|
|
| Line 7: |
Line 7: |
| | DiseasesDB = | | | DiseasesDB = |
| | ICD10 = {{ICD10|N|14|0|n|10}} | | | ICD10 = {{ICD10|N|14|0|n|10}} |
| | ICD9 = {{ICD9|583.89}}, {{ICD9|584.7}} | | | ICD9 = {{ICD9|583.89}} |
| | ICDO = | | | ICDO = |
| | OMIM = | | | OMIM = |
| Line 18: |
Line 18: |
| {{SK}} Analgesic abuse nephropathy; analgesic-associated nephropathy; AAN | | {{SK}} Analgesic abuse nephropathy; analgesic-associated nephropathy; AAN |
|
| |
|
| '''Analgesic nephropathy''' is injury to the [[kidney]] caused by [[analgesic|analgesic medications]] such as [[aspirin]], [[phenacetin]], and [[paracetamol]]. The term usually refers to damage induced by excessive use of combinations of these medications, especially combinations that include phenacetin. It may also be used to describe kidney injury from any single analgesic medication.
| | ==[[Analgesic nephropathy overview|Overview]]== |
| | | ==[[Analgesic nephropathy historical perspective|Historical Perspective]]== |
| The specific kidney injuries induced by analgesics are [[renal papillary necrosis]] and [[interstitial nephritis|chronic interstitial nephritis]]. They appear to result from decreased [[renal blood flow|blood flow to the kidney]], rapid consumption of [[antioxidant]]s, and subsequent [[oxidative stress|oxidative damage]] to the kidney. This kidney damage may lead to progressive [[chronic renal failure]], abnormal [[urinalysis]] results, [[hypertension|high blood pressure]], and [[anemia]]. A small proportion of individuals with analgesic nephropathy may develop [[end-stage kidney disease]].
| | ==[[Analgesic nephropathy pathophysiology |Pathophysiology]]== |
| | | ==[[Analgesic nephropathy differential diagnosis|Differentiating Analgesic nephropathy from other Diseases]]== |
| Analgesic nephropathy was once a common cause of kidney injury and end-stage kidney disease in parts of Europe, Australia, and the United States. In most areas, its incidence has declined sharply since the use of phenacetin fell in the 1970s and 1980s. | | ==[[Analgesic nephropathy epidemiology and demographics|Epidemiology and Demographics]]== |
| | | ==[[Analgesic nephropathy risk factors|Risk Factors]]== |
| ==History==
| | ==[[Analgesic nephropathy natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| {{main|Phenacetin|Analgesic}}
| |
| | |
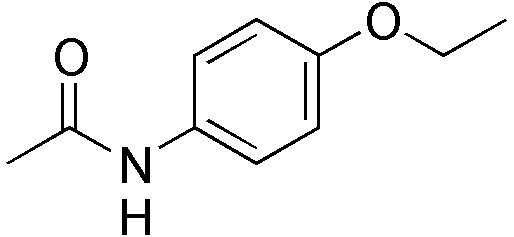
| [[Analgesic]]s are a class of medications widely used in the treatment of [[pain]]. They include [[aspirin]] and other [[non-steroidal anti-inflammatory drug]]s (NSAIDs), as well as the antipyretics [[paracetamol]] (known as acetaminophen in the United States) and [[phenacetin]]. Introduced in the late 19th century, phenacetin was once a common component of mixed analgesics in parts of Europe, Australia, and the United States.<ref name="pmid9734593">{{cite journal |author=McLaughlin JK, Lipworth L, Chow WH, Blot WJ |title=Analgesic use and chronic renal failure: a critical review of the epidemiologic literature |journal=Kidney Int. |volume=54 |issue=3 |pages=679–86 |year=1998 |month=September |pmid=9734593 |doi=10.1046/j.1523-1755.1998.00043.x |url=http://dx.doi.org/10.1046/j.1523-1755.1998.00043.x}}</ref> These combined analgesics contained aspirin or other NSAID with phenacetin, paracetamol, or salicylamide, and caffeine or codeine.<ref name="an-utd">{{cite book |last=de Broe |first=Marc E |editor=Curhan, Gary C (ed.) |title=UpToDate |accessdate=2008-09-30 |year=2008 |location=Waltham, MA |chapter=Analgesic nephropathy}}</ref>
| |
| | |
