|
|
| (13 intermediate revisions by 2 users not shown) |
| Line 4: |
Line 4: |
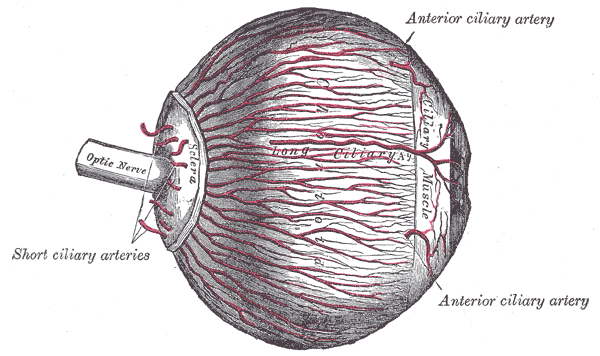
| | Image = Gray873.png | | | Image = Gray873.png |
| | Caption = The arteries of the choroid and iris. The greater part of the sclera has been removed. | | | Caption = The arteries of the choroid and iris. The greater part of the sclera has been removed. |
| | DiseasesDB = 501
| |
| | ICD10 = {{ICD10|G|45|3|g|40}}
| |
| | ICD9 = {{ICD9|362.34}}
| |
| | ICDO =
| |
| | OMIM =
| |
| | MedlinePlus = 000784
| |
| | MeshID = D020757
| |
| }} | | }} |
| {{Amaurosis fugax}} | | {{Amaurosis fugax}} |
| | '''For patient information, click [[Amaurosis fugax (patient information)|here]] |
| | ''' |
| | |
| {{CMG}} | | {{CMG}} |
|
| |
|
| {{Editor join}} | | {{SK}} Transient monocular blindness |
|
| |
|
| ==Pathophysiology== | | ==[[Amaurosis fugax overview|Overview]]== |
|
| |
|
| Prior to 1990, amaurosis fugax could, "clinically, be divided into four identifiable symptom complexes, each with its underlying pathoetiology: embolic, hypoperfusion, angiospasm, and unknown."<ref name="Burde">Burde RM. "Amaurosis fugax. An overview." ''J Clin Neuroophthalmol.'' 1989 Sep;9(3):185-9. PMID 2529279</ref> In 1990, the causes of amaurosis fugax were better refined by Amaurosis Fugax Study Group, which has defined five distinct causes of transient monocular blindness: embolic, hemodynamic, ocular, neurologic, and idiopathic.<ref name="ASG">The Amaurosis Fugax Study Group. [http://stroke.ahajournals.org/cgi/reprint/21/2/201.pdf "Current management of amaurosis fugax."] ''Stroke.'' 1990;21(2):201-208.</ref> Concerning the pathology underlying these causes (stay [[idiopathic]]), "some of the more frequent causes include atheromatous disease of the internal carotid or [[ophthalmic artery]], [[vasospasm]], [[optic neuropathy]], [[giant cell arteritis]], [[angle-closure glaucoma]], increased intracranial pressure, orbital compressive disease, a [[steal phenomenon]], and blood hyperviscosity or hypercoagulability."<ref name="Newman">Newman NJ. "Cerebrovascular disease." ''Walsh & Hoyt's Clinical Neuro-Ophthalmology.'' (Miller NR, Newman NJ, eds.) Vol 3. 5th ed. Baltimore, Williams & Wilkins; 1998:3420-3426.</ref>
| | ==[[Amaurosis fugax historical perspective|Historical Perspective]]== |
|
| |
|
| ===Embolic and Hemodynamic Origin=== | | ==[[Amaurosis fugax pathophysiology|Pathophysiology]]== |
| With respect to embolic and hemodynamic causes, this transient monocular visual loss ultimately occurs due to a temporary reduction in [[retinal artery]], [[ophthalmic artery]], or [[Ciliary arteries|ciliary artery]] blood flow, leading to a decrease in retinal circulation which, in turn, causes retinal hypoxia.<ref name="vasospastic">[http://archopht.ama-assn.org/cgi/content/extract/120/2/220 "Exercise-Induced Vasospastic Amaurosis Fugax."] ''Arch Ophthalmol.'' 2002 February;120(2):220-222.</ref> Also, it must be noted that while, classically and most commonly, emboli causing amaurosis fugax are described as coming from an atherosclerotic [[carotid artery]], any emboli arising from vasculature preceding the [[retinal artery]], [[ophthalmic artery]], or [[ciliary arteries]] may cause this transient monocular blindness.
