Artemether and lumefantrin: Difference between revisions
No edit summary |
No edit summary |
||
| Line 95: | Line 95: | ||
====Prior Use of Mefloquine==== | ====Prior Use of Mefloquine==== | ||
Administration of three doses of mefloquine followed 12 hours later by a 6-dose regimen of Coartem Tablets in 14 healthy volunteers demonstrated no effect of mefloquine on plasma concentrations of artemether or the artemether/DHA ratio. However, exposure to lumefantrine was reduced, possibly due to lower absorption secondary to a mefloquine-induced decrease in bile production. Patients should be monitored for decreased efficacy and food consumption should be encouraged with administration of Coartem Tablets | Administration of three doses of [[mefloquine]] followed 12 hours later by a 6-dose regimen of Coartem Tablets in 14 healthy volunteers demonstrated no effect of [[mefloquine]] on plasma concentrations of artemether or the artemether/DHA ratio. However, exposure to [[lumefantrine]] was reduced, possibly due to lower absorption secondary to a [[mefloquine]]-induced decrease in bile production. Patients should be monitored for decreased efficacy and food consumption should be encouraged with administration of Coartem Tablets. | ||
====Hormonal Contraceptives==== | ====Hormonal Contraceptives==== | ||
In vitro, the metabolism of ethinyl estradiol and levonorgestrel was not induced by artemether, DHA, or lumefantrine. However, artemether has been reported to weakly induce, in humans, the activity of CYP2C19, CYP2B6, and CYP3A. Therefore, Coartem Tablets may potentially reduce the effectiveness of hormonal contraceptives. Patients using oral, transdermal patch, or other systemic hormonal contraceptives should be advised to use an additional non-hormonal method of birth control | In vitro, the metabolism of [[ethinyl estradiol]] and [[levonorgestrel]] was not induced by artemether, DHA, or [[lumefantrine]]. However, artemether has been reported to weakly induce, in humans, the activity of [[CYP2C19]], [[CYP2B6]], and [[CYP3A]]. Therefore, Coartem Tablets may potentially reduce the effectiveness of [[hormonal contraceptives]]. Patients using oral, transdermal patch, or other systemic hormonal contraceptives should be advised to use an additional non-hormonal method of birth control. | ||
====CYP2D6 Substrates==== | ====CYP2D6 Substrates==== | ||
Lumefantrine inhibits CYP2D6 in vitro. Administration of Coartem Tablets with drugs that are metabolized by CYP2D6 may significantly increase plasma concentrations of the co-administered drug and increase the risk of adverse effects. Many of the drugs metabolized by CYP2D6 can prolong the QT interval and should not be administered with Coartem Tablets due to the potential additive effect on the QT interval (e.g., flecainide, imipramine, amitriptyline, clomipramine) | Lumefantrine inhibits [[CYP2D6]] in vitro. Administration of Coartem Tablets with drugs that are metabolized by [[CYP2D6]] may significantly increase plasma concentrations of the co-administered drug and increase the risk of adverse effects. Many of the drugs metabolized by [[CYP2D6]] can prolong the [[QT interval]+ and should not be administered with Coartem Tablets due to the potential additive effect on the [[QT interval]] (e.g., [[flecainide]], [[imipramine]], [[amitriptyline]], [[clomipramine]]) | ||
====Sequential Use of Quinine==== | ====Sequential Use of Quinine==== | ||
A single dose of intravenous quinine (10 mg/kg bodyweight) concurrent with the final dose of a 6-dose regimen of Coartem Tablets demonstrated no effect of intravenous quinine on the systemic exposure of DHA or lumefantrine. Quinine exposure was also not altered. Exposure to artemether was decreased. This decrease in artemether exposure is not thought to be clinically significant. However, quinine and other drugs that prolong the QT interval should be used cautiously following treatment with Coartem Tablets due to the long elimination half-life of lumefantrine and the potential for additive QT effects; ECG monitoring is advised if use of drugs that prolong the QT interval is medically required | A single dose of intravenous [[quinine]] (10 mg/kg bodyweight) concurrent with the final dose of a 6-dose regimen of Coartem Tablets demonstrated no effect of intravenous [[quinine]] on the systemic exposure of DHA or [[lumefantrine]]. [[Quinine]] exposure was also not altered. Exposure to artemether was decreased. This decrease in artemether exposure is not thought to be clinically significant. However, [[quinine]] and other drugs that prolong the [[QT interval]] should be used cautiously following treatment with Coartem Tablets due to the long elimination half-life of [[lumefantrine]] and the potential for additive [[QT effects]]; ECG monitoring is advised if use of drugs that prolong the [[QT interval]] is medically required. | ||
