Basal cell carcinoma pathophysiology: Difference between revisions
No edit summary |
|||
| Line 2: | Line 2: | ||
{{Basal cell carcinoma}} | {{Basal cell carcinoma}} | ||
{{CMG}};{{AE}}{{SM}} | {{CMG}};{{AE}}{{SM}} | ||
==Overview== | |||
Basal cell carcinomas develop in the [[basal cell layer]] of the [[skin]]. Cumulative DNA damage leads to [[mutation]]s, after sunlight exposure. | |||
==Pathophysiology== | ==Pathophysiology== | ||
Basal cell carcinomas develop in the [[basal cell layer]] of the [[skin]]. | Basal cell carcinomas develop in the [[basal cell layer]] of the [[skin]]. Sunlight exposure leads to the formation of [[thymine dimer]]s, a form of DNA damage. | ||
While [[DNA repair]] removes most UV-induced damage, not all crosslinks are excised. There is, therefore, cumulative DNA damage leading to [[mutation]]s. Apart from the mutagenesis, sunlight depresses the local [[immune system]], possibly decreasing immune surveillance for new tumor cells. | While [[DNA repair]] removes most UV-induced damage, not all crosslinks are excised. There is, therefore, cumulative DNA damage leading to [[mutation]]s. Apart from the mutagenesis, sunlight depresses the local [[immune system]], possibly decreasing immune surveillance for new tumor cells. | ||
| Line 15: | Line 18: | ||
[[Image:Basalioma.jpg|200px]] | [[Image:Basalioma.jpg|200px]] | ||
===Microscopic Pathology=== | ===Microscopic Pathology=== | ||
| Line 33: | Line 35: | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Dermatology]] | [[Category:Dermatology]] | ||
| Line 45: | Line 40: | ||
[[Category:Pathology]] | [[Category:Pathology]] | ||
[[Category:Oncology]] | [[Category:Oncology]] | ||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
Revision as of 19:19, 28 July 2015
|
Basal cell carcinoma Microchapters |
|
Diagnosis |
|---|
|
Case Studies |
|
Basal cell carcinoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Basal cell carcinoma pathophysiology |
|
Risk calculators and risk factors for Basal cell carcinoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Shivali Marketkar, M.B.B.S. [2]
Overview
Basal cell carcinomas develop in the basal cell layer of the skin. Cumulative DNA damage leads to mutations, after sunlight exposure.
Pathophysiology
Basal cell carcinomas develop in the basal cell layer of the skin. Sunlight exposure leads to the formation of thymine dimers, a form of DNA damage.
While DNA repair removes most UV-induced damage, not all crosslinks are excised. There is, therefore, cumulative DNA damage leading to mutations. Apart from the mutagenesis, sunlight depresses the local immune system, possibly decreasing immune surveillance for new tumor cells.
Basal-cell carcinoma also develops as a result of basal-cell nevus syndrome, or Gorlin's syndrome, which is also characterized by odontogenic keratocysts of the jaw, palmar or plantar (sole of the foot) pits, calcification of the falx cerebri (in the center line of the brain) and rib abnormalities.
The cause of the syndrome is a mutation in the PTCH1 tumor-suppressor gene at chromosome 9q22.3, which inhibits the hedgehog signaling pathway. A mutation in the SMO gene, which is also on the hedgehog pathway, also causes basal-cell carcinoma.[1]
Gross Pathology
Basal cell carcinoma in a 75 year old male.
Microscopic Pathology
Shown below is a classic micrograph of basal cell carcinoma(H&E stain).The features seen are:
- Peripheral palisading
- Myxoid stroma
- Artefactual clefting
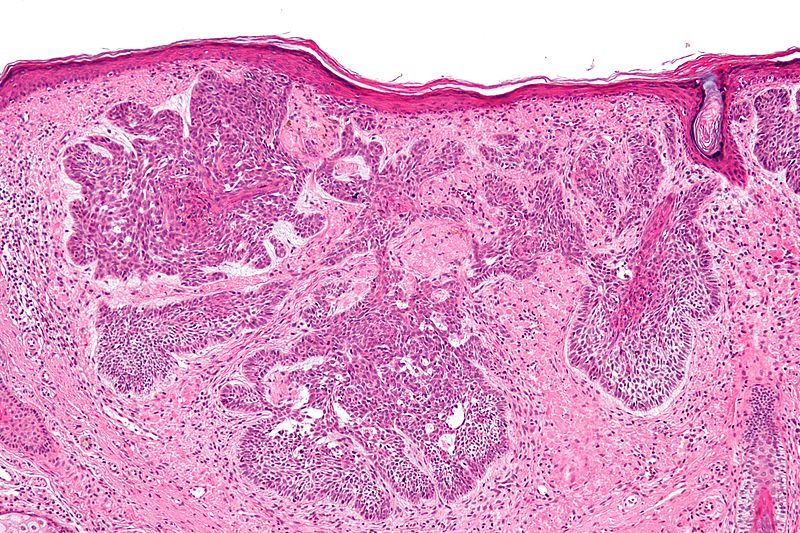
Shown below is the image of nodular variant of Basal cell carcinoma

Video
{{#ev:youtube|JnJXrFnvOKs}}
References
- ↑ Epstein EH, Shepard JA, Flotte TJ (2008). "Case records of the Massachusetts General Hospital. Case 3-2008. An 80-year-old woman with cutaneous basal-cell carcinomas and cysts of the jaws". N Engl J Med. 358 (4): 393–401. doi:10.1056/NEJMcpc0707893. PMID 18216361. Unknown parameter
|month=ignored (help)
