Avelumab
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Yashasvi Aryaputra[2], Anmol Pitliya, M.B.B.S. M.D.[3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
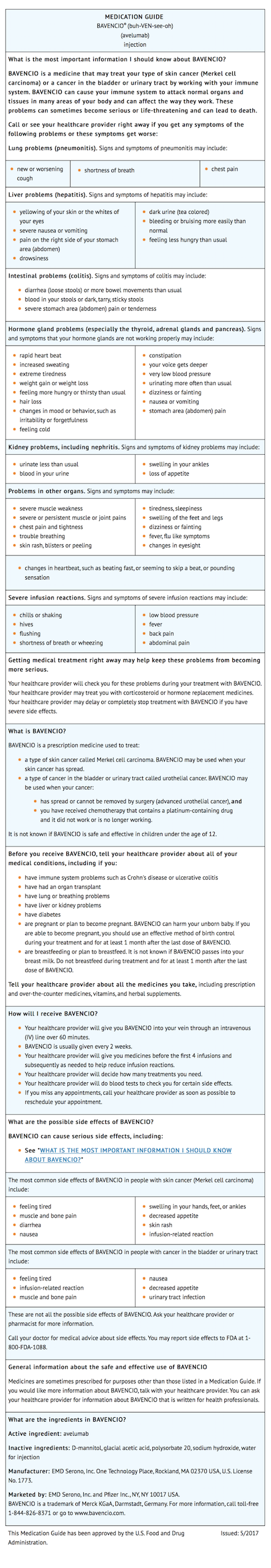
Avelumab is a programmed death ligand-1 (PD-L1) blocking antibody that is FDA approved for the treatment of adults and pediatric patients 12 years and older with metastatic Merkel cell carcinoma (MCC) and patients with locally advanced or metastatic urothelial carcinoma (UC) who have disease progression during or following platinum-containing chemotherapy or have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy. Common adverse reactions include fatigue, musculoskeletal pain, diarrhea, nausea, infusion-related reaction, rash, decreased appetite, and peripheral edema in patients with metastatic Merkel cell carcinoma. Most common adverse reactions in patients with locally advanced or metastatic urothelial carcinoma were fatigue, infusion-related reaction, musculoskeletal pain, nausea, decreased appetite, and urinary tract infection.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indication:
Metastatic Merkel Cell Carcinoma
- Avelumab is indicated for the treatment of adults and pediatric patients 12 years and older with metastatic Merkel cell carcinoma (MCC).
- This indication is approved under accelerated approval based on tumor response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
Locally Advanced or Metastatic Urothelial Carcinoma
- Avelumab is indicated for the treatment of patients with locally advanced or metastatic urothelial carcinoma (UC) who:
- Have disease progression during or following platinum-containing chemotherapy.
- Have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
- This indication is approved under accelerated approval based on tumor response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
Recommended Dosage
- The recommended dose of avelumab is 10 mg/kg administered as an intravenous infusion over 60 minutes every 2 weeks until disease progression or unacceptable toxicity.
Dose Modifications

Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding avelumab Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding avelumab Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Indication:
Metastatic Merkel Cell Carcinoma
- Avelumab is indicated for the treatment of adults and pediatric patients 12 years and older with metastatic Merkel cell carcinoma (MCC).
- This indication is approved under accelerated approval based on tumor response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
Locally Advanced or Metastatic Urothelial Carcinoma
- Avelumab is indicated for the treatment of patients with locally advanced or metastatic urothelial carcinoma (UC) who:
- Have disease progression during or following platinum-containing chemotherapy.
- Have disease progression within 12 months of neoadjuvant or adjuvant treatment with platinum-containing chemotherapy.
- This indication is approved under accelerated approval based on tumor response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
Recommended Dosage
- The recommended dose of avelumab is 10 mg/kg administered as an intravenous infusion over 60 minutes every 2 weeks until disease progression or unacceptable toxicity.
Dose Modifications

Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding avelumab Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding avelumab Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
- None
Warnings
Immune-Mediated Pneumonitis
- Avelumab can cause immune-mediated pneumonitis, including fatal cases. Monitor patients for signs and symptoms of pneumonitis and evaluate patients with suspected pneumonitis with radiographic imaging. Administer corticosteroids (initial dose of 1 to 2 mg/kg/day prednisone or equivalent, followed by a corticosteroid taper) for Grade 2 or greater pneumonitis. Withhold avelumab for moderate (Grade 2) pneumonitis, and permanently discontinue for severe (Grade 3), life-threatening (Grade 4), or recurrent moderate (Grade 2) pneumonitis.
- Pneumonitis occurred in 1.2% (21/1738) of patients receiving avelumab including one (0.1%) patient with Grade 5, one (0.1%) with Grade 4, and five (0.3%) with Grade 3 pneumonitis. Immune-mediated pneumonitis led to permanent discontinuation of avelumab in 0.3% (6/1738) of patients. Among the 21 patients with immune-mediated pneumonitis, the median time to onset was 2.5 months (range: 3 days to 11 months) and the median duration of pneumonitis was 7 weeks (range: 4 days to 4+ months). All 21 patients were treated with systemic corticosteroids; 17 (81%) of the 21 patients received high-dose corticosteroids for a median of 8 days (range: 1 day to 2.3 months). Resolution of pneumonitis occurred in 12 (57%) of the 21 patients at the time of data cut-off.
Immune-Mediated Hepatitis
- Avelumab can cause immune-mediated hepatitis including fatal cases. Monitor patients for abnormal liver tests prior to and periodically during treatment. Administer corticosteroids (initial dose of 1 to 2 mg/kg/day prednisone or equivalent, followed by a corticosteroid taper) for Grade 2 or greater hepatitis. Withhold avelumab for moderate (Grade 2) immune-mediated hepatitis until resolution and permanently discontinue for severe (Grade 3) or life-threatening (Grade 4) immune-mediated hepatitis.
- Immune-mediated hepatitis occurred in 0.9% (16/1738) of patients receiving avelumab including two (0.1%) patients with Grade 5 and 11 (0.6 %) patients with Grade 3 immune-mediated hepatitis. Immune-mediated hepatitis led to permanent discontinuation of avelumab in 0.5% (9/1738) of patients. Among the 16 patients with immune-mediated hepatitis, the median time to onset was 3.2 months (range: 1 week to 15 months), and the median duration of hepatitis was 2.5 months (range: 1 day to 7.4+ months). All 16 patients were treated with corticosteroids; 15 (94%) of the 16 patients received high-dose corticosteroids for a median of 14 days (range: 1 day to 2.5 months). Resolution of hepatitis occurred in nine (56%) of the 16 patients at the time of data cut-off.
