|
|
| (5 intermediate revisions by 2 users not shown) |
| Line 1: |
Line 1: |
| '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' |
|
| |
| {{Infobox Disease | | | {{Infobox Disease | |
| Name = Baker's cyst | | | Name = Baker's cyst | |
| Line 17: |
Line 16: |
| {{Baker's cyst}} | | {{Baker's cyst}} |
| {{CMG}} | | {{CMG}} |
| | ==[[Baker's cyst overview|Overview]]== |
|
| |
|
| ==Overview== | | ==[[Baker's cyst historical perspective|Historical Perspective]]== |
| A '''Baker's cyst''', otherwise known as a [[popliteal]] [[cyst]], is a benign swelling found behind the [[knee]] [[joint]].
| |
| | |
| ==Etymology==
| |
| It is named after the [[surgery|surgeon]] who first described it, Dr. William Morrant Baker (1839-1896).<ref>{{cite web | title=William Morrant Baker | url=http://www.whonamedit.com/doctor.cfm/649.html | publisher=[[Who Named It]]}}</ref>
| |
|
| |
|
| ==Etiology== | | ==[[Baker's cyst classification|Classification]]== |
| In adults, Baker's cysts usually arise from almost any form of knee [[arthritis]] and [[cartilage]] (particularly the meniscus) tear. Baker's cysts in children do not point to underlying joint disease. Baker's cysts arise between the tendons of the medial head of the gastrocnemius and the semimembranosus muscles. They are posterior to the medial femoral condyle.
| |
|
| |
|
| The [[synovium|synovial]] sack of the knee joint can, under certain circumstances, produce a posterior bulge, into the popliteal space, the space behind the knee. When this bulge becomes large enough, it becomes palpable and cystic. Most Baker's cysts maintain this direct communication with the synovial cavity of the knee, but sometimes, the new cyst pinches off. A Baker's cyst can rupture and produce acute pain behind the knee and in the calf and swelling of the calf muscles.
| | ==[[Baker's cyst pathophysiology|Pathophysiology]]== |
|
| |
|
| As a summary:
| | ==[[Baker's cyst causes|Causes]]== |
|
| |
|
| *A popliteal cyst is '''fluid distention of a bursa between the gastrocnemius and semimembranosus tendons via a communication with the knee joint'''.
| | ==[[Baker's cyst differential diagnosis|Differentiating Baker's cyst from other Diseases]]== |
| *Fluid within a Baker's cyst may communicate freely with the knee joint. However, the presence of a valvelike mechanism may allow joint fluid to communicate in only one direction.
| |
| *Popliteal cysts may be seen with many joint abnormalities, such as internal derangement, osteoarthrosis, or inflammatory [[arthritis]]; the most common associations include joint effusion, meniscal tear, and degenerative joint disease.
| |
|
| |
|
| ==Diagnosis== | | ==[[Baker's cyst epidemiology and demographics|Epidemiology and Demographics]]== |
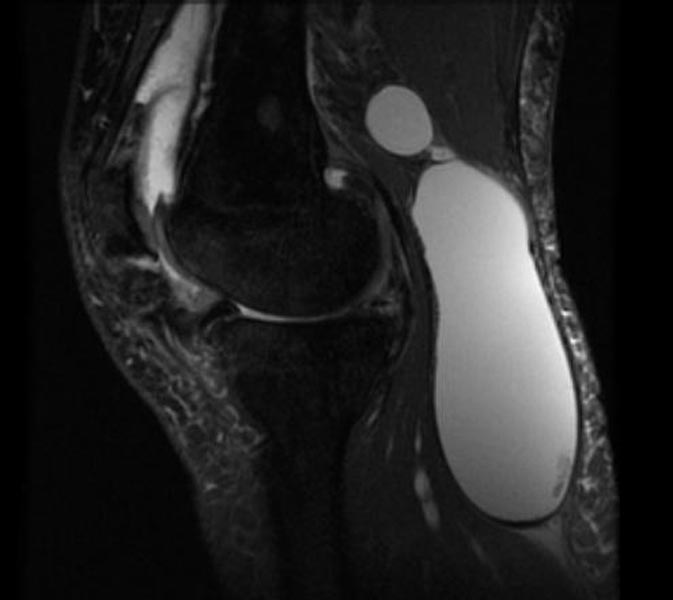
| Diagnosis is by examination. They are easier to see from behind with the patient standing with knees fully extended and then most easily felt with the knee partially flexed. Diagnosis is confirmed by [[medical ultrasonography|ultrasonography]], although if needed and there is no suspicion of a [[popliteal artery]] [[aneurysm]] then aspiration of synovial fluid from the cyst may be undertaken with care. An [[Magnetic resonance imaging|MRI]] image can reveal presence of a Baker's cyst.
| |
|
| |
|
| A burst cyst can cause calf pain, swelling and redness that may mimic [[thrombophlebitis]] or a potentially life-threatening [[deep vein thrombosis]] (DVT) which may need to be excluded by urgent blood tests and ultrasonography. Although an infrequent occurrence, a Baker's cyst can compress vascular structures and cause leg edema and a true DVT.
