Basal cell carcinoma medical therapy
|
Basal cell carcinoma Microchapters |
|
Diagnosis |
|---|
|
Case Studies |
|
Basal cell carcinoma medical therapy On the Web |
|
American Roentgen Ray Society Images of Basal cell carcinoma medical therapy |
|
Risk calculators and risk factors for Basal cell carcinoma medical therapy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Saarah T. Alkhairy, M.D.
Overview
After the suspicious lesion is evaluated, the medical therapy is divided into low-risk and high-risk basal cell carcinoma patients. Medical therapy consists of surgery, radiation therapy, and follow-up for recurrence.
Basal Cell Carcinoma Medical Therapy
After the suspicious lesion is evaluated, the medical therapy is divided into low-risk and high-risk basal cell carcinoma patients.
The table below summarizes the characteristics in low-risk and high-risk lesions[1].
| H&P | Low Risk | High Risk |
| Location/size | Area L < 20 mm; Area M < 10 mm; Area H < 6 mm | Area L ≥ 20 mm; Area M ≥ 10 mm; Area H ≥ 6 mm |
| Borders | Well defined | Poorly defined |
| Primary vs. recurrent | Primary | Recurrent |
| Immunosuppression | (-) | (+) |
| Site of prior radiation therapy | (-) | (+) |
| Subtype | Nodular, superficial | Aggressive growth pattern |
| Perineural involvement | (-) | (+) |
Area H = “mask areas” of face (central face, eyelids, eyebrows, periorbital, nose, lips [cutaneous and vermilion], chin, mandible, preauricular and postauricular skin/sulci, temple, ear), genitalia, hands, and feet
Area M = cheeks, forehead, scalp, neck, and pre-tibial area
Area L = trunk and extremities (excluding pre-tibial area, hands, feet, nail units, and ankles)
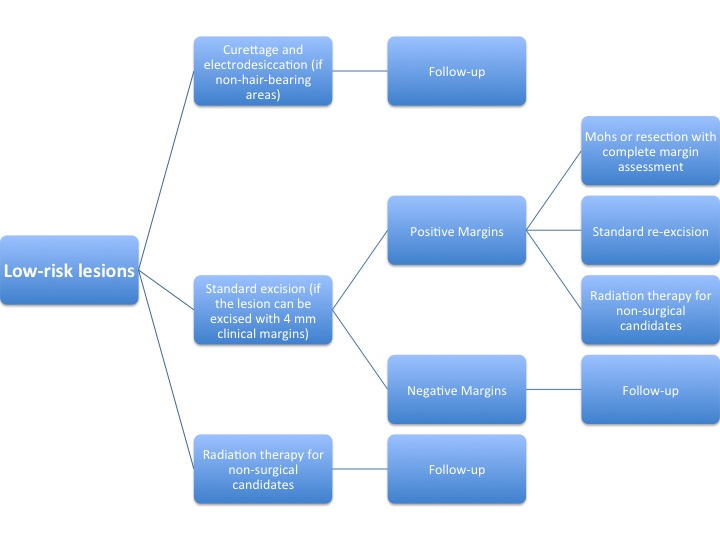
The algorithm below demonstrates a treatment protocol for low-risk lesions[2].
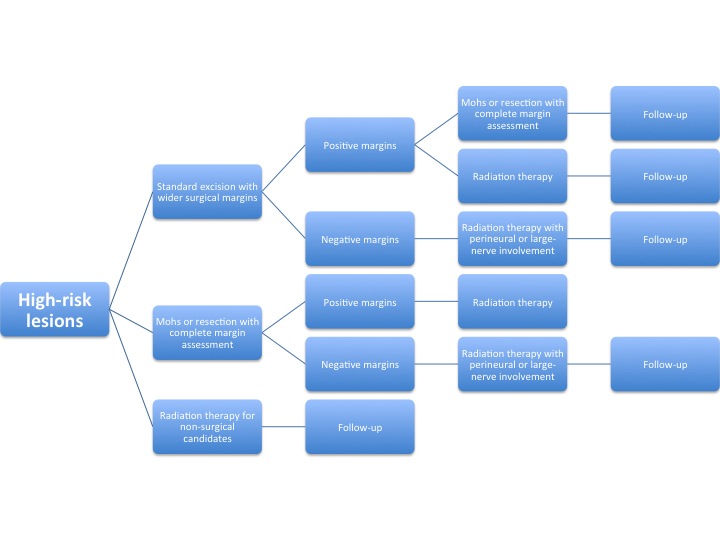
The algorithm below demonstrates a treatment protocol for high-risk lesions[3].
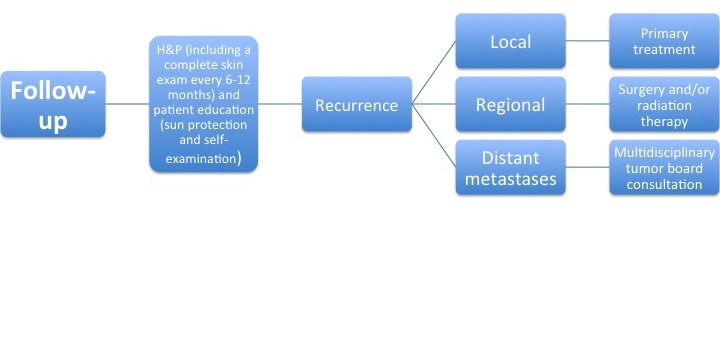
After the primary treatment, a follow-up is performed to evaluate for recurrence of the tumor.
The algorithm below demonstrates a follow-up protocol[4].
Other medical therapy techniques include the following:
- Oral vismodegib - was approved by the FDA in January 2012 for adult patients with locally advanced basal cell carcinoma who are not candidates for surgery or radiation
- Radiotherapy - used in elderly patients with extensive lesions when surgery is inappropriate
- Topical photodynamic therapy - particularly for the management of superficial BCC that involves the application of a topical emulsion-based 5-aminolaevulinic acid
- Fluorouracil - particularly for the management of multiple superficial BCC on the trunk and limbs
- Imiquimod - particularly for the management of superficial BCC