| In the 1950s, Spühler and Zollinger reported an association between kidney injury and the chronic use of phenacetin.<ref name="pmid13137299">{{cite journal |author=Spühler O, Zollinger HU |title=Die chronisch-interstitielle Nephritis. |language=German |journal=Z Klin Med |volume=151 |issue=1 |pages=1–50 |year=1953 |pmid=13137299 |doi= |url=}}</ref> They noted that chronic users of phenacetin had an increased risk of developing specific kidney injuries, namely [[renal papillary necrosis]] and [[interstitial nephritis|chronic interstitial nephritis]]. This condition was dubbed analgesic nephropathy and was attributed to phenacetin, although no absolute causative role was demonstrated. With further reports of the increased risk of kidney injury with prolonged and excessive phenacetin use, however, phenacetin was banned in several countries between the 1960s and 1980s.<ref name="pmid9734593"/>
| |
| | |
| As the use of phenacetin declined, so too did the prevalence of analgesic nephropathy as a cause of end-stage renal disease. Data from [[Switzerland]], for example, demonstrated a decline in the prevalence of analgesic nephropathy among patients with end-stage renal disease, from 28% in 1981 to 12% in 1990.<ref name="pmid7816247">{{cite journal |author=Brunner FP, Selwood NH |title=End-stage renal failure due to analgesic nephropathy, its changing pattern and cardiovascular mortality. EDTA-ERA Registry Committee |journal=Nephrol. Dial. Transplant. |volume=9 |issue=10 |pages=1371–6 |year=1994 |pmid=7816247 |doi= |url=http://ndt.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=7816247}}</ref> An autopsy study performed in Switzerland suggested that the prevalence of analgesic nephropathy in the general population has likewise decreased; the prevalence was 3% in 1980 and 0.2% in 2000.<ref name="pmid16891638"/>
| |
| | |
| While these data demonstrate that analgesic nephropathy has been all but eliminated in some regions, in other regions the condition persists. Notably, in Belgium, the prevalence of analgesic nephropathy among dialysis patients was 17.9% in 1984 and 15.6% in 1990.<ref name="pmid8177475">{{cite journal |author=Elseviers MM, de Broe ME |title=Analgesic nephropathy in Belgium is related to the sales of particular analgesic mixtures |journal=Nephrol. Dial. Transplant. |volume=9 |issue=1 |pages=41–6 |year=1994 |pmid=8177475 |doi= |url=http://ndt.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=8177475}}</ref><ref name="pmid7753450">{{cite journal |author=Noels LM, Elseviers MM, de Broe ME |title=Impact of legislative measures on the sales of analgesics and the subsequent prevalence of analgesic nephropathy: a comparative study in France, Sweden and Belgium |journal=Nephrol. Dial. Transplant. |volume=10 |issue=2 |pages=167–74 |year=1995 |pmid=7753450 |doi= |url=http://ndt.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=7753450}}</ref> Michielsen and de Schepper have suggested that analgesic nephropathy persists among Belgian dialysis patients not due to non-phenacetin analgesics, but because Belgium accepts a higher proportion of elderly patients for dialysis. According to these authors, a greater proportion have analgesic nephropathy because a greater percentage of Belgian dialysis patients have been exposed to long-term use of phenacetin.<ref name="pmid11181803">{{cite journal |author=Michielsen P, de Schepper P |title=Trends of analgesic nephropathy in two high-endemic regions with different legislation |journal=J. Am. Soc. Nephrol. |volume=12 |issue=3 |pages=550–6 |year=2001 |month=March |pmid=11181803 |doi= |url=http://jasn.asnjournals.org/cgi/pmidlookup?view=long&pmid=11181803}}</ref>
