Aortic dissection classification
|
Aortic dissection Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenarios |
|
Case Studies |
|
|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Several different classification systems have been used to describe aortic dissections. The systems commonly in use are either based on either the anatomy of the dissection (proximal, distal) or the duration of onset of symptoms (acute, chronic) prior to presentation.
Classification
- Several classification systems have been suggested for the description of aortic dissection.[1][2][3][4]
- The commonly used classifications for aortic dissection are either based on the timing of the symptoms or the anatomy of the dissection.
- DeBakey and Stanford systems are the commonly used classification systems for aortic dissection.
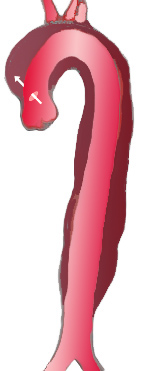
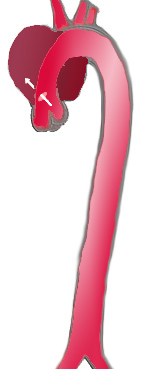
DeBakey Classification System
The DeBakey system classifies aortic dissection based on anatomy of the aorta. It classifies the dissection according to the intimal tear location.[5]
- Type I - Intimal tear is located in ascending aorta, spreads at least to the aortic arch and often beyond it distally.
- Type II –Intimal tear is located and limited to the ascending aorta.
- Type III – Intimal tear is located in descending aorta, rarely extends proximally.
- Type III A: Dissection limited to the descending thoracic aorta
- Type III B: Dissection extended below the diaphragm
|
|

| |
| Percentage | 60 % | 10-15 % | 25-30 % |
| Type | DeBakey I | DeBakey II | DeBakey III |
| Stanford A | Stanford B | ||
| Proximal | Distal | ||
| Classification of aortic dissection | |||
Stanford Classification System
Stanford classification system is based on the involvement of ascending aorta.[6]
- A = Type I and II DeBakey
- B = Type III Debakey

Classification based on the Proximity
- Proximal: Ascending aortic involvement
- Distal: Descending aortic involvement distal to left subclavian artery
Classification by the Time of Onset
- Acute: Onset within 2 weeks of onset of pain
- Subacute: Onset within 2-6 weeks of onset of pain
- Chronic: Onset within 6 weeks of pain.
References
- ↑ Nienaber CA, Eagle KA (August 2003). "Aortic dissection: new frontiers in diagnosis and management: Part I: from etiology to diagnostic strategies". Circulation. 108 (5): 628–35. doi:10.1161/01.CIR.0000087009.16755.E4. PMID 12900496.
- ↑ Tsai TT, Nienaber CA, Eagle KA (December 2005). "Acute aortic syndromes". Circulation. 112 (24): 3802–13. doi:10.1161/CIRCULATIONAHA.105.534198. PMID 16344407.
- ↑ DEBAKEY ME, HENLY WS, COOLEY DA, MORRIS GC, CRAWFORD ES, BEALL AC (January 1965). "SURGICAL MANAGEMENT OF DISSECTING ANEURYSMS OF THE AORTA". J. Thorac. Cardiovasc. Surg. 49: 130–49. PMID 14261867.
- ↑ Daily PO, Trueblood HW, Stinson EB, Wuerflein RD, Shumway NE (September 1970). "Management of acute aortic dissections". Ann. Thorac. Surg. 10 (3): 237–47. doi:10.1016/s0003-4975(10)65594-4. PMID 5458238.
- ↑ DeBakey ME, Henly WS, Cooley DA, Morris GC Jr, Crawford ES, Beall AC Jr. Surgical management of dissecting aneurysms of the aorta. J Thorac Cardiovasc Surg 1965;49:130-49. PMID 14261867.
- ↑ Daily PO, Trueblood HW, Stinson EB, Wuerflein RD, Shumway NE. Management of acute aortic dissections. Ann Thorac Surg 1970;10:237-47. PMID 5458238.