Immune-Mediated Colitis
- Avelumab can cause immune-mediated colitis. Monitor patients for signs and symptoms of colitis. Administer corticosteroids (initial dose of 1 to 2 mg/kg/day prednisone or equivalent followed by a corticosteroid taper) for Grade 2 or greater colitis. Withhold avelumab for moderate or severe (Grade 2 or 3) colitis until resolution. Permanently discontinue avelumab for life-threatening (Grade 4) or for recurrent (Grade 3) colitis upon re-initiation of avelumab.
- Immune-mediated colitis occurred in 1.5% (26/1738) of patients receiving avelumab including seven (0.4%) patients with Grade 3 colitis. Immune-mediated colitis led to permanent discontinuation of avelumab in 0.5% (9/1738) of patients. Among the 26 patients with immune-mediated colitis, the median time to onset was 2.1 months (range: 2 days to 11 months) and the median duration of colitis was 6 weeks (range: 1 day to 14+ months). All 26 patients were treated with corticosteroids; 15 (58%) of the 26 patients received high-dose corticosteroids for a median of 19 days (range: 1 day to 2.3 months). Resolution of colitis occurred in 18 (70%) of the patients at the time of data cut-off.
Immune-Mediated Endocrinopathies
Adrenal Insufficiency
- Monitor patients for signs and symptoms of adrenal insufficiency during and after treatment. Administer corticosteroids as appropriate for adrenal insufficiency. Withhold avelumab for severe (Grade 3) or life-threatening (Grade 4) adrenal insufficiency.
- Adrenal insufficiency occurred in 0.5% (8/1738) of patients receiving avelumab including one patient (0.1%) with Grade 3 adrenal insufficiency. Immune-mediated adrenal insufficiency led to permanent discontinuation of avelumab in 0.1% (2/1738) of patients. Among the 8 patients with immune-mediated adrenal insufficiency, the median time to onset was 2.5 months (range: 1 day to 8 months). All eight patients were treated with corticosteroids; four (50%) of the eight patients received high-dose corticosteroids for a median of 1 day (range: 1 day to 24 days).
Thyroid Disorders (Hypothyroidism/Hyperthyroidism)
- Avelumab can cause immune-mediated thyroid disorders. Thyroid disorders can occur at any time during treatment. Monitor patients for changes in thyroid function at the start of treatment, periodically during treatment, and as indicated based on clinical evaluation. Manage hypothyroidism with hormone-replacement therapy. Initiate medical management for control of hyperthyroidism. Withhold avelumab for severe (Grade 3) or life-threatening (Grade 4) thyroid disorders.
- Immune-mediated thyroid disorders occurred in 6% (98/1738) of patients receiving avelumab including 3 (0.2%) Grade 3 immune-mediated thyroid disorders. Immune-mediated thyroid disorders led to discontinuation of avelumab in 0.1% (2/1738) of patients. Hypothyroidism occurred in 90 (5%) patients; hyperthyroidism in seven (0.4%) patients; and thyroiditis in four (0.2%) patients treated with avelumab. Among the 98 patients with immune-mediated thyroid disorders, the median time to onset was 2.8 months (range: 2 weeks to 13 months) and the median duration was not estimable (range: 6 days to more than 26 months). Immune-mediated thyroid disorders resolved in seven (7%) of the 98 patients.
Type 1 Diabetes Mellitus
- Avelumab can cause type 1 diabetes mellitus, including diabetic ketoacidosis. Monitor patients for hyperglycemia or other signs and symptoms of diabetes. Withhold avelumab and administer anti-hyperglycemics or insulin in patients with severe or life-threatening (Grade ≥ 3) hyperglycemia. Resume treatment with avelumab when metabolic control is achieved on insulin replacement or anti-hyperglycemics.
- Type 1 diabetes mellitus without an alternative etiology occurred in 0.1% (2/1738) of patients including two cases of Grade 3 hyperglycemia that led to permanent discontinuation of avelumab.
Immune-Mediated Nephritis and Renal Dysfunction
- Avelumab can cause immune-mediated nephritis. Monitor patients for elevated serum creatinine prior to and periodically during treatment. Administer corticosteroids (initial dose of 1 to 2 mg/kg/day prednisone or equivalent followed by a corticosteroid taper) for Grade 2 or greater nephritis. Withhold avelumab for moderate (Grade 2) or severe (Grade 3) nephritis until resolution to ≤ Grade 1. Permanently discontinue avelumab for life-threatening (Grade 4) nephritis.
- Immune-mediated nephritis occurred in 0.1% (1/1738) of patients receiving avelumab; avelumab was permanently discontinued in this patient.
Other Immune-Mediated Adverse Reactions
- Avelumab can result in severe and fatal immune-mediated adverse reactions. These immune-mediated reactions may involve any organ system. Most immune-mediated reactions initially manifest during treatment with avelumab; however, immune-mediated adverse reactions can occur after discontinuation of avelumab.
- For suspected immune-mediated adverse reactions, evaluate to confirm or rule out an immune-mediated adverse reaction and to exclude other causes. Depending upon the severity of the adverse reaction, withhold or permanently discontinue avelumab, administer high dose corticosteroids, and if appropriate, initiate hormone replacement therapy. Upon improvement to Grade 1 or less, initiate corticosteroid taper. Resume avelumab when the immune-mediated adverse reaction remains at Grade 1 or less following corticosteroid taper. Permanently discontinue avelumab for any severe (Grade 3) immune-mediated adverse reaction that recurs and for any life-threatening immune-mediated adverse reaction.
- The following clinically significant, immune-mediated adverse reactions occurred at an incidence of less than 1% of 1738 patients treated with avelumab for each of the following adverse reactions: immune-mediated myocarditis including fatal cases, immune-mediated myositis, psoriasis, arthritis, exfoliative dermatitis, erythema multiforme, pemphigoid, hypopituitarism, uveitis, Guillain-Barré syndrome, and systemic inflammatory response. The following clinically significant, immune-mediated adverse reactions have been reported with other products in this class: bullous dermatitis, Stevens Johnson Syndrome (SJS)/toxic epidermal necrolysis (TEN), pancreatitis, rhabdomyolysis, myasthenia gravis, histiocytic necrotizing lymphadenitis, demyelination, vasculitis, hemolytic anemia, hypophysitis, iritis, and encephalitis.
Infusion-Related Reactions
- Avelumab can cause severe or life-threatening infusion-related reactions. Premedicate with antihistamine and acetaminophen prior to the first 4 infusions. Monitor patients for signs and symptoms of infusion-related reactions including pyrexia, chills, flushing, hypotension, dyspnea, wheezing, back pain, abdominal pain, and urticaria. Interrupt or slow the rate of infusion for mild or moderate infusion-related reactions. Stop the infusion and permanently discontinue avelumab for severe (Grade 3) or life-threatening (Grade 4) infusion-related reactions.