| |
|
| |
|
| *Atherosclerotic [[carotid artery]]: Amaurosis fugax may present as a type of [[transient ischemic attack]] (TIA), during which an [[embolus]] unilaterally obstructs the lumen of the [[retinal artery]] or [[ophthalmic artery]], causing a decrease in blood flow to the ipsilateral retina. The most common source of these thromboemboli is an atherosclerotic carotid artery.<ref name="braat">Braat, Andries; Peter H. Hoogland, A.C. DeVries, J.C. Alexander de Mol VanOtterloo. [http://ves.sagepub.com/cgi/content/abstract/35/2/141 "Amaurosis Fugax and Stenosis of the Ophthalmic Artery."] ''Vascular and Endovascular Surgery.'' 2001;35(2):141-142.</ref><br> However, a severely atherosclerotic [[carotid artery]] may also cause amaurosis fugax due to its stenosis of blood flow, leading to ischemia when the retina is exposed to bright light.<ref name="Kaiboriboon">Kaiboriboon K; Piriyawat P; Selhorst JB. "Light-induced amaurosis fugax." ''Am J Ophthalmol.'' 2001 May;131(5):674-6. PMID 11336956.</ref> "Unilateral visual loss in bright light may indicate ipsilateral carotid artery occlusive disease and may reflect the inability of borderline circulation to sustain the increased retinal metabolic activity associated with exposure to bright light."<ref name="Furlan">AU Furlan AJ; Whisnant JP; Kearns TP. "Unilateral visual loss in bright light. An unusual symptom of carotid artery occlusive disease." ''Arch Neurol.'' 1979 Nov;36(11):675-6. PMID 508123.</ref>
| | ==[[Amaurosis fugax causes|Causes]]== |
|
| |
|
| *Atherosclerotic [[ophthalmic artery]]: Will present similarly to an atherosclerotic internal carotid artery.
| | ==[[Amaurosis fugax differential diagnosis|Differentiating Amaurosis fugax from other Diseases]]== |
|
| |
|
| *Cardiac [[emboli]]: Emboli arising from the heart may also cause luminal obstruction of the retinal, ophthalmic, and/or ciliary arteries, causing a decrease in blood flow to the ipsilateral retina; examples being those arising due to (1) [[atrial fibrillation]], (2) valvular abnormalities including post-rheumatic valvular disease, [[mitral valve prolapse]], and a [[bicuspid aortic valve]], and (3) [[atrial myxoma]]s.
| | ==[[Amaurosis fugax epidemiology and demographics|Epidemiology and Demographics]]== |
|
| |
|
| *Temporary [[vasospasm]] leading to decreased blood flow can be a cause of amaurosis fugax.<ref name="Ellenberger">Ellenberger C Jr., Epstein AD. "Ocular complications of atherosclerosis: what do they mean?" ''Semin Neurol.'' 1986;6:185-193.</ref><ref name="Fisher">Fisher M. "Transient monocular blindness associated with hemiplegia." ''Arch Ophthalmol.'' 1952;47:167-203.</ref> Generally, these episodes are brief, lasting no longer that five minutes,<ref name="stephen">Burger, Stephen; robert Saul, John Selhorst, Stephen Thurston. "Transient monocular blindness caused by vasospasm." ''The New England Journal of Medicine.'' 1991;325:870-873.</ref> and have been associated with exercise.<ref name="vasospastic" /><ref name="Imes">Imes RK, Hoyt WF. "Exercise-induced transient visual events in young healthy adults." ''J Clin Neuro Ophthalmol.'' 1989:9;9:178-180.</ref> These vasospastic episodes are not restricted to young and healthy individuals. "Observations suggest that a systemic hemodynamic challenge provoke[s] the release of vasospastic substance in the rentinal vasculature of one eye."<ref name="stephen" />
| | ==[[Amaurosis fugax risk factors|Risk Factors]]== |
|
| |
|