====Interaction with Drugs that are Known to Prolong the QT Interval==== | ====Interaction with Drugs that are Known to Prolong the QT Interval==== | ||
Coartem is to be used with caution when co-administered with drugs that may cause prolonged QT interval such as antiarrhythmics of classes IA and III, neuroleptics and antidepressant agents, certain antibiotics including some agents of the following classes: macrolides, fluoroquinolones, imidazole, and triazole antifungal agents | Coartem is to be used with caution when co-administered with drugs that may cause prolonged [[QT interval]] such as [[antiarrhythmics]] of classes IA and III, [[neuroleptics]] and [[antidepressant agents]], certain [[antibiotics]] including some agents of the following classes: [[macrolides]], [[fluoroquinolones]], [[imidazole]], and [[triazole]] [[antifungal agents]]. | ||
|alcohol=Alcohol-Artemether and lumefantrin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |alcohol=Alcohol-Artemether and lumefantrin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | ||
}} | }} | ||
Revision as of 20:58, 4 February 2015
{{DrugProjectFormSinglePage |authorTag=Alberto Plate [1] |genericName=Artemether |aOrAn=an |drugClass=antimanlaric |indicationType=treatment |indication=acute, uncomplicated malaria infections due to Plasmodium falciparum in patients of 5 kg bodyweight and above |adverseReactions=headache, anorexia, dizziness, asthenia, arthralgia and myalgia |blackBoxWarningTitle=TITLE |blackBoxWarningBody=Condition Name: (Content) |offLabelAdultGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Artemether and lumefantrin in adult patients. |offLabelAdultNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Artemether and lumefantrin in adult patients. |offLabelPedGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Artemether and lumefantrin in pediatric patients. |offLabelPedNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Artemether and lumefantrin in pediatric patients. |contraindications=====Hypersensitivity====
- Known hypersensitivity to artemether, lumefantrine, or to any of the excipients of Coartem Tablets.
Strong CYP3A4 Inducers
- Co-administration of strong inducers of CYP3A4 such as rifampin, carbamazepine, phenytoin and St. John's wort with Coartem Tablets can result in decreased concentrations of artemether and/or lumefantrine and loss of antimalarial efficacy.
|warnings=====Prolongation of the QT Interval==== Some antimalarials (e.g., halofantrine, quinine, quinidine) including Coartem Tablets have been associated with prolongation of the QT interval on the electrocardiogram. Coartem Tablets should be avoided in patients:
- With congenital prolongation of the QT interval (e.g., long QT syndrome) or any other clinical condition known to prolong the QTc interval such as patients with a history of symptomatic cardiac arrhythmias, with clinically relevant bradycardia or with severe cardiac disease.
- With a family history of congenital prolongation of the QT interval or sudden death.
- With known disturbances of electrolyte balance, e.g., hypokalemia or hypomagnesemia.
- Receiving other medications that prolong the QT interval, such as class IA (quinidine, procainamide, disopyramide), or class III (amiodarone, sotalol) antiarrhythmic agents; antipsychotics (pimozide, ziprasidone); antidepressants; certain antibiotics (macrolide antibiotics, fluoroquinolone antibiotics, imidazole, and triazole antifungal agents).
- Receiving medications that are metabolized by the cytochrome enzyme CYP2D6 which also have cardiac effects (e.g., flecainide, imipramine, amitriptyline, clomipramine).
Use of QT Prolonging Drugs and Other Antimalarials
- Halofantrine and Coartem Tablets should not be administered within one month of each other due to the long elimination half-life of lumefantrine (3-6 days) and potential additive effects on the QT interval.
- Antimalarials should not be given concomitantly with Coartem Tablets, unless there is no other treatment option, due to limited safety data.