- Infusion-related reactions occurred in 25% (439/1738) of patients treated with avelumab including three (0.2%) Grade 4 and nine (0.5%) Grade 3 infusion-related reactions. Ninety-three percent (1615/1738) of patients received premedication with antihistamine and acetaminophen. Eleven (92%) of the 12 patients with Grade ≥ 3 reactions were treated with intravenous corticosteroids. Fourteen percent of patients (252/1738) had infusion-related reactions that occurred after the avelumab infusion was completed.
Embryo-Fetal Toxicity
- Based on its mechanism of action, avelumab can cause fetal harm when administered to a pregnant woman. Animal studies have demonstrated that inhibition of the PD-1/PD-L1 pathway can lead to increased risk of immune-mediated rejection of the developing fetus resulting in fetal death. If this drug is used during pregnancy, or if the patient becomes pregnant while taking avelumab, inform the patient of the potential risk to a fetus. Advise females of childbearing potential to use effective contraception during treatment with avelumab and for at least one month after the last dose of avelumab.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The data described in the WARNINGS AND PRECAUTIONS section are based on two trials, in which 1738 patients received avelumab at doses of 10 mg/kg intravenously every two weeks. This included 88 patients with metastatic MCC (JAVELIN Merkel 200 trial) and 242 patients with locally advanced and metastatic UC within the JAVELIN Solid Tumor trial. In the JAVELIN Solid Tumor trial, 1650 patients were treated with avelumab at doses of 10 mg/kg.
- The following criteria were used to classify an adverse reaction as immune-mediated: onset within 90 days after last dose of avelumab, no spontaneous resolution within 7 days of onset, treatment with corticosteroids or other immunosuppressant or hormone replacement therapy, biopsy consistent with immune-mediated reaction, and no other clear etiology.
- The study population characteristics of the 1738 patients were median age of 64 years (range: 19 to 91 years); 52% male; 78% White, 9% Asian, 5% Black or African American, and 8% other ethnic groups; ECOG performance score of 0 (38%), 1 (62%), or > 1 (0.4%); and the underlying malignancies were non-small cell lung cancer (20%), gastric and gastroesophageal cancer (15%), urothelial cancer (14%), ovarian cancer (13%), metastatic breast cancer (10%), head and neck cancer (9%), metastatic MCC (5%), mesothelioma, renal cell carcinoma, melanoma, adrenocortical carcinoma (3% each), colorectal cancer, castrate-resistant prostate cancer, and unknown (1% each). In this population, 24% of patients were exposed to avelumab for ≥ 6 months and 7% were exposed to avelumab for ≥ 12 months.
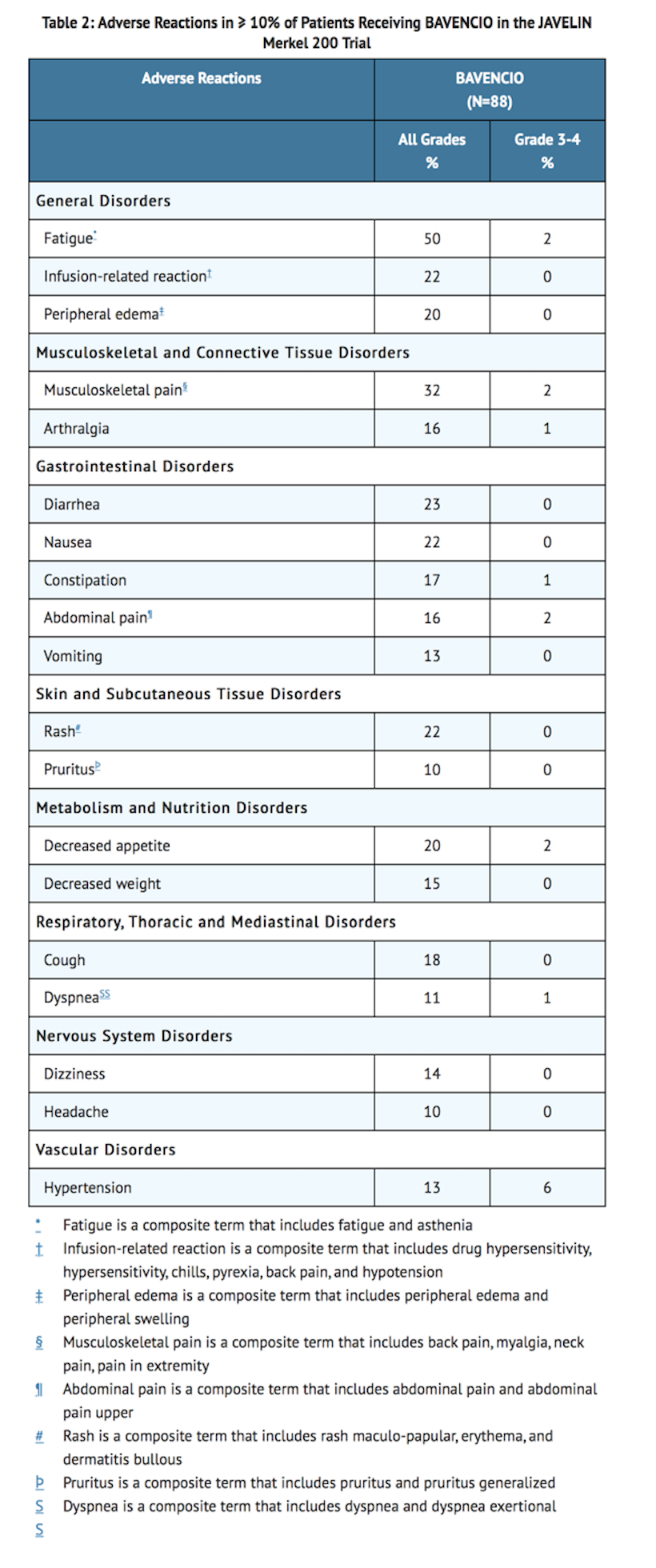
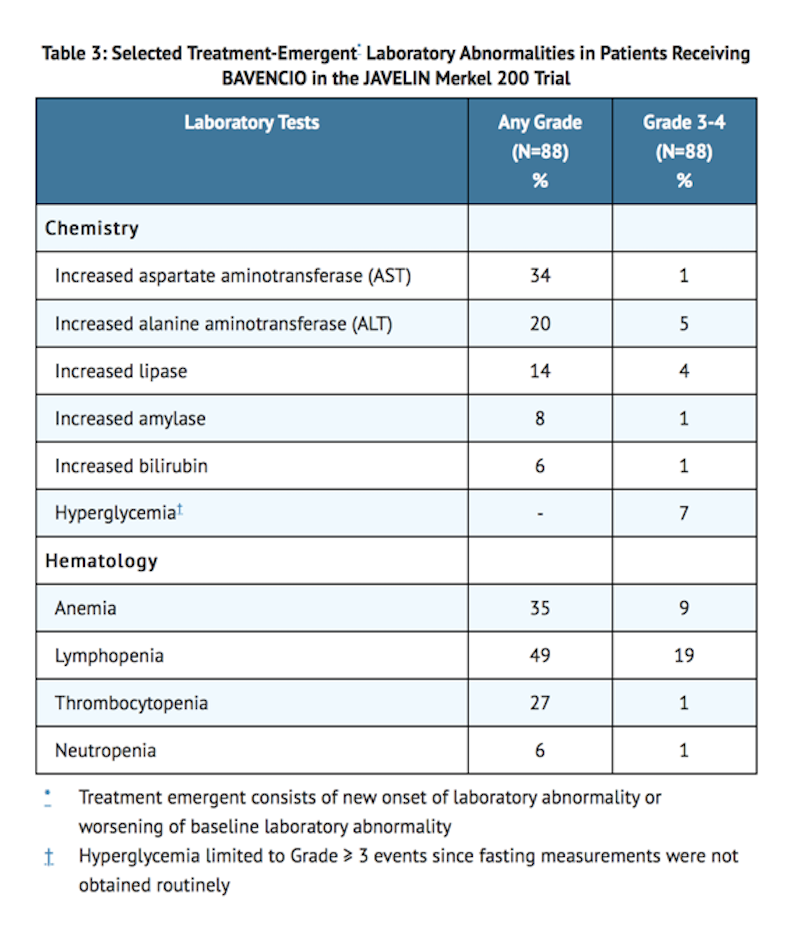
Metastatic Merkel Cell Carcinoma
- The data described below reflect exposure to avelumab 10 mg/kg intravenously every 2 weeks in 88 patients with metastatic MCC enrolled in the JAVELIN Merkel 200 trial. Patients with any of the following were excluded: autoimmune disease; medical conditions requiring systemic immunosuppression; prior organ or allogeneic stem cell transplantation; prior treatment with anti-PD-1, anti-PD-L1, or anti-CTLA-4 antibodies; central nervous system (CNS) metastases; infection with HIV, hepatitis B, or hepatitis C; or ECOG performance score ≥ 2.