| |
| | |
| ==Pathophysiology==
| |
| The scarring of the small blood vessels, called capillary sclerosis, is the initial lesion of analgesic nephropathy.<ref name="pmid6641031">{{cite journal |author=Mihatsch MJ, Hofer HO, Gudat F, Knüsli C, Torhorst J, Zollinger HU |title=Capillary sclerosis of the urinary tract and analgesic nephropathy |journal=Clin. Nephrol. |volume=20 |issue=6 |pages=285–301 |year=1983 |month=December |pmid=6641031 |doi= |url=}}</ref> Found in the [[renal pelvis]], [[ureter]], and capillaries supplying the [[nephron]]s, capillary sclerosis is thought to lead to [[renal papillary necrosis]] and, in turn, [[interstitial nephritis|chronic interstitial nephritis]].<ref name="pmid16891638">{{cite journal |author=Mihatsch MJ, Khanlari B, Brunner FP |title=Obituary to analgesic nephropathy--an autopsy study |journal=Nephrol. Dial. Transplant. |volume=21 |issue=11 |pages=3139–45 |year=2006 |month=November |pmid=16891638 |doi=10.1093/ndt/gfl390 |url=http://ndt.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=16891638}}</ref><ref name="pmid6641031"/>
| |
| | |
| How phenacetin and other analgesics lead to this damage is incompletely understood. It is currently thought that the renal toxicities of NSAIDs and the antipyretics phenacetin and paracetamol may combine to give rise to analgesic nephropathy. A committee of investigators reported in 2000 that there was insufficient evidence to suggest that non-phenacetin analgesics by themselves are associated with analgesic nephropathy.<ref name="pmid11115060">{{cite journal |author=Feinstein AR, Heinemann LA, Curhan GC, ''et al'' |title=Relationship between nonphenacetin combined analgesics and nephropathy: a review. Ad Hoc Committee of the International Study Group on Analgesics and Nephropathy |journal=Kidney Int. |volume=58 |issue=6 |pages=2259–64 |year=2000 |month=December |pmid=11115060 |doi=10.1046/j.1523-1755.2000.00410.x |url=http://dx.doi.org/10.1046/j.1523-1755.2000.00410.x}}</ref>
| |
| | |
| ===Aspirin and NSAIDs===
| |
| Proper [[Renal function|kidney function]] depends upon adequate blood flow to the kidney. [[Renal blood flow|Kidney blood flow]] is a complex, tightly regulated process that relies on a number of [[hormone]]s and other small molecules, such as [[prostaglandin]]s. Under normal circumstances, [[prostaglandin E2]] (PGE<sub>2</sub>) produced by the kidney is necessary to support adequate blood flow to the kidney. Like all prostaglandins, PGE<sub>2</sub> synthesis depends upon the [[cyclooxygenase]]s.
| |
| | |
| Aspirin and other NSAIDs are inhibitors of the cyclooxygenases. In the kidney, this inhibition results in decreased PGE<sub>2</sub> concentration causing a reduction in blood flow. Because blood flow to the kidney first reaches the [[renal cortex]] (outside) and then the [[renal medulla]] (inside), the deeper structures of the kidney are most sensitive to decreased blood flow. Thus the innermost structures of the kidney, called the [[renal papilla]]e, are especially dependent on prostaglandin synthesis to maintain adequate blood flow. Inhibition of cyclooxygenases therefore rather selectively damages the renal papillae, increasing the risk of [[renal papillary necrosis]].<ref name="an-utd"/>
| |
| | |
| Most healthy kidneys contain enough physiologic reserve to compensate for this NSAID-induced decrease in blood flow. However, those subjected to additional injury from phenacetin or paracetamol may progress to analgesic nephropathy.
