Angular cheilitis
| Angular cheilitis | |
| ICD-10 | K13.0 |
|---|---|
| ICD-9 | 528.5 |
|
WikiDoc Resources for Angular cheilitis |
|
Articles |
|---|
|
Most recent articles on Angular cheilitis Most cited articles on Angular cheilitis |
|
Media |
|
Powerpoint slides on Angular cheilitis |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Angular cheilitis |
|
Clinical Trials |
|
Ongoing Trials on Angular cheilitis at Clinical Trials.gov Trial results on Angular cheilitis Clinical Trials on Angular cheilitis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Angular cheilitis NICE Guidance on Angular cheilitis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Angular cheilitis Discussion groups on Angular cheilitis Patient Handouts on Angular cheilitis Directions to Hospitals Treating Angular cheilitis Risk calculators and risk factors for Angular cheilitis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Angular cheilitis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Aakash Hans, MD[2]

Overview
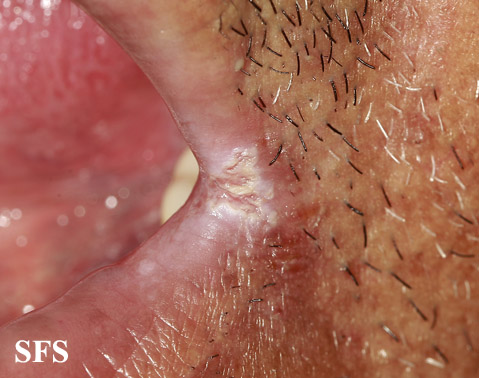
Angular cheilitis (also called perlèche, cheilosis or angular stomatitis) is an inflammatory lesion at the labial commissure, or corner of the mouth, and often occurs bilaterally. The condition manifests as deep cracks or splits. In severe cases, the splits can bleed when the mouth is opened and shallow ulcers or a crust may form. It usually occurs due to an underlying condition as the main cause. As the condition is generally mild, it has the propensity to go unnoticed for long periods of time. Identifying the underlying etiology is essential to decide the appropriate treatment. Altered structures of the mouth leads to approximation of the lips which causes pooling of the saliva at the angles of the mouth. It also presents as part of syndromes, especially those related to micro-nutrient deficiencies. Therefore, even after diagnosis, further testing should be done to rule out any underlying abnormalities which could later turn more sinister. The condition itself is manageable, resolves within two weeks if treatment is initiated on time and poses little to no risk to life. It rarely causes permanent disfigurement but it is notorious for recurrence if the contributing factors like oral health and denture care are not maintained hygienically or when treatment is taken inadequately. Ill-fitting dentures are also a common recurring cause of angular cheilitis.
Causes
Various etiologies are involved and often an interplay of all the factors is seen.
- Infections: Majority of the cases are due to combination of the microorganisms mentioned below. Out of these, candida and staphylococcus have the potential to be the sole cause of infection.
- Fungal: Candida is normally present in the oral cavity, but in its yeast form, which is non-pathogenic. Poor oral hygiene, dentures and uncontrolled diabetes are responsible for candida turning into its hyphal form (pathogenic) and increasing its number of colonies in the mouth. Subsequently the candida erodes the commissures, setting foundation for additional bacterial infection.
- Bacterial : Within the anterior portion of the nose, resides Staphylococcus aureus, which is another common cause of infection, given its proximity to the commissures. Streptococci is also prevalent in the nares and hence is occasionally isolated as cause of infection.
- Systemic diseases: The inability to absorb vital nutrients as a result of bowel inflammation, the healing processes get adversely affected in individuals with inflammatory bowel disease which in turn play a significant role in the development of cheilitis. Characterised by decreased salivary gland function and dry mouth, Sjögren's syndrome predisposes to angular cheilitis. Contrary to the pre-established pathophysiology of excess saliva being detrimental to the commissure, low levels of saliva is also damaging as it provides the lubrication to reduce friction at the commissures.
- Atopic dermatitis: Any allergy or irritant to the commissural skin has the possibility of causing angular cheilitis. Dental braces, mouthwash, lipsticks, toothpastes and foods with certain flavours and chemical preservatives, all are potentially capable of rendering chronic irritation at these skin folds.
- Micronutrient deficiency: Ranges from protein deficiency to iron, Vit B2, B9 and B12 and zinc deficiency.
- Recurrent insults to angle of mouth: Aggressive dental flossing, licking the commissures, sucking lollipops and candy and some medications like isotretinoin and certain chemotherapeutic drugs make the angles of the mouth more susceptible to inflammation followed by infection.
Epidemiology
Even though in the United States the prevalence is approximately in every 7 out of 1000 individuals, angular cheilitis is the most common form of lip infections (bacterial/fungal). It is more common in certain groups which are at a greater risk. These include persons who wear dentures, with certain conditions like inflammatory bowel disease, HIV-positive individual and other immunodeficiency states. Children and adults between 30-60 years are more frequently affected by angular cheilitis.
Pathophysiology
The most well understood mechanism behind angular cheilitis is the continuous exposure of the angles of the mouth to saliva. It may seem harmless, but saliva has various enzymes which when left for a prolonged period on the skin, can cause erosion and eventually weaken the physical barrier and integrity of the skin covering the angle of the mouth. This in turn makes the area vulnerable to higher chances of infection by various micro-organisms. Another factor is the angle of the mouth acting like a transition zone between the squamous epithelium of the face and the epithelium lining the oral cavity. It experiences increased amounts of shearing and frictional forces when the mouth opens and closes. These factors act together to weaken the commissures and provide an inlet for chemicals and infections to further damage the area.
Diagnosis
- Physical examination: Angles of mouth appear red and swollen with triangular lesions limited to the commissures in mild cases. Unless there are factors unequally affecting one side over the other, angular cheilitis lesions are commonly seen on both sides. Chronic inflammation can cause formation of fissures which follows the natural path of saliva flow to form, along the marionette lines. The oral mucosa should also be examined to detect oral thrush, which if present, should be treated.
- Investigations : Based on the impression about the possible cause, investigation should confirm the initial diagnosis.
Treatment
A multifaceted approach is essential in successful treatment. Once the infectious etiology is established, treatment is initiated with the appropriate anti-fungal or antibiotic. Initially the route of administration is topical which is then changed to systemic if the infection does not subside. Topical antifungals like Clotrimazole, ketoconazole ointments are available. Nystatin “swish and swallow” is often used for associated oral thrush. Systemic antifungals include fluconazole, itraconazole or capsofungin, all taken ideally once a day. Topical antiseptics like mupirocin ointment and fusidic acid cream are effective if bacterial cause is suspected. Thrice daily application is advised. Oral antibiotics are seldom used before confirmation of the causative bacteria through culture studies.