Aortic dissection chest x ray: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| (24 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | {{Aortic dissection}} | ||
{{CMG}} ; '''Associate Editor-In-Chief:''' {{CZ}}; {{RT}} | {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}}; {{RT}} {{Sahar}} | ||
==Overview== | ==Overview== | ||
[[Chest x-ray]] may be helpful in the [[diagnosis]] of aortic dissection. Findings suggestive of aortic dissection on [[x-ray]] include widening of mediastinum, wide [[aortic]] contour, tracheal deviation, aortic kinking, and displacement of previous aortic calcification. [[Chest x-ray]] has limited [[sensitivity]] (64%) and [[specificity]] (86%) in the [[diagnosis]] of [[Aortic disease|aortic diseases]]. It also worth mentioning that a normal [[Chest X-ray|chest x-ray]] may not rule out the [[diagnosis]] of aortic dissection. | |||
==Chest X Ray== | ==Chest X Ray== | ||
*Findings on [[chest x-ray]] suggestive of aortic dissection include:<ref name="pmid14715319">{{cite journal |vauthors=von Kodolitsch Y, Nienaber CA, Dieckmann C, Schwartz AG, Hofmann T, Brekenfeld C, Nicolas V, Berger J, Meinertz T |title=Chest radiography for the diagnosis of acute aortic syndrome |journal=Am. J. Med. |volume=116 |issue=2 |pages=73–7 |date=January 2004 |pmid=14715319 |doi=10.1016/j.amjmed.2003.08.030 |url=}}</ref> | |||
* [[Wide mediastinum|Widening of mediastinum]] | **[[Wide mediastinum|Widening of mediastinum]] | ||
* Tracheal deviation | ** Wide [[aortic]] contour | ||
* The calcium sign - separation of the | **[[Tracheal deviation]] | ||
* [[Pleural effusion]]s may be noted | ** Aortic kinking | ||
** The [[calcium]] sign - separation of the [[intima]]l [[calcification]] from the outer [[aortic]] soft [[tissue]] border by 10 mm <ref name="GartlandSookur2007">{{cite journal|last1=Gartland|first1=S|last2=Sookur|first2=D|last3=Lee|first3=H|title=Aortic dissection: an x ray sign|journal=Emergency Medicine Journal|volume=24|issue=4|year=2007|pages=310–310|issn=1472-0205|doi=10.1136/emj.2006.037010}}</ref> | |||
**[[Pleural effusion]]s may be noted | |||
* | *According to one study, the following features were more likely to be observed on [[chest x-ray]]: | ||
* | ** Aortic kinking or tortuosity | ||
* | ** Displacement of previous [[calcification]] | ||
** Wide aortic contour | |||
A 'normal' chest x-ray does not rule out the possibility of an aortic dissection. | *A 'normal' [[chest x-ray]] does not rule out the possibility of an [[aortic]] dissection.<ref name="HartnellWakeley1993">{{cite journal|last1=Hartnell|first1=G. G.|last2=Wakeley|first2=C. J.|last3=Tottle|first3=A.|last4=Papouchado|first4=M.|last5=Wilde|first5=R. P. H.|title=Limitations of Chest Radiography in Discriminating Between Aortic Dissection and Myocardial Infarction|journal=Journal of Thoracic Imaging|volume=8|issue=2|year=1993|pages=152–155|issn=0883-5993|doi=10.1097/00005382-199321000-00008}}</ref><br> | ||
*[[Chest x-ray]] [[sensitivity]] for the [[diagnosis]] of [[aortic]] disease is 64%.<ref name="pmid14715319">{{cite journal |vauthors=von Kodolitsch Y, Nienaber CA, Dieckmann C, Schwartz AG, Hofmann T, Brekenfeld C, Nicolas V, Berger J, Meinertz T |title=Chest radiography for the diagnosis of acute aortic syndrome |journal=Am. J. Med. |volume=116 |issue=2 |pages=73–7 |date=January 2004 |pmid=14715319 |doi=10.1016/j.amjmed.2003.08.030 |url=}}</ref> | |||
*[[Chest x-ray]] [[specificity]] for the [[diagnosis]] of [[aortic]] disease is 86%. | |||