| | ==[[Baker's cyst risk factors|Risk Factors]]== |
|
| |
|
| (Images courtesy of RadsWiki)
| | ==[[Baker's cyst screening|Screening]]== |
|
| |
|
| <gallery>
| | ==[[Baker's cyst natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| Image:Popliteal-cyst-001.jpg|PD: A large popliteal cyst
| |
| Image:Popliteal-cyst-002.jpg|PD: A large popliteal cyst
| |
| </gallery>
| |
|
| |
|
| <gallery>
| | == Diagnosis == |
| Image:Popliteal-cyst-003.jpg|PD fat sat: A large popliteal cyst
| | [[Baker's cyst history and symptoms| History and Symptoms]] | [[Baker's cyst physical examination | Physical Examination]] | [[Baker's cyst laboratory findings | Laboratory Findings]] | [[Baker's cyst CT|CT]] | [[Baker's cyst MRI|MRI]] | [[Baker's cyst ultrasound|Ultrasound]] | [[Baker's cyst other imaging findings|Other Imaging Findings]] | [[Baker's cyst other diagnostic studies|Other Diagnostic Studies]] |
| Image:Popliteal-cyst-004.jpg|PD: A large popliteal cyst
| |
| </gallery>
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| Baker's cysts usually require no treatment unless they are symptomatic. Often rest and leg elevation are all that is needed. If necessary, the cyst can be aspirated to reduce its size, then injected with a [[corticosteroid]] to reduce inflammation. Surgical excision is reserved for cysts that cause a great amount of discomfort to the patient. A ruptured cyst is treated with rest, leg elevation, and injection of a corticosteroid into the knee. Recently, [[prolotherapy]] (in use at the [[Mayo Clinic]] since 2005) has shown encouraging results as an effective way to treat Baker's cysts and other types of musculoskeletal conditions.<ref name="pmid15864836">{{cite journal |author= |title=Alternative treatments. Dealing with chronic pain |journal=Mayo Clinic health letter (English ed.) |volume=23 |issue=4 |pages=1–3 |year=2005 |pmid=15864836 |doi=}}</ref><ref name="isbn0971450323 ">{{cite book |author=March Darrow |title=Prolotherapy: Living Pain Free |publisher=Protex Press |location= |year= |pages= |isbn=0971450323 |oclc= |doi=}}</ref> | | [[Baker's cyst medical therapy|Medical Therapy]] | [[Baker's cyst surgery|Surgery]] | [[Baker's cyst primary prevention|Primary Prevention]] | [[Baker's cyst secondary prevention|Secondary Prevention]] | [[Baker's cyst cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Baker's cyst future or investigational therapies|Future or Investigational Therapies]] |
| | |
| Baker's cysts in children, unlike in older people, nearly always disappear with time, and rarely require excision.
| |
| | |
| ==Symptomatic relief==
| |
| ===Cryotherapy===
| |
| | |
| Ice pack therapy is believed to be an effective way of controlling the pain caused by Baker's cyst. Ice must not be applied directly onto the skin but be separated by a thin cloth. Alternatively cooling packs may be used, but the total application time for any product is for no more than 15 minutes at a time.
| |
| | |
| ===Medication===
| |
| Medications bought at [[pharmacies]] may be used to help soothe pain. Painkillers with [[paracetamol]] aka [[tylenol]] (acetaminophen) or with the additional [[anti-inflammatory]] action (such as [[ibuprofen]] or [[naproxen]]) may be used. Stronger [[non-steroidal anti-inflammatory drug]]s may be required by [[medical prescription|prescription]] from one's [[general practitioner]].
| |
| | |
| ===Heat===
| |
| Heat is also a recognized treatment. The application of a [[heating pad]] on a low setting for 10-20 minutes may relieve some pain, but only if instructions are followed carefully.
| |
| | |
| ===Bracing===
| |
| A knee brace can offer support, but relieve pain by stimulating nerve fibre,<!-- braces stimulating nerves and so reduce pain - sounds nonsense, surely just that reduces flexion during walking and so less squeezing of the taut cyst--> giving the feel of stability in the joint. If only support is necessary, a simple elastic bandage is recommended; however, braces compress the back of the knee, where it is most tender, and can cause pain.
| |
| | |
| ===Rest and specific exercise===
| |
| Many activities can put strain on the knee, and cause pain in the case of Baker's cyst. Avoiding activities such as squatting, kneeling, heavy lifting, climbing, and even running can help prevent pain. Despite this, some exercises can help relieve pain, and a physiotherapist may instruct on stretching and strengthening the [[quadriceps]] and/or the [[patellar ligament]].
| |
| | |
| ==Potential Complications==
| |
| * Pseudothrombophlebitis syndrome (rupture, dissection)
| |
| * [[Deep vein thrombosis]]
| |
| * Leaking
| |
| * Infection
| |
| * Posterior compartment syndrome
| |
| * Trapped calcified bodies
| |
| | |
| ==References==
| |
| * {{cite book | author = Hellmann, DB | year = 2005| title = Current Medical Diagnosis & Treatment | chapter = Chapter 20: Arthritis & Musculoskeletal Disorders | editor = Tierney LM, Jr., McPhee SJ, Papadakis MA | edition = 44th Edition | publisher = F. A. Davis Company | location = Philadelphia, PA | id = ISBN 0-07-145323-7}}
| |
| * [http://www.jointhealing.com/pages/knee/bakers_cyst.html Joint Healing.com-Baker's Cyst]
| |
| | |
| ==Footnotes==
| |
| <references/>
| |
| | |
| ==External links==
| |
| * {{GPnotebook|302383106|Baker's cyst}}
| |
| | |
|
| |
|
| | ==[[Baker's cyst case study one|Case #1]]== |
|
| |
|
| [[Category:Surgery]] | | [[Category:Surgery]] |
| | [[Category:Orthopedics]] |
| [[Category:Musculoskeletal disorders]] | | [[Category:Musculoskeletal disorders]] |
| [[Cateogry:Orthopedics]]
| |
| [[Category:Overview complete]] | | [[Category:Overview complete]] |
|
| |
|
| [[de:Baker-Zyste]]
| |
| [[pl:Torbiel Bakera]]
| |
| [[pt:Cisto de Baker]]
| |
| {{WikiDoc Help Menu}} | | {{WikiDoc Help Menu}} |
| {{WikiDoc Sources}} | | {{WikiDoc Sources}} |