- Drugs that prolong the QT interval, including antimalarials such as quinine and quinidine, should be used cautiously following Coartem Tablets, due to the long elimination half-life of lumefantrine (3-6 days) and the potential for additive effects on the QT interval; ECG monitoring is advised if use of drugs that prolong the QT interval is medically required.
- If mefloquine is administered immediately prior to Coartem Tablets there may be a decreased exposure to lumefantrine, possibly due to a mefloquine-induced decrease in bile production. Therefore, patients should be monitored for decreased efficacy and food consumption should be encouraged while taking Coartem Tablets.
Drug Interactions with CYP3A4
- When Coartem Tablets are co-administered with substrates of CYP3A4 it may result in decreased concentrations of the substrate and potential loss of substrate efficacy. When Coartem Tablets are co-administered with an inhibitor of CYP3A4, including grapefruit juice it may result in increased concentrations of artemether and/or lumefantrine and potentiate QT prolongation. When Coartem Tablets are co-administered with inducers of CYP3A4 it may result in decreased concentrations of artemether and/or lumefantrine and loss of antimalarial efficacy.
- Drugs that have a mixed effect on CYP3A4, especially antiretroviral drugs such as HIV protease inhibitors and non-nucleoside reverse transcriptase inhibitors, and those that have an effect on the QT interval should be used with caution in patients taking Coartem Tablets.
- Coartem Tablets may reduce the effectiveness of hormonal contraceptives. Therefore, patients using oral, transdermal patch, or other systemic hormonal contraceptives should be advised to use an additional non-hormonal method of birth control.
Drug Interactions with CYP2D6
- Administration of Coartem Tablets with drugs that are metabolized by CYP2D6 may significantly increase plasma concentrations of the co-administered drug and increase the risk of adverse effects. Many of the drugs metabolized by CYP2D6 can prolong the QT interval and should not be administered with Coartem Tablets due to the potential additive effect on the QT interval (e.g., flecainide, imipramine, amitriptyline, clomipramine).
Recrudescence
- Food enhances absorption of artemether and lumefantrine following administration of Coartem Tablets.
- Patients who remain averse to food during treatment should be closely monitored as the risk of recrudescence may be greater. In the event of recrudescent P. falciparum infection after treatment with Coartem Tablets, patients should be treated with a different antimalarial drug.
Hepatic and Renal Impairment
- Coartem Tablets have not been studied for efficacy and safety in patients with severe hepatic and/or renal impairment.
Plasmodium vivax Infection
- Coartem Tablets have been shown in limited data (43 patients) to be effective in treating the erythrocytic stage of P. vivax infection. However, relapsing malaria caused by P. vivax requires additional treatment with other antimalarial agents to achieve radical cure i.e., eradicate any hypnozoites forms that may remain dormant in the liver.