- The median duration of exposure to avelumab was 4 months (range: 2 weeks to 21 months). Forty percent of patients received avelumab for more than 6 months and 14% were treated for more than one year. The study population characteristics were: median age of 73 years (range: 33 to 88), 74% male, 92% White, ECOG performance score of 0 (56%) or 1 (44%), and 65% of patients had one prior anti-cancer therapy for metastatic MCC and 35% had two or more prior therapies.
- Avelumab was permanently discontinued for adverse reactions in six (7%) patients; adverse reactions resulting in permanent discontinuation were ileus, Grade 3 transaminitis, Grade 3 creatine kinase elevation, tubulointerstitial nephritis, and Grade 3 pericardial effusion. Avelumab was temporarily discontinued in 21 (24%) patients for adverse events, excluding temporary dose interruption for infusion-related reactions where infusion was restarted the same day. The most common adverse reaction requiring dose interruption was anemia. Serious adverse reactions that occurred in more than one patient were acute kidney injury, anemia, abdominal pain, ileus, asthenia, and cellulitis. The most common adverse reactions (≥ 20%) were fatigue, musculoskeletal pain, diarrhea, nausea, infusion-related reaction, rash, decreased appetite, and peripheral edema.
- Table 2 and Table 3 summarize the incidence of adverse reactions and laboratory abnormalities, respectively, that occurred in patients receiving avelumab.
Locally Advanced or Metastatic Urothelial Carcinoma
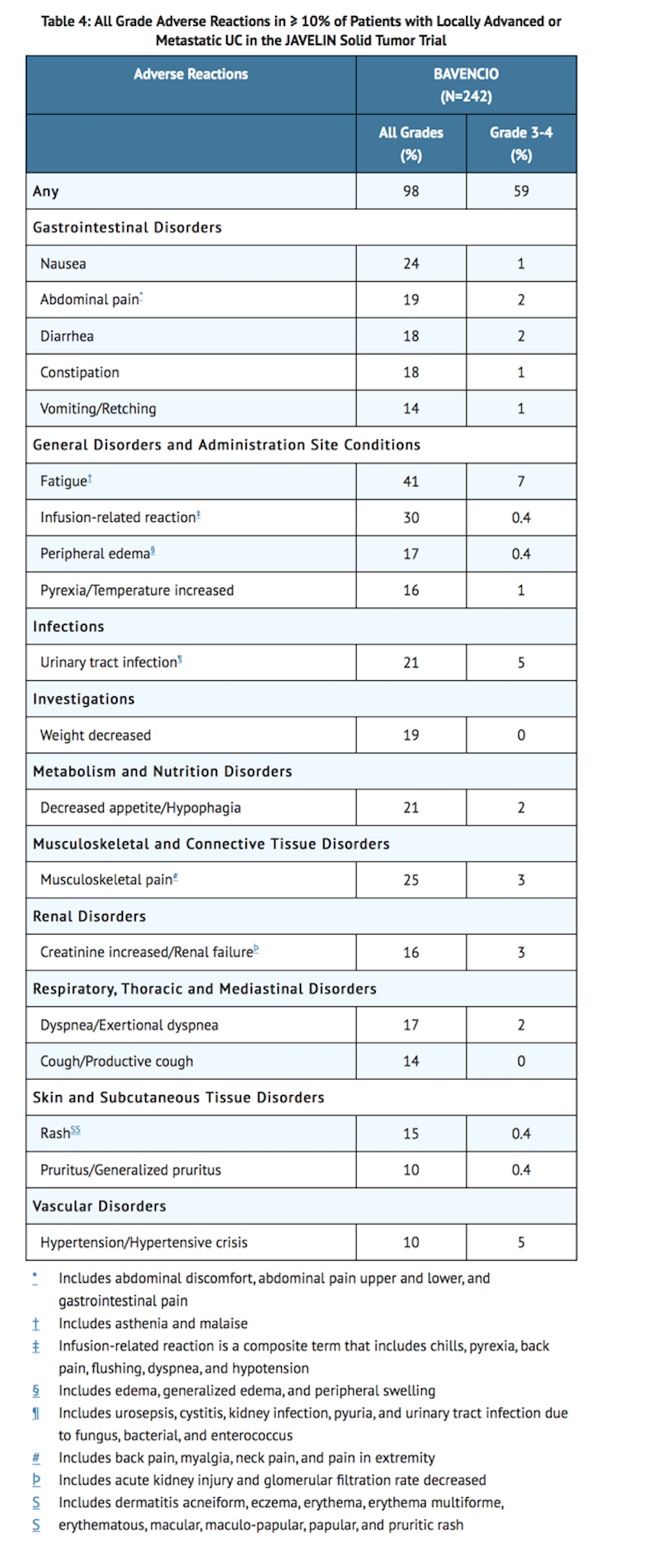
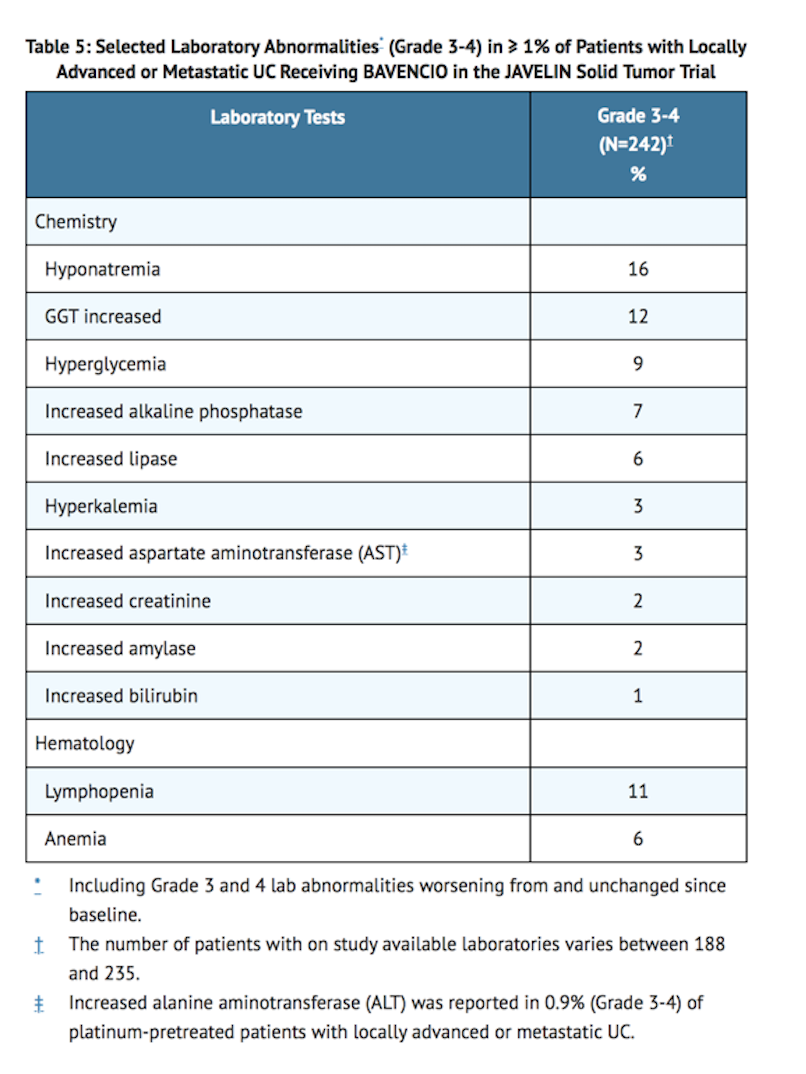
- Table 4 describes adverse reactions reported in 242 patients with locally advanced or metastatic UC receiving avelumab at 10 mg/kg every 2 weeks in the UC cohorts of the JAVELIN Solid Tumor trial. Patients received pre-medication with an anti-histamine and acetaminophen prior to each infusion. The median duration of exposure to avelumab was 12 weeks (range: 2 weeks to 92 weeks).
- Fourteen patients (6%) who were treated with avelumab experienced either pneumonitis, respiratory failure, sepsis/urosepsis, cerebrovascular accident, or gastrointestinal adverse events, which led to death.
- Avelumab was permanently discontinued for Grade 1-4 adverse reactions in 30 (12%) patients. The adverse reaction that resulted in permanent discontinuation in > 1% of patients was fatigue. Avelumab was temporarily discontinued in 29% of patients for adverse reactions, excluding temporary dose interruption for infusion-related reactions where infusion was restarted the same day. The adverse reactions that resulted in temporary discontinuation in > 1% of patients were diarrhea, fatigue, dyspnea, urinary tract infection, and rash.
- Grade 1-4 serious adverse reactions were reported in 41% of patients. The most frequent serious adverse reactions reported in ≥ 2% of patients were urinary tract infection/urosepsis, abdominal pain, musculoskeletal pain, creatinine increased/renal failure, dehydration, hematuria/urinary tract hemorrhage, intestinal obstruction/small intestine obstruction, and pyrexia.
