012.11.007. PMID 23265327.
- ↑ 2.0 2.1 2.2 Epstein AE, DiMarco JP, Ellenbogen KA, Estes NAM III, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices). Circulation. 2008; 117: 2820–2840. PMID 18483207
- ↑ FRIEDBERG CK, DONOSO E, STEIN WG (1964). "NONSURGICAL ACQUIRED HEART BLOCK". Ann N Y Acad Sci. 111: 835–47. PMID 14206803.
- ↑ "Recommendations for pacemaker prescription for symptomatic bradycardia. Report of a working party of the British Pacing and Electrophysiology Group". Br Heart J. 66 (2): 185–91. 1991. PMC 1024617. PMID 1883673.
- ↑ GADBOYS HL, WISOFF G, LITWAK RS (1964). "SURGICAL TREATMENT OF COMPLETE HEART BLOCK. AN ANALYSIS OF 36 CASES". JAMA. 189: 97–102. PMID 14149997.
- ↑ Johansson BW (1966). "Complete heart block. A clinical, hemodynamic and pharmacological study in patients with and without an artificial pacemaker". Acta Med Scand Suppl. 451: 1–127. PMID 5223645.
- ↑ Hindman MC, Wagner GS, JaRo M, Atkins JM, Scheinman MM, DeSanctis RW; et al. (1978). "The clinical significance of bundle branch block complicating acute myocardial infarction. 2. Indications for temporary and permanent pacemaker insertion". Circulation. 58 (4): 689–99. PMID 688580.
- ↑ Donmoyer TL, DeSanctis RW, Austen WG (1967). "Experience with implantable pacemakers using myocardial electrodes in the management of heart block". Ann Thorac Surg. 3 (3): 218–27. PMID 4951735.
- ↑ LEVINE SA, MILLER H, PENTON GB (1956). "Some clinical features of complete heart block". Circulation. 13 (6): 801–24. PMID 13356435.
- ↑ Dhingra RC, Denes P, Wu D, Chuquimia R, Rosen KM (1974). "The significance of second degree atrioventricular block and bundle branch block. Observations regarding site and type of block". Circulation. 49 (4): 638–46. PMID 4817704.
- ↑ DONOSO E, ADLER LN, FRIEDBERG CK (1964). "UNUSUAL FORMS OF SECOND-DEGREE ATRIOVENTRICULAR BLOCK, INCLUDING MOBITZ TYPE-II BLOCK, ASSOCIATED WITH THE MORGAGNI-ADAMS-STOKES SYNDROME". Am Heart J. 67: 150–7. PMID 14118480.
- ↑ Ranganathan N, Dhurandhar R, Phillips JH, Wigle ED (1972). "His Bundle electrogram in bundle-branch block". Circulation. 45 (2): 282–94. PMID 5009474.
- ↑ 13.0 13.1 Dhingra RC, Denes P, Wu D, Chuquimia R, Amat-y-Leon F, Wyndham C; et al. (1974). "Syncope in patients with chronic bifascicular block. Significance, causative mechanisms, and clinical implications". Ann Intern Med. 81 (3): 302–6. PMID 4854561.
- ↑ 14.0 14.1 14.2 Scheinman MM, Peters RW, Modin G, Brennan M, Mies C, O'Young J (1977). "Prognostic value of infranodal conduction time in patients with chronic bundle branch block". Circulation. 56 (2): 240–4. PMID 872316.
- ↑ 15.0 15.1 15.2 McAnulty JH, Kauffman S, Murphy E, Kassebaum DG, Rahimtoola SH (1978). "Survival in patients with intraventricular conduction defects". Arch Intern Med. 138 (1): 30–5. PMID 619828.
- ↑ 16.0 16.1 16.2 McAnulty JH, Rahimtoola SH, Murphy E, DeMots H, Ritzmann L, Kanarek PE; et al. (1982). "Natural history of "high-risk" bundle-branch block: final report of a prospective study". N Engl J Med. 307 (3): 137–43. doi:10.1056/NEJM198207153070301. PMID 7088050.
- ↑ 17.0 17.1 17.2 17.3 Scheinman MM, Peters RW, Suavé MJ, Desai J, Abbott JA, Cogan J; et al. (1982). "Value of the H-Q interval in patients with bundle branch block and the role of prophylactic permanent pacing". Am J Cardiol. 50 (6): 1316–22. PMID 7148708.
- ↑ Kulbertus H, Collignon P (1969). "Association of right bundle-branch block with left superior or inferior intraventricular block. Its relation to complete heart block and Adams-Stokes syndrome". Br Heart J. 31 (4): 435–40. PMC 487515. PMID 5791121.
- ↑ DePasquale NP, Bruno MS (1973). "Natural history of combined right bundle branch block and left anterior hemiblock (bilateral bundle branch block)". Am J Med. 54 (3): 297–303. PMID 4689232.