|clinicalTrials=====Serious Adverse Reactions==== The following serious and otherwise important adverse reactions are discussed in greater detail in other sections of labeling:
Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rate observed in practice.
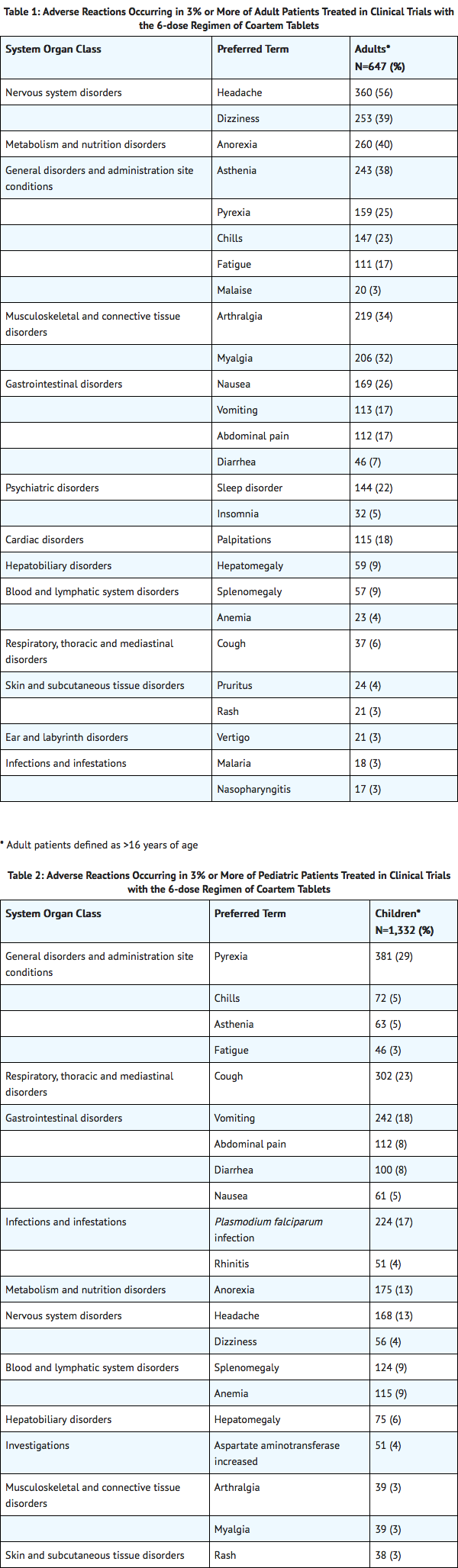
The data described below reflect exposure to a 6-dose regimen of Coartem Tablets in 1,979 patients including 647 adults (older than 16 years) and 1,332 children (16 years and younger). For the 6-dose regimen, Coartem Tablets was studied in active-controlled (366 patients) and non-controlled, open-label trials (1,613 patients). The 6-dose Coartem Tablets population was patients with malaria between ages 2 months and 71 years: 67% (1,332) were 16 years and younger and 33% (647) were older than 16 years. Males represented 73% and 53% of the adult and pediatric populations, respectively. The majority of adult patients were enrolled in studies in Thailand, while the majority of pediatric patients were enrolled in Africa.
Tables 1 and 2 show the most frequently reported adverse reactions (вЙ•3%) in adults and children respectively who received the 6-dose regimen of Coartem Tablets. Adverse reactions collected in clinical trials included signs and symptoms at baseline but only treatment emergent adverse events, defined as events that appeared or worsened after the start of treatment, are presented below. In adults, the most frequently reported adverse reactions were headache, anorexia, dizziness, and asthenia. In children, the adverse reactions were pyrexia, cough, vomiting, anorexia, and headache. Most adverse reactions were mild, did not lead to discontinuation of study medication, and resolved.
In limited comparative studies, the adverse reaction profile of Coartem Tablets appeared similar to that of another antimalarial regimen.
Discontinuation of Coartem Tablets due to adverse drug reactions occurred in 1.1% of patients treated with the 6-dose regimen overall: 0.2% (1/647) in adults and 1.6% (21/1,332) in children.
Clinically significant adverse reactions reported in adults and/or children treated with the 6-dose regimen of Coartem Tablets which occurred in clinical studies at <3% regardless of causality are listed below:
- Blood and lymphatic system disorders: eosinophilia
- Ear and labyrinth disorders: tinnitus
- Eye disorders: conjunctivitis
- Gastrointestinal disorders: constipation, dyspepsia, dysphagia, peptic ulcer
- General disorders: gait disturbance
- Infections and infestations: abscess, acrodermatitis, bronchitis, ear infection, gastroenteritis, helminthic infection, hookworm infection, impetigo, influenza, lower respiratory tract infection, malaria, nasopharyngitis, oral herpes, pneumonia, respiratory tract infection, subcutaneous abscess, upper respiratory tract infection, urinary tract infection
- Investigations: alanine aminotransferase increased, aspartate aminotransferase increased, hematocrit decreased, lymphocyte morphology abnormal, platelet count decreased, platelet count increased, white blood cell count decreased, white blood cell count increased
- Metabolism and nutrition disorders: hypokalemia
- Musculoskeletal and connective tissue disorders: back pain
- Nervous system disorders: ataxia, clonus, fine motor delay, hyperreflexia, hypoaesthesia, nystagmus, tremor.