- The most common Grade 3 and 4 adverse reactions (≥ 3%) were anemia, fatigue, hyponatremia, hypertension urinary tract infection, and musculoskeletal pain.
- The most common adverse reactions (≥ 20%) were fatigue, infusion-related reaction, musculoskeletal pain, nausea, decreased appetite, and urinary tract infection.
- Eleven (4.5%) patients received an oral prednisone dose equivalent to ≥ 40 mg daily for an immune-mediated adverse reaction.
- Table 4 summarizes the adverse reactions that occurred in at least 10% of patients with locally advanced or metastatic UC receiving avelumab while Table 5 summarizes selected Grade 3-4 laboratory abnormalities that occurred in ≥ 1% of patients treated with avelumab.
Immunogenicity
- As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to avelumab in the studies described below with the incidence of antibodies in other studies or to other products may be misleading.
- Of the 1738 patients treated with avelumab 10 mg/kg as an intravenous infusion every 2 weeks, 1558 were evaluable for treatment-emergent anti-drug antibodies (ADA) and 64 (4.1%) tested positive. The development of treatment-emergent ADA against avelumab did not appear to alter the pharmacokinetic profile or risk of infusion-related reactions.
Postmarketing Experience
There is limited information regarding Avelumab Postmarketing Experience in the drug label.
Drug Interactions
There is limited information regarding Avelumab Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
- Risk Summary
- Based on its mechanism of action, avelumab can cause fetal harm when administered to a pregnant woman. There are no available data on the use of avelumab in pregnant women. Animal studies have demonstrated that inhibition of the PD-1/PD-L1 pathway can lead to increased risk of immune-mediated rejection of the developing fetus resulting in fetal death [see DATA]. Human IgG1 immunoglobulins (IgG1) are known to cross the placenta. Therefore, avelumab has the potential to be transmitted from the mother to the developing fetus. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, advise the patient of the potential risk to a fetus.
- In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
- Data (Animal Data)
- Animal reproduction studies have not been conducted with avelumab to evaluate its effect on reproduction and fetal development. A central function of the PD-1/PD-L1 pathway is to preserve pregnancy by maintaining maternal immune tolerance to the fetus. In murine models of pregnancy, blockade of PD-L1 signaling has been shown to disrupt tolerance to the fetus and to result in an increase in fetal loss; therefore, potential risks of administering avelumab during pregnancy include increased rates of abortion or stillbirth. As reported in the literature, there were no malformations related to the blockade of PD-1/PD-L1 signaling in the offspring of these animals; however, immune-mediated disorders occurred in PD-1 and PD-L1 knockout mice. Based on its mechanism of action, fetal exposure to avelumab may increase the risk of developing immune-related disorders or altering the normal immune response.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Avelumab in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Avelumab during labor and delivery.