| |
| | |
| ===Phenacetin and paracetamol===
| |
| It is unclear how phenacetin induces injury to the kidney.<ref name="an-utd"/> Bach and Hardy have proposed that phenacetin's metabolites lead to [[lipid peroxidation]] that damages cells of the kidney.<ref name="pmid3910912">{{cite journal |author=Bach PH, Hardy TL |title=Relevance of animal models to analgesic-associated renal papillary necrosis in humans |journal=Kidney Int. |volume=28 |issue=4 |pages=605–13 |year=1985 |month=October |pmid=3910912 |doi= |url=}}</ref>
| |
| | |
| [[Paracetamol]] is the major metabolite of phenacetin and may contribute to kidney injury through a specific mechanism. In cells of the kidney, cyclooxygenases catalyse the conversion of paracetamol into [[NAPQI|''N''-acetyl-''p''-benzoquinoneimine]] (NAPQI).<ref name="pmid6798713">{{cite journal |author=Mohandas J, Duggin GG, Horvath JS, Tiller DJ |title=Metabolic oxidation of acetaminophen (paracetamol) mediated by cytochrome P-450 mixed-function oxidase and prostaglandin endoperoxide synthetase in rabbit kidney |journal=Toxicol. Appl. Pharmacol. |volume=61 |issue=2 |pages=252–9 |year=1981 |month=November |pmid=6798713 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/0041-008X(81)90415-4}}</ref> NAPQI depletes glutathione via non-enzymatic conjugation to [[glutathione]], a naturally occurring [[antioxidant]].<ref name="pmid8669429">{{cite journal |author=Duggin GG |title=Combination analgesic-induced kidney disease: the Australian experience |journal=Am. J. Kidney Dis. |volume=28 |issue=1 Suppl 1 |pages=S39–47 |year=1996 |month=July |pmid=8669429 |doi= |url=}}</ref> With depletion of glutathione, cells of the kidney become particularly sensitive to [[oxidative stress|oxidative damage]]. | |
| | |
| ==Clinical features==
| |
| {| class="wikitable" style="float:right; margin:10px"
| |
| |+ Clinical findings in analgesic nephropathy<ref name="pmid713270"/>
| |
| |-
| |
| ! Finding
| |
| ! Proportion affected
| |
| |-
| |
| | Headache
| |
| | 35-100%
| |
| |-
| |
| | Pyuria
| |
| | 50-100%
| |
| |-
| |
| | Anemia
| |
| | 60-90%
| |
| |-
| |
| | Hypertension
| |
| | 15-70%
| |
| |-
| |
| | Gastrointestinal symptoms
| |
| | 40-60%
| |
| |-
| |
| | Urinary tract infection
| |
| | 30-60%
| |
| |}
| |
| | |
| Common findings in patients with analgesic nephropathy include [[headache]], [[anemia]], high blood pressure ([[hypertension]]), and white blood cells in the urine ([[pyuria]]).<ref name="pmid713270">{{cite journal |author=Murray TG, Goldberg M |title=Analgesic-associated nephropathy in the U.S.A.: epidemiologic, clinical and pathogenetic features |journal=Kidney Int. |volume=13 |issue=1 |pages=64–71 |year=1978 |month=January |pmid=713270 |doi= |url=}}</ref> Some individuals with analgesic nephropathy may also have protein in their urine ([[proteinuria]]).<ref name="pmid362034">{{cite journal |author=Nanra RS, Stuart-Taylor J, de Leon AH, White KH |title=Analgesic nephropathy: etiology, clinical syndrome, and clinicopathologic correlations in Australia |journal=Kidney Int. |volume=13 |issue=1 |pages=79–92 |year=1978 |month=January |pmid=362034 |doi= |url=}}</ref>
| |
| | |
| ==Diagnosis== | | ==Diagnosis== |
| Diagnosis is traditionally based on the clinical findings above in combination with excessive analgesic use. It is estimated that between 2 and 3 kg each of phenacetin or aspirin must be consumed before evidence of analgesic nephropathy becomes clinically apparent.<ref name="an-utd"/>