- Psychiatric disorders: agitation, mood swings
- Renal and urinary disorders: hematuria, proteinuria
- Respiratory, thoracic and mediastinal disorders: asthma, pharyngo-laryngeal pain
- Skin and subcutaneous tissue disorders: urticaria
|postmarketing=The following adverse reactions have been identified during post-approval use of Coartem Tablets. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Hypersensitivity reactions including urticaria and angioedema. Serious skin reactions (bullous eruption) have been rarely reported.
|drugInteractions=====Rifampin==== Oral administration of rifampin, a strong CYP3A4 inducer, with Coartem Tablets resulted in significant decreases in exposure to artemether, dihydroartemisinin (DHA, metabolite of artemether) and lumefantrine by 89%, 85% and 68%, respectively, when compared to exposure values after Coartem Tablets alone. Concomitant use of strong inducers of CYP3A4 such as rifampin, carbamazepine, phenytoin and St. John's wort is contraindicated with Coartem Tablets.
Ketoconazole
Concurrent oral administration of ketoconazole, a potent CYP3A4 inhibitor, with a single dose of Coartem Tablets resulted in a moderate increase in exposure to artemether, DHA, and lumefantrine in a study of 15 healthy subjects. No dose adjustment of Coartem Tablets is necessary when administered with ketoconazole or other potent CYP3A4 inhibitors. However, due to the potential for increased concentrations of lumefantrine which could lead to QT prolongation, Coartem Tablets should be used cautiously with drugs that inhibit CYP3A4.
Antiretroviral Drugs
Both artemether and lumefantrine are metabolized by CYP3A4. Antiretroviral drugs, such as protease inhibitors and non-nucleoside reverse transcriptase inhibitors, are known to have variable patterns of inhibition, induction or competition for CYP3A4. Therefore, the effects of antiretroviral drugs on the exposure to artemether, DHA, and lumefantrine are also variable [see Clinical Pharmacology (12.3)]. Coartem Tablets should be used cautiously in patients on antiretroviral drugs because decreased artemether, DHA, and/or lumefantrine concentrations may result in a decrease of antimalarial efficacy of Coartem Tablets, and increased lumefantrine concentrations may cause QT prolongation.
Prior Use of Mefloquine
Administration of three doses of mefloquine followed 12 hours later by a 6-dose regimen of Coartem Tablets in 14 healthy volunteers demonstrated no effect of mefloquine on plasma concentrations of artemether or the artemether/DHA ratio. However, exposure to lumefantrine was reduced, possibly due to lower absorption secondary to a mefloquine-induced decrease in bile production. Patients should be monitored for decreased efficacy and food consumption should be encouraged with administration of Coartem Tablets.
Hormonal Contraceptives
In vitro, the metabolism of ethinyl estradiol and levonorgestrel was not induced by artemether, DHA, or lumefantrine. However, artemether has been reported to weakly induce, in humans, the activity of CYP2C19, CYP2B6, and CYP3A. Therefore, Coartem Tablets may potentially reduce the effectiveness of hormonal contraceptives. Patients using oral, transdermal patch, or other systemic hormonal contraceptives should be advised to use an additional non-hormonal method of birth control.
CYP2D6 Substrates
Lumefantrine inhibits CYP2D6 in vitro. Administration of Coartem Tablets with drugs that are metabolized by CYP2D6 may significantly increase plasma concentrations of the co-administered drug and increase the risk of adverse effects. Many of the drugs metabolized by CYP2D6 can prolong the [[QT interval]+ and should not be administered with Coartem Tablets due to the potential additive effect on the QT interval (e.g., flecainide, imipramine, amitriptyline, clomipramine)
Sequential Use of Quinine
A single dose of intravenous quinine (10 mg/kg bodyweight) concurrent with the final dose of a 6-dose regimen of Coartem Tablets demonstrated no effect of intravenous quinine on the systemic exposure of DHA or lumefantrine. Quinine exposure was also not altered. Exposure to artemether was decreased. This decrease in artemether exposure is not thought to be clinically significant. However, quinine and other drugs that prolong the QT interval should be used cautiously following treatment with Coartem Tablets due to the long elimination half-life of lumefantrine and the potential for additive QT effects; ECG monitoring is advised if use of drugs that prolong the QT interval is medically required.
Interaction with Drugs that are Known to Prolong the QT Interval
Coartem is to be used with caution when co-administered with drugs that may cause prolonged QT interval such as antiarrhythmics of classes IA and III, neuroleptics and antidepressant agents, certain antibiotics including some agents of the following classes: macrolides, fluoroquinolones, imidazole, and triazole antifungal agents. |alcohol=Alcohol-Artemether and lumefantrin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. }}