Nursing Mothers
- There is no information regarding the presence of avelumab in human milk, the effects on the breastfed infant, or the effects on milk production. Since many drugs including antibodies are excreted in human milk, advise a lactating woman not to breastfeed during treatment and for at least one month after the last dose of avelumab due to the potential for serious adverse reactions in breastfed infants.
Pediatric Use
- The safety and effectiveness of avelumab have been established in pediatric patients aged 12 years and older for metastatic MCC. Use of avelumab in this age group is supported by evidence from adequate and well-controlled studies of avelumab in adults with additional population pharmacokinetic data demonstrating that age and body weight had no clinically meaningful effect on the steady state exposure of avelumab, that drug exposure is generally similar between adults and pediatric patients age 12 years and older for monoclonal antibodies, and that the course of MCC is sufficiently similar in adult and pediatric patients to allow extrapolation of data in adults to pediatric patients. The recommended dose in pediatric patients 12 years of age or greater is the same as that in adults.
- Safety and effectiveness of avelumab have not been established in pediatric patients less than 12 years of age.
Geriatic Use
- Metastatic Merkel Cell Carcinoma
- Clinical studies of avelumab in MCC did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients.
- Locally Advanced or Metastatic Urothelial Carcinoma
- Of the 226 patients with locally advanced or metastatic UC treated with avelumab, 68% were 65 years or over and 29% were 75 years or over. Among patients 65 years or over who were followed for at least 13 weeks, 14% (22/153) responded to avelumab and 58% (89/153) developed a Grade 3-4 adverse reaction. No overall differences in safety or efficacy were reported between elderly patients and younger patients.
Gender
There is no FDA guidance on the use of Avelumab with respect to specific gender populations.
Race
There is no FDA guidance on the use of Avelumab with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Avelumab in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Avelumab in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Avelumab in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Avelumab in patients who are immunocompromised.
Administration and Monitoring
Administration
- Administer the diluted solution over 60 minutes through an intravenous line containing a sterile, non-pyrogenic, low protein binding in-line filter (pore size of 0.2 micron).
- Do not co-administer other drugs through the same intravenous line.
Monitoring
- Evidence of disease response or stabilization may indicate efficacy.
- Hyperglycemia or other signs or symptoms of diabetes.
- Liver function tests: Prior to initiation and periodically during therapy.
- Serum creatinine: Prior to initiation and periodically during treatment.
- Thyroid function changes: At initiation and periodically during treatment, and as clinically indicated.
- Signs and symptoms of adrenal insufficiency.
- Signs and symptoms of colitis.
- Signs and symptoms of infusion-related reactions, including pyrexia, chills, flushing, hypotension, dyspnea, wheezing, back pain, abdominal pain, and urticaria.
- Signs and symptoms of pneumonitis: If suspected evaluate with radiographic imaging.
IV Compatibility
There is limited information regarding the compatibility of Avelumab and IV administrations.
Overdosage
There is limited information regarding Avelumab overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
Avelumab?
| |
| Therapeutic monoclonal antibody | |
| Source | u |
| Target | PD-L1 |
| Identifiers | |
| CAS number | |
| ATC code | None |
| PubChem | ? |
| DrugBank | |
| Chemical data | |
| Formula | ? |
| Mol. mass | ? |
| Synonyms | MSB0010718C |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | Proteolysis |
| Half life | 6.1 days |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | Intravenous infusion |
Mechanism of Action
- PD-L1 may be expressed on tumor cells and tumor-infiltrating immune cells and can contribute to the inhibition of the anti-tumor immune response in the tumor microenvironment. Binding of PD-L1 to the PD-1 and B7.1 receptors found on T cells and antigen presenting cells suppresses cytotoxic T-cell activity, T-cell proliferation, and cytokine production. Avelumab binds PD-L1 and blocks the interaction between PD-L1 and its receptors PD-1 and B7.1. This interaction releases the inhibitory effects of PD-L1 on the immune response resulting in the restoration of immune responses, including anti-tumor immune responses. Avelumab has also been shown to induce antibody-dependent cell-mediated cytotoxicity (ADCC) in vitro. In syngeneic mouse tumor models, blocking PD-L1 activity resulted in decreased tumor growth.
Structure
There is limited information regarding Avelumab Structure in the drug label.
Pharmacodynamics
There is limited information regarding Avelumab Pharmacodynamics in the drug label.
Pharmacokinetics
- The pharmacokinetics of avelumab was studied in 1629 patients who received doses ranging from 1 to 20 mg/kg every 2 weeks. The data showed that the exposure of avelumab increased dose-proportionally in the dose range of 10 to 20 mg/kg every 2 weeks. Steady-state concentrations of avelumab were reached after approximately 4 to 6 weeks (2 to 3 cycles) of repeated dosing, and the systemic accumulation was approximately 1.25-fold.
Distribution
- The geometric mean volume of distribution at steady state for a subject receiving 10 mg/kg was 4.72 L.
Elimination
- The primary elimination mechanism of avelumab is proteolytic degradation. Based on population pharmacokinetic analyses in patients with solid tumors, the total systemic clearance was 0.59 L/day and the terminal half-life was 6.1 days in patients receiving 10 mg/kg. In a post hoc analysis, avelumab clearance was found to decrease over time in patients with MCC, with a mean maximal reduction (% coefficient of variation [CV%]) from baseline value of approximately 41.7% (40.0%), which is not considered clinically important. There was no evidence to suggest a change of avelumab clearance over time in patients with UC.
Specific Populations
- Body weight was positively correlated with total systemic clearance in population pharmacokinetic analyses. No clinically meaningful differences in pharmacokinetics were observed in the clearance of avelumab based on age; sex; race; PD-L1 status; tumor burden; mild [calculated creatinine clearance (CLcr) 60 to 89 mL/min, n=623 as estimated by the Cockcroft-Gault formula], moderate [CLcr 30 to 59 mL/min, n=320], or severe [CLcr 15 to 29 mL/min, n=4] renal impairment; and mild [bilirubin less than or equal to ULN and AST greater than ULN or bilirubin between 1 and 1.5 times ULN, n=217] or moderate [bilirubin between 1.5 and 3 times ULN, n=4] hepatic impairment. There are limited data from patients with severe hepatic impairment [bilirubin greater than 3 times ULN, n=1], and the effect of severe hepatic impairment on the pharmacokinetics of avelumab is unknown.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- No studies have been conducted to assess the potential of avelumab for genotoxicity or carcinogenicity.