*[[Chest X-ray|Chest x-ray]] has particularly low [[accuracy]] in the [[diagnosis]] of ascending aortic dissection. | |||
===Chest X-Ray Examples of Aortic Dissection=== | |||
[[File:Aortic-dissection-23.png|thumb|left|500px|Aortic dissection with marked widening of the mediastinum<ref>Case courtesy of Dr Wayland Wang, Radiopaedia.org, rID: 50763</ref>]] | |||
[[File:Aortic-dissection-34.jpeg|thumb|center|400px|Aortic dissection with marked pleural effusion (blue arrow), left upper mediastinal mass (yellow arrow), and tracheal deviation (orange arrow)<ref>Case courtesy of Dr Devanshi Pathania, Radiopaedia.org, rID: 68763</ref>]] | |||
==2014 ESC Guidelines on the Diagnosis and Treatment of Aortic Diseases (DO NOT EDIT)<ref>{{cite journal|title=2014 ESC Guidelines on the diagnosis and treatment of aortic diseases|journal=European Heart Journal|volume=35|issue=41|year=2014|pages=2873–2926|issn=0195-668X|doi=10.1093/eurheartj/ehu281}}</ref>== | |||
{|class="wikitable" | |||
|- | |||
|colspan="1" style="text-align:center; background:LemonChiffon"| [[ESC guidelines classification scheme#Classification of Recommendations|Class IIb]] | |||
|- | |||
|bgcolor="LemonChiffon"|<nowiki>"</nowiki> Chest X-ray may be considered in cases of low clinical probability of AAS. ''([[ESC guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | |||
|} | |||
==2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the Diagnosis and Management of Patients With Thoracic Aortic Disease(DO NOT EDIT)<ref name="pmid20233780">{{cite journal |author=Hiratzka LF, Bakris GL, Beckman JA, ''et al.'' |title=2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine |journal=[[Circulation]] |volume=121 |issue=13 |pages=e266–369 |year=2010 |month=April |pmid=20233780 |doi=10.1161/CIR.0b013e3181d4739e |url=}}</ref>== | ==2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the Diagnosis and Management of Patients With Thoracic Aortic Disease (DO NOT EDIT)<ref name="pmid20233780">{{cite journal |author=Hiratzka LF, Bakris GL, Beckman JA, ''et al.'' |title=2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine |journal=[[Circulation]] |volume=121 |issue=13 |pages=e266–369 |year=2010 |month=April |pmid=20233780 |doi=10.1161/CIR.0b013e3181d4739e |url=}}</ref>== | ||
===Screening Tests (DO NOT EDIT)<ref name="pmid20233780">{{cite journal |author=Hiratzka LF, Bakris GL, Beckman JA, ''et al.'' |title=2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine |journal=[[Circulation]] |volume=121 |issue=13 |pages=e266–369 |year=2010 |month=April |pmid=20233780 |doi=10.1161/CIR.0b013e3181d4739e |url=}}</ref>=== | ===Screening Tests (DO NOT EDIT)<ref name="pmid20233780">{{cite journal |author=Hiratzka LF, Bakris GL, Beckman JA, ''et al.'' |title=2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine |journal=[[Circulation]] |volume=121 |issue=13 |pages=e266–369 |year=2010 |month=April |pmid=20233780 |doi=10.1161/CIR.0b013e3181d4739e |url=}}</ref>=== | ||
{|class="wikitable" | {|class="wikitable" | ||
| Line 26: | Line 38: | ||
| colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | | colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | ||
|- | |- | ||
|bgcolor="LightGreen" |<nowiki>"</nowiki>'''1.''' The role of [[chest x-ray]] in the evaluation of possible thoracic aortic disease should be directed by the patient's pretest risk of disease as follows: | |bgcolor="LightGreen" |<nowiki>"</nowiki>'''1.''' The role of [[chest x-ray]] in the evaluation of possible [[thoracic aorta|thoracic aortic]] disease should be directed by the patient's pretest risk of disease as follows: | ||