| | [[Analgesic nephropathy history and symptoms|History and Symptoms]] | [[Analgesic nephropathy physical examination|Physical Examination]] | [[Analgesic nephropathy laboratory findings|Laboratory Findings]] | [[Analgesic nephropathy CT|CT]] |
| | |
| Once suspected, analgesic nephropathy can be confirmed with relative accuracy using [[computed tomography]] (CT) imaging without [[contrast medium|contrast]].<ref name="pmid9459649">{{cite journal |author=de Broe ME, Elseviers MM |title=Analgesic nephropathy |journal=N. Engl. J. Med. |volume=338 |issue=7 |pages=446–52 |year=1998 |month=February |pmid=9459649 |doi= |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=9459649&promo=ONFLNS19}}</ref> One trial demonstrated that the appearance of papillary calcifications on CT imaging was 92% [[sensitivity|sensitive]] and 100% [[specificity|specific]] for the diagnosis of analgesic nephropathy.<ref name="pmid8569094">{{cite journal |author=Elseviers MM, De Schepper A, Corthouts R, ''et al'' |title=High diagnostic performance of CT scan for analgesic nephropathy in patients with incipient to severe renal failure |journal=Kidney Int. |volume=48 |issue=4 |pages=1316–23 |year=1995 |month=October |pmid=8569094 |doi= |url=}}</ref>
| |
| | |
| ==Complications==
| |
| Complications of analgesic nephropathy include [[pyelonephritis]]<ref name="pmid10620560">{{cite journal |author=Maisonneuve P, Agodoa L, Gellert R, ''et al'' |title=Distribution of primary renal diseases leading to end-stage renal failure in the United States, Europe, and Australia/New Zealand: results from an international comparative study |journal=Am. J. Kidney Dis. |volume=35 |issue=1 |pages=157–65 |year=2000 |month=January |pmid=10620560 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0272638600765127}}</ref> and [[end-stage kidney disease]].<ref name="pmid7816247"/> Risk factors for poor prognosis include recurrent urinary tract infection and persistently elevated blood pressure.<ref name="pmid4638849"/> Analgesic nephropathy also appears to increase the risk of developing cancers of the [[urinary system]].<ref name="pmid7045494">{{cite journal |author=Blohmé I, Johansson S |title=Renal pelvic neoplasms and atypical urothelium in patients with end-stage analgesic nephropathy |journal=Kidney Int. |volume=20 |issue=5 |pages=671–5 |year=1981 |month=November |pmid=7045494 |doi= |url=}}</ref>
| |
| | |
| ==Treatment== | | ==Treatment== |
| Treatment of analgesic nephropathy begins with the discontinuation of analgesics, which often halts the progression of the disease and may even result in normalization of kidney function.<ref name="pmid4638849">{{cite journal |author=Linton AL |title=Renal disease due to analgesics. I. Recognition of the problem of analgesic nephropathy |journal=Can Med Assoc J |volume=107 |issue=8 |pages=749–51 |year=1972 |month=October |pmid=4638849 |pmc=1941002 |doi= |url=}}</ref>
| | [[Analgesic nephropathy medical therapy|Medical Therapy]] | [[Analgesic nephropathy future or investigational therapies|Future or Investigational Therapies]] |
| | | ==Case Studies== |
| ==Terminology== | | :[[Analgesic nephropathy case study one|Case #1]] |
| The term ''analgesic nephropathy'' usually refers to damage induced by excessive use of combinations of these medications, specifically combinations that include phenacetin. For this reason, it is also called '''analgesic abuse nephropathy'''. Others prefer the less judgmental '''analgesic-associated nephropathy'''.<ref name="pmid713270"/> Both terms are abbreviated to the acronym '''AAN''', by which the condition is also commonly known.
| |
| | |
|
| |
|
| {{Nephrology}} | | {{Nephrology}} |