- Fertility studies have not been conducted with avelumab; however, an assessment of male and female reproductive organs was included in 3-month repeat-dose toxicity study in Cynomolgus monkeys. Weekly administration of avelumab did not result in any notable effects in the male and female reproductive organs.
Animal Toxicology and/or Pharmacology
- In animal models, inhibition of PD-L1/PD-1 signaling increased the severity of some infections and enhanced inflammatory responses. M. tuberculosis-infected PD-1 knockout mice exhibit markedly decreased survival compared with wild-type controls, which correlated with increased bacterial proliferation and inflammatory responses in these animals. PD-L1 and PD-1 knockout mice and mice receiving PD-L1 blocking antibody have also shown decreased survival following infection with lymphocytic choriomeningitis virus.
Clinical Studies
Metastatic Merkel Cell Carcinoma
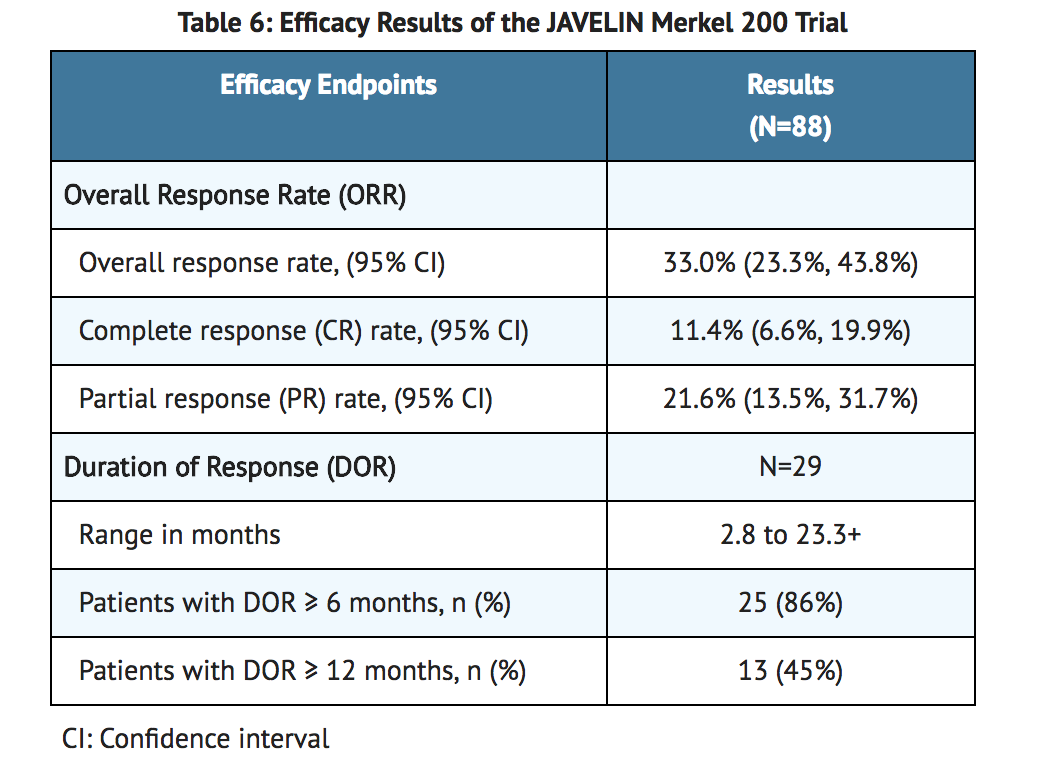
- The efficacy and safety of avelumab was demonstrated in the JAVELIN Merkel 200 trial (NCT02155647), an open-label, single-arm, multi-center study conducted in patients with histologically confirmed metastatic MCC whose disease had progressed on or after chemotherapy administered for distant metastatic disease. The trial excluded patients with autoimmune disease; medical conditions requiring systemic immunosuppression; prior organ or allogeneic stem cell transplantation; prior treatment with anti-PD-1, anti-PD-L1, or anti-CTLA-4 antibodies; CNS metastases; infection with HIV, hepatitis B, or hepatitis C; or ECOG performance score ≥ 2.
- Patients received avelumab 10 mg/kg as an intravenous infusion over 60 minutes every 2 weeks until disease progression or unacceptable toxicity. Patients with radiological disease progression not associated with significant clinical deterioration, defined as no new or worsening symptoms, no change in performance status for greater than 2 weeks, and no need for salvage therapy, could continue treatment. Tumor response assessments were performed every 6 weeks. The major efficacy outcome measures were confirmed overall response rate (ORR) according to Response Evaluation Criteria in Solid Tumors (RECIST) v1.1 as assessed by a blinded independent central review committee (IRC) and IRC-assessed duration of response. The efficacy analysis was conducted when the last patient enrolled had completed 12 months of follow-up.
- A total of 88 patients were enrolled. Baseline patient characteristics were a median age of 73 years (range: 33 to 88), 74% of patients were male, 92% were White, and the ECOG performance score was 0 (56%) or 1 (44%). Seventy-five percent of patients were 65 years or older, 35% were 75 or older, and 3% were 85 or older. Sixty-five percent of patients were reported to have had one prior anti-cancer therapy for metastatic MCC and 35% had two or more prior therapies. Fifty-three percent of patients had visceral metastases. All patients had tumor samples evaluated for PD-L1 expression; of these, 66% were PD-L1-positive (≥ 1% of tumor cells), 18% were PD-L1 negative, and 16% had non-evaluable results by an investigational immunohistochemistry assay. Archival tumor samples were evaluated for Merkel cell polyomavirus (MCV) using an investigational assay; of the 77 patients with evaluable results, 52% had evidence of MCV.
- Efficacy results are presented in Table 6. Responses were observed in patients regardless of tumor PD-L1 expression or presence of MCV.