|- | |- | ||
|bgcolor="LightGreen" |'''a.''' Intermediate risk: [[Chest x-ray]] should be performed on all intermediate-risk patients, as it may establish a clear alternate diagnosis that will obviate the need for definitive aortic imaging. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])'' | |bgcolor="LightGreen" |'''a.''' Intermediate risk: [[Chest x-ray]] should be performed on all intermediate-risk patients, as it may establish a clear alternate [[diagnosis]] that will obviate the need for definitive aortic imaging. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])'' | ||
|- | |- | ||
|bgcolor="LightGreen" |'''b.''' Low risk: [[Chest x-ray]] should be performed on all low-risk patients, as it may either establish an alternative diagnosis or demonstrate findings that are suggestive of thoracic aortic disease, indicating the need for urgent definitive aortic imaging. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | |bgcolor="LightGreen" |'''b.''' Low risk: [[Chest x-ray]] should be performed on all low-risk patients, as it may either establish an alternative [[diagnosis]] or demonstrate findings that are suggestive of [[thoracic aorta|thoracic aortic]] disease, indicating the need for urgent definitive [[aortic]] imaging. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | ||
|} | |} | ||
| Line 37: | Line 49: | ||
|colspan="1" style="text-align:center; background:LightCoral"| [[ACC AHA guidelines classification scheme#Classification of Recommendations|Class III]] (No Benefit) | |colspan="1" style="text-align:center; background:LightCoral"| [[ACC AHA guidelines classification scheme#Classification of Recommendations|Class III]] (No Benefit) | ||
|- | |- | ||
|bgcolor="LightCoral"|<nowiki>"</nowiki> '''1.''' A negative [[chest x-ray]] should not delay definitive aortic imaging in patients determined to be high risk for [[aortic dissection]] by initial screening. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | |bgcolor="LightCoral"|<nowiki>"</nowiki> '''1.''' A negative [[chest x-ray]] should not delay definitive [[aortic]] imaging in patients determined to be high risk for [[aortic dissection]] by initial screening. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])''<nowiki>"</nowiki> | ||
|} | |} | ||
== References == | == References == | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[CME Category::Cardiology]] | |||
[[Category:Grammar]] | [[Category:Grammar]] | ||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
| Line 48: | Line 64: | ||
[[Category:Up-To-Date]] | [[Category:Up-To-Date]] | ||
[[Category:Up-To-Date cardiology]] | [[Category:Up-To-Date cardiology]] | ||
[[Category:Best pages]] | |||
Latest revision as of 19:26, 20 December 2019
|
Aortic dissection Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenarios |
|
Case Studies |
|
|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Raviteja Guddeti, M.B.B.S. [3] Sahar Memar Montazerin, M.D.[4]
Overview
Chest x-ray may be helpful in the diagnosis of aortic dissection. Findings suggestive of aortic dissection on x-ray include widening of mediastinum, wide aortic contour, tracheal deviation, aortic kinking, and displacement of previous aortic calcification. Chest x-ray has limited sensitivity (64%) and specificity (86%) in the diagnosis of aortic diseases. It also worth mentioning that a normal chest x-ray may not rule out the diagnosis of aortic dissection.