- ↑ Denes P, Dhingra RC, Wu D, Wyndham CR, Amat-y-Leon F, Rosen KM (1977). "Sudden death in patients with chronic bifascicular block". Arch Intern Med. 137 (8): 1005–10. PMID 879938.
- ↑ Peters RW, Scheinman MM, Modin C, O'Young J, Somelofski CA, Mies C (1979). "Prophylactic permanent pacemakers for patients with chronic bundle branch block". Am J Med. 66 (6): 978–85. PMID 453228.
- ↑ Fisch GR, Zipes DP, Fisch C (1980). "Bundle branch block and sudden death". Prog Cardiovasc Dis. 23 (3): 187–224. PMID 7001541.
- ↑ Morady F, Higgins J, Peters RW, Schwartz AB, Shen EN, Bhandari A; et al. (1984). "Electrophysiologic testing in bundle branch block and unexplained syncope". Am J Cardiol. 54 (6): 587–91. PMID 6475778.
- ↑ Click RL, Gersh BJ, Sugrue DD, Holmes DR, Wood DL, Osborn MJ; et al. (1987). "Role of invasive electrophysiologic testing in patients with symptomatic bundle branch block". Am J Cardiol. 59 (8): 817–23. PMID 3825942.
- ↑ Ezri M, Lerman BB, Marchlinski FE, Buxton AE, Josephson ME (1983). "Electrophysiologic evaluation of syncope in patients with bifascicular block". Am Heart J. 106 (4 Pt 1): 693–7. PMID 6613815.
- ↑ Twidale N, Heddle WF, Ayres BF, Tonkin AM (1988). "Clinical implications of electrophysiology study findings in patients with chronic bifascicular block and syncope". Aust N Z J Med. 18 (7): 841–7. PMID 3250407.
- ↑ Englund A, Bergfeldt L, Rehnqvist N, Aström H, Rosenqvist M (1995). "Diagnostic value of programmed ventricular stimulation in patients with bifascicular block: a prospective study of patients with and without syncope". J Am Coll Cardiol. 26 (6): 1508–15. doi:10.1016/0735-1097(95)00354-1. PMID 7594078.
- ↑ Probst P, Pachinger O, Akbar Murad A, Leisch F, Kaindl F (1979). "The HQ time in congestive cardiomyopathies". Am Heart J. 97 (4): 436–41. PMID 425877.
- ↑ 29.0 29.1 Dhingra RC, Wyndham C, Bauernfeind R, Swiryn S, Deedwania PC, Smith T; et al. (1979). "Significance of block distal to the His bundle induced by atrial pacing in patients with chronic bifascicular block". Circulation. 60 (7): 1455–64. PMID 498473.
- ↑ Cheng TO (1971). "Atrial pacing: its diagnostic and therapeutic applications". Prog Cardiovasc Dis. 14 (2): 230–47. PMID 4937704.
- ↑ Brignole M, Menozzi C, Moya A, Garcia-Civera R, Mont L, Alvarez M; et al. (2001). "Mechanism of syncope in patients with bundle branch block and negative electrophysiological test". Circulation. 104 (17): 2045–50. PMID 11673344.
- ↑ Perloff JK, Stevenson WG, Roberts NK, Cabeen W, Weiss J (1984). "Cardiac involvement in myotonic muscular dystrophy (Steinert's disease): a prospective study of 25 patients". Am J Cardiol. 54 (8): 1074–81. PMID 6496328.
- ↑ Hiromasa S, Ikeda T, Kubota K, Hattori N, Nishimura M, Watanabe Y; et al. (1987). "Myotonic dystrophy: ambulatory electrocardiogram, electrophysiologic study, and echocardiographic evaluation". Am Heart J. 113 (6): 1482–8. PMID 3591615.
- ↑ Stevenson WG, Perloff JK, Weiss JN, Anderson TL (1990). "Facioscapulohumeral muscular dystrophy: evidence for selective, genetic electrophysiologic cardiac involvement". J Am Coll Cardiol. 15 (2): 292–9. PMID 2299071.
- ↑ JAMES TN, FISCH C (1963). "OBSERVATIONS ON THE CARDIOVASCULAR INVOLVEMENT IN FRIEDREICH'S ATAXIA". Am Heart J. 66: 164–75. PMID 14051182.
- ↑ Roberts NK, Perloff JK, Kark RA (1979). "Cardiac conduction in the Kearns-Sayre syndrome (a neuromuscular disorder associated with progressive external ophthalmoplegia and pigmentary retinopathy). Report of 2 cases and review of 17 published cases". Am J Cardiol. 44 (7): 1396–400. PMID 506943.
- ↑ Charles R, Holt S, Kay JM, Epstein EJ, Rees JR (1981). "Myocardial ultrastructure and the development of atrioventricular block in Kearns-Sayre syndrome". Circulation. 63 (1): 214–9. PMID 7438396.
- ↑ JAMES TN (1962). "Observations on the cardiovascular involvement, including the cardiac conduction system, in progressive muscular dystrophy". Am Heart J. 63: 48–56. PMID 14451031.