Locally Advanced or Metastatic Urothelial Carcinoma
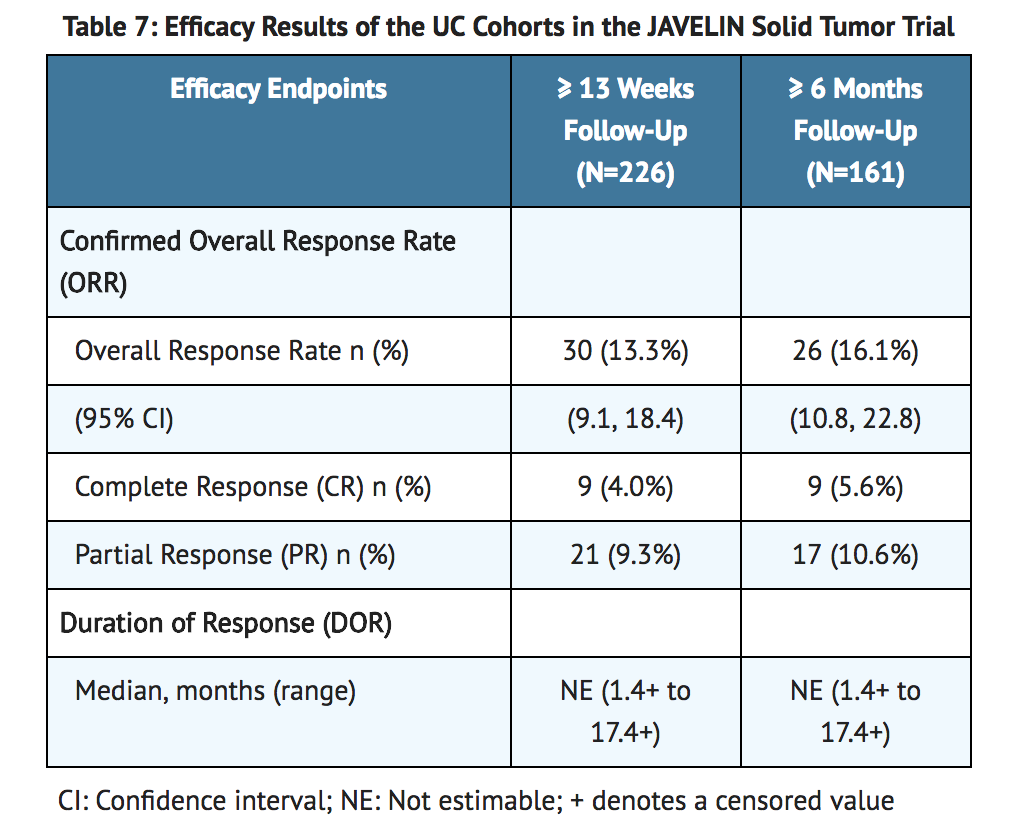
- The efficacy and safety of avelumab was demonstrated in the UC cohorts of the JAVELIN Solid Tumor trial, an open-label, single-arm, multi-center study that included 242 patients with locally advanced or metastatic urothelial carcinoma (UC) with disease progression on or after platinum-containing chemotherapy or who had disease progression within 12 months of treatment with a platinum-containing neoadjuvant or adjuvant chemotherapy regimen. Patients with active or history of central nervous system metastasis; other malignancies within the last 5 years; organ transplant; conditions requiring therapeutic immune suppression; or active infection with HIV, hepatitis B, or hepatitis C were excluded. Patients with autoimmune disease, other than type 1 diabetes, vitiligo, psoriasis, or thyroid disease that did not require immunosuppressive treatment, were excluded. Patients were included regardless of their PD-L1 status.
- Patients received avelumab at a dose of 10 mg/kg intravenously every 2 weeks until radiographic or clinical progression or unacceptable toxicity. Tumor response assessments were performed every 6 weeks. Efficacy outcome measures included confirmed overall response rate (ORR), as assessed by an Independent Endpoint Review Committee (IERC) using Response Evaluation Criteria in Solid Tumors (RECIST) v1.1, and duration of response (DOR). Efficacy was evaluated in patients who were followed for a minimum of both 13 weeks and 6 months at the time of data cut-off.
- Baseline demographic and disease characteristics for the 226 patients with a minimum of 13 weeks of follow-up were median age 68 years (range: 30 to 89), 72% male, 80% White, and 34% and 66% of patients had an ECOG performance status 0 and 1, respectively. Forty-four percent of patients had non-bladder urothelial carcinoma including 23% of patients with upper tract disease, and 83% of patients had visceral metastases (baseline target and/or non-target lesions present outside of the lymph nodes). Nine (4%) patients had disease progression following prior platinum-containing neoadjuvant or adjuvant therapy only. Forty-seven percent of patients only received prior cisplatin-based regimens, 32% received only prior carboplatin-based regimens, and 20% received both cisplatin and carboplatin-based regimens. At baseline, 17% of patients had a hemoglobin < 10 g/dL and 34% of patients had liver metastases.
- Efficacy results are presented in Table 7. The median time to response was 2.0 months (range: 1.3 to 11.0) among patients followed for either ≥ 13 weeks or ≥ 6 months. Using a clinical trial assay to assess PD-L1 staining, with 16% of patients not evaluable, there were no clear differences in response rates based on PD-L1 tumor expression. Among the total 30 responding patients followed for ≥ 13 weeks, 22 patients (73%) had an ongoing response of 6 months or longer and 4 patients (13%) had ongoing responses of 12 months or longer. Among the total 26 responding patients followed for ≥ 6 months, 22 patients (85%) had ongoing responses of 6 months or longer and 4 patients (15%) had ongoing responses of 12 months or longer.
How Supplied
- Avelumab Injection is a sterile, preservative-free, and clear, colorless to slightly yellow solution for intravenous infusion supplied as a single-dose vial of 200 mg/10 mL (20 mg/mL), individually packed into a carton (NDC 44087-3535-1).
Storage
- Store refrigerated at 36°F to 46°F (2°C to 8°C) in original package to protect from light.
- Do not freeze or shake the vial.
- The vial stopper is not made with natural rubber latex.
Images
Drug Images
{{#ask: Page Name::Avelumab |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Avelumab |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Immune-Mediated Adverse Reactions
Inform patients of the risk of immune-mediated adverse reactions requiring corticosteroids or hormone replacement therapy, including, but not limited to:
- Pneumonitis: Advise patients to contact their healthcare provider immediately for new or worsening cough, chest pain, or shortness of breath.
- Hepatitis: Advise patients to contact their healthcare provider immediately for jaundice, severe nausea or vomiting, pain on the right side of abdomen, lethargy, or easy bruising or bleeding.
- Colitis: Advise patients to contact their healthcare provider immediately for diarrhea or severe abdominal pain.
- Endocrinopathies: Advise patients to contact their healthcare provider immediately for signs or symptoms of adrenal insufficiency, hypothyroidism, hyperthyroidism, and diabetes mellitus.
- Nephritis and Renal Dysfunction: Advise patients to contact their healthcare provider immediately for signs or symptoms of nephritis including decreased urine output, blood in urine, swelling in ankles, loss of appetite, and any other symptoms of renal dysfunction.
Infusion-Related Reactions
- Advise patients to contact their healthcare provider immediately for signs or symptoms of potential infusion-related reactions.
Embryo-Fetal Toxicity
- Advise females of reproductive potential that avelumab can cause fetal harm. Instruct females of reproductive potential to use highly effective contraception during and for at least one month after the last dose of avelumab.
Lactation
- Advise nursing mothers not to breastfeed while taking avelumab and for at least one month after the final dose.
Precautions with Alcohol
Alcohol-Avelumab interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Bavencio
Look-Alike Drug Names
There is limited information regarding Avelumab Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.