Chest X Ray
- Findings on chest x-ray suggestive of aortic dissection include:[1]
- Widening of mediastinum
- Wide aortic contour
- Tracheal deviation
- Aortic kinking
- The calcium sign - separation of the intimal calcification from the outer aortic soft tissue border by 10 mm [2]
- Pleural effusions may be noted
- According to one study, the following features were more likely to be observed on chest x-ray:
- Aortic kinking or tortuosity
- Displacement of previous calcification
- Wide aortic contour
- A 'normal' chest x-ray does not rule out the possibility of an aortic dissection.[3]
- Chest x-ray sensitivity for the diagnosis of aortic disease is 64%.[1]
- Chest x-ray specificity for the diagnosis of aortic disease is 86%.
- Chest x-ray has particularly low accuracy in the diagnosis of ascending aortic dissection.
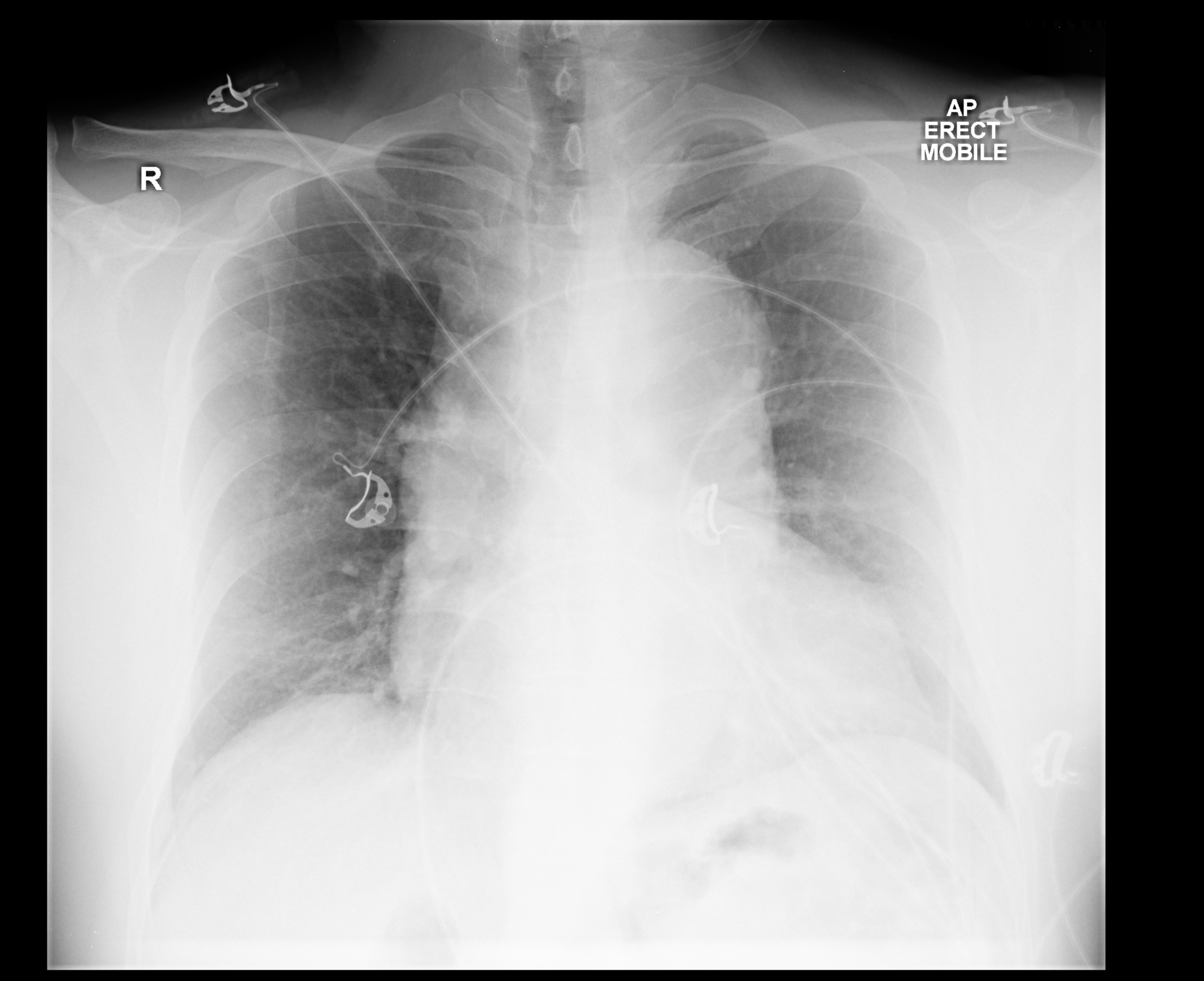
Chest X-Ray Examples of Aortic Dissection

2014 ESC Guidelines on the Diagnosis and Treatment of Aortic Diseases (DO NOT EDIT)[6]
| Class IIb |
| " Chest X-ray may be considered in cases of low clinical probability of AAS. (Level of Evidence: C)" |
2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the Diagnosis and Management of Patients With Thoracic Aortic Disease (DO NOT EDIT)[7]
Screening Tests (DO NOT EDIT)[7]
| Class I |
| "1. The role of chest x-ray in the evaluation of possible thoracic aortic disease should be directed by the patient's pretest risk of disease as follows: |
| a. Intermediate risk: Chest x-ray should be performed on all intermediate-risk patients, as it may establish a clear alternate diagnosis that will obviate the need for definitive aortic imaging. (Level of Evidence: C) |
| b. Low risk: Chest x-ray should be performed on all low-risk patients, as it may either establish an alternative diagnosis or demonstrate findings that are suggestive of thoracic aortic disease, indicating the need for urgent definitive aortic imaging. (Level of Evidence: C)" |
| Class III (No Benefit) |
| " 1. A negative chest x-ray should not delay definitive aortic imaging in patients determined to be high risk for aortic dissection by initial screening. (Level of Evidence: C)" |
References
- ↑ 1.0 1.1 von Kodolitsch Y, Nienaber CA, Dieckmann C, Schwartz AG, Hofmann T, Brekenfeld C, Nicolas V, Berger J, Meinertz T (January 2004). "Chest radiography for the diagnosis of acute aortic syndrome". Am. J. Med. 116 (2): 73–7. doi:10.1016/j.amjmed.2003.08.030. PMID 14715319.
- ↑ Gartland, S; Sookur, D; Lee, H (2007). "Aortic dissection: an x ray sign". Emergency Medicine Journal. 24 (4): 310–310. doi:10.1136/emj.2006.037010. ISSN 1472-0205.
- ↑ Hartnell, G. G.; Wakeley, C. J.; Tottle, A.; Papouchado, M.; Wilde, R. P. H. (1993). "Limitations of Chest Radiography in Discriminating Between Aortic Dissection and Myocardial Infarction". Journal of Thoracic Imaging. 8 (2): 152–155. doi:10.1097/00005382-199321000-00008. ISSN 0883-5993.
- ↑ Case courtesy of Dr Wayland Wang, Radiopaedia.org, rID: 50763
- ↑ Case courtesy of Dr Devanshi Pathania, Radiopaedia.org, rID: 68763
- ↑ "2014 ESC Guidelines on the diagnosis and treatment of aortic diseases". European Heart Journal. 35 (41): 2873–2926. 2014. doi:10.1093/eurheartj/ehu281. ISSN 0195-668X.
- ↑ 7.0 7.1 Hiratzka LF, Bakris GL, Beckman JA; et al. (2010). "2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine". Circulation. 121 (13): e266–369. doi:10.1161/CIR.0b013e3181d4739e. PMID 20233780. Unknown parameter
|month=ignored (help)