Anterior cruciate ligament injury
For patient information click here
| Anterior cruciate ligament injury | |
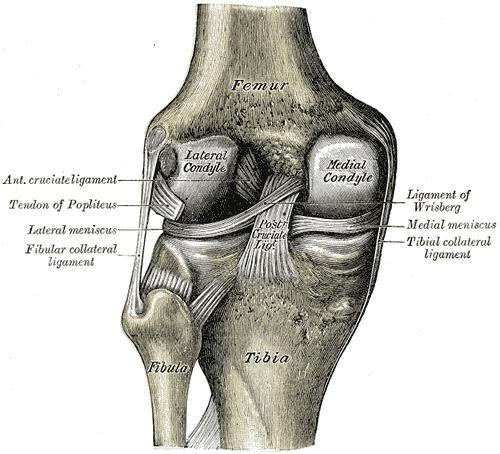
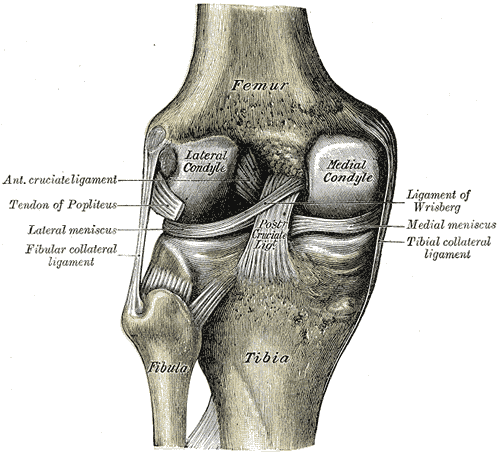
| Diagram of the right knee | |
| ICD-10 | S83.5 |
| ICD-9 | 844.2 |
| eMedicine | pmr/3 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
An injury to the anterior cruciate ligament can be a debilitating musculoskeletal injury seen most often in athletes. Non-contact tears and ruptures are the most common causes of ACL injury.
Causes
ACL injuries occur when an athlete rapidly decelerates, followed by a sharp or sudden change in direction (cutting). ACL failure has been linked to heavy or stiff-legged landing; as well as twisting or turning the knee while landing, especially when the knee is in the valgus (knock-knee) position.
Women in sports such as football, basketball, tennis and volleyball are significantly more prone to ACL injuries than men. The discrepancy has been attributed to differences between the sexes in anatomy, general muscular strength, reaction time of muscle contraction and coordination, and training techniques. A recent study suggests hormone-induced changes in muscle tension associated with menstrual cycles may also be an important factor [1]). Women have a relatively wider pelvis, requiring the femur to angle toward the knees[2].
The majority of ACL injuries occur in athletes landing flat on their heels. The latter directs the forces directly up the tibia into the knee, while the straight-knee position places the lateral femoral condyle on the back-slanted portion of the tibia. The resultant forward slide of the tibia relative to the femur is restrained primarily by the now-vulnerable ACL.
Diagnosis
The pivot-shift test, anterior drawer test and the Lachman test are used during the clinical examination of suspected ACL injury. The ACL can also be visualized using a magnetic resonance imaging scan (MRI scan).
Symptoms of an ACL injury include hearing a sudden popping sound, swelling, and instability of the knee (i.e., a "wobbly" feeling). Continued athletic activity on a knee with an ACL injury can have devastating consequences, resulting in massive cartilage damage, leading to an increased risk of developing osteoarthritis later in life.
ACL tear. Note the Segond fracture
Treatment
The ACL primarily serves to stabilize the knee in an extended position and when surrounding muscles are relaxed; so if the muscles are strong, many people can function without it.
The term for non-surgical treatment for ACL rupture is "conservative management", and it often includes physical therapy and using a knee brace. Lack of an ACL increases the risk of other knee injuries such as a torn meniscus, so sports with cutting and twisting motions are strongly discouraged. For patients who frequently participate in such sports, surgery is often indicated.
Surgery
There are two main options for ACL graft selection, allograft and autograft. Autografts are the patients' own tissues, and options include the hamstring tendons or middle third of the patella tendon. Allograft is cadaveric tissue sourced from a tissue bank. Each method has its own advantages and disadvantages; hamstring and middle third of patella tendon having similar outcomes. Patellar grafts are often incorrectly cited as being stronger, but the site of the harvest is often extremely painful for weeks after surgery and some patients develop chronic patellar tendinitis. Replacement via a posthumous donor involves a slightly higher risk of infection. Additionally, donor grafts eliminate tendon harvesting which, due to improved arthroscopic methods, is responsible for most post-operative pain.
The surgery is typically undertaken arthroscopically, with tunnels drilled into the femur and tibia at approximately the original ACL attachments. The graft is then placed into position and held in place. There are a variety of fixation devices available, particularly for hamstring tendon fixation. These include screws, buttons and post fixation devices. The graft typically attaches to the bone within six to eight weeks[3]. The original collagen tissue in the graft acts as a scaffold and new collagen tissue is laid down in the graft with time. Hence the graft takes over six months to reach maximal strength.[3]
After surgery, the knee joint loses flexibility, and the muscles around the knee and in the thigh tend to atrophy. All treatment options require extensive physical therapy to regain muscle strength around the knee and restore range of motion (ROM). For some patients, the lengthy rehabilitation period may be more difficult to deal with than the actual surgery. In general, a rehabilitation period of six months to a year is required to regain pre-surgery strength and use.[citation needed] This is very dependent on the rehabilitation assignment provided by the surgeon as well as the person who is receiving the surgery. External bracing is recommended for athletes in contact and collision sports for a period of time after reconstruction. It is important however to realize that this type of prevention is given by a 'surgeon to surgeon' basis; all surgeons will prescribe a brace and crutches for post surgery recovery total usage time is one month. After surgery no sports for 6 to 7 months. Whether the ACL deficient knee is reconstructed or not, the patient is susceptible to early onset of chronic degenerative joint disease.
See also
- Anterior cruciate ligament
- Skiing and skiing topics
- ACL reconstruction
- Sports injuries
- Lachman test
- Unhappy triad
Additional images
-
Right knee-joint, from the front, showing interior ligaments.
-
Left knee-joint from behind, showing interior ligaments.
References
- ↑ Catalyst: Weak at the Knees - ABC TV Science
- ↑ McLean SG, Huang X, van den Bogert AJ (2005). "Association between lower extremity posture at contact and peak knee valgus moment during sidestepping: implications for ACL injury". Clin Biomech (Bristol, Avon). 20 (8): 863–70. doi:10.1016/j.clinbiomech.2005.05.007. PMID 16005555.
- ↑ 3.0 3.1 Muller B, Bowman KF, Bedi A (2013). "ACL graft healing and biologics". Clin Sports Med. 32 (1): 93–109. doi:10.1016/j.csm.2012.08.010. PMID 23177465. Unknown parameter
|month=ignored (help)
- CS1 maint: Multiple names: authors list
- Pages with citations using unsupported parameters
- Pages with broken file links
- All articles with unsourced statements
- Articles with unsourced statements from October 2007
- Articles with invalid date parameter in template
- Traumatology
- Injuries
- Orthopedics
- Sports medicine
- Overview complete