| *[[Giant cell arteritis]]: Giant cell arteritis can result in granulomatous inflammation within the central [[retinal artery]] and posterior ciliary arteries of eye, resulting in partial or complete occlusion, leading to decreased blood flow manifesting as amaurosis fugax. Commonly, amaurosis fugax caused by [[giant cell arteritis]] may be associated with [[jaw claudication]] and [[headache]]. However, it is also not uncommon for these patients to have no other symptoms.<ref name="Hayreh2">AU Hayreh SS; Podhajsky PA; Zimmerman B. "Occult giant cell arteritis: ocular manifestations." ''Am J Ophthalmol.'' 1998 Apr;125(4):521-6. PMID 9559738.</ref> One comprehensive review found a two to nineteen percent incidence of amaurosis fugax among these patients.<ref name="goodman">Goodman BW Jr. "Temporal arteritis." ''Am J Med.'' 1979;67:839-852.</ref>
| | ==[[Amaurosis fugax natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
|
| |
|
| *[[Systemic lupus erythematosus]]<ref name="giorgi">Giorgi, Afeltra, Gabrieli. "Transient visual symptoms in systemic lupus erthematosus and antiphospholipid syndrome." ''Ocular Immunology and Inflammation.'' March 2001;9(1):49-57.</ref><ref name="GoldD">Gold D, Feiner L, Henkind P. "Retinal arterial occlusive disease in systemic lupus erythematosus." ''Arch Ophthalmol.'' 1977;95:1580-1585.</ref>
| | ==Diagnosis== |
|
| |
|
| *[[Periarteritis nodosa]]<ref name="NewmanNM">Newman NM, Hoyt WF, Spencer WH. "Macula-sparing blackouts: clinical and pathologic investigations of intermittent choroidal vascular insufficiency in a case of periarteritis nodosa." ''Arch Ophthalmol.'' 1974; 91:367-370.</ref>
| | [[Amaurosis fugax diagnostic evaluation|Diagnostic Evaluation]] | [[Amaurosis fugax history and symptoms|History and Symptoms]] | [[Amaurosis fugax physical examination|Physical Examination]] | [[Amaurosis fugax laboratory findings|Laboratory Findings]] | [[Amaurosis fugax CT|CT]] | [[Amaurosis fugax MRI|MRI]] | [[Amaurosis fugax echocardiography or ultrasound|Echocardiography or Ultrasound]] | [[Amaurosis fugax other imaging findings|Other Imaging Findings]] |
|
| |
|
| *[[Eosinophilia|Eosinophilic]] [[vasculitis]]<ref name="Schwartz">Schwartz ND, So YT, Hollander H, Allen S, Fye KH. "Eosinophilic vasculitis leading to amaurosis fugax in a patient with acquired immunodeficiency syndrome." ''Arch Intern Med.'' 1986;146:2059-2060</ref>
| | ==Treatment== |
| | |
| *[[Hyperviscosity syndrome]]<ref name="Bacigalupi" />
| |
| **[[Polycythemia]]<ref name="Berdel">Berdel, Theiss, Fink, Rastetter. "Peripheral arterial occlusion and amaurosis fugax as the first manifestation of polycythemia vera." ''Journal Annals of Hematology.'' 1984;48(3):177-180.</ref>
| |
| | |
| *[[Hypercoagulability]]<ref name="Mundall">Mundall, Quintero, von Kaulla, Harmon, Austin. "Transient monocular blindness and increased platelet aggregability treated with aspirin." ''Neurology.'' 1972;22:280-285.</ref>
| |
| **[[Protein C deficiency]]<ref name="smith_db">Smith. "Protein C deficiency: A cause of amaurosis fugax?" ''Neurol Neurosurg Psychiatry.'' 1987;50:361-362.</ref>
| |
| **[[Antiphospholipid antibodies]]<ref name="Digre">Digre, Durcan, Branch, Jacobson, Varner, Baringer. "Amaurosis fugax associated with antiphospholipid antibodies." ''Ann Neurol.'' 1989;25:228-232.</ref>
| |
| ***[[Anticardiolipin antibodies]]<ref name="DigreK" />
| |
| ***[[Lupus anticoagulant]]<ref name="Landi">Landi, Calloni, Sabbadini, Mannucci, Candelise. "Recurrent ischemic attacks in two young adults with lupus anticoagulants." ''Stroke.'' 1983;14:377-379.</ref><ref name="Elias">Elias M, Eldor A. "Thromboembolism in patients with the 'lupus'-type circulating anticoagulant." ''arch Intern Med.'' 1984;144:510-515.</ref>
| |
| | |
| *[[Thrombocytosis]]<ref name="DigreK" />
| |
| | |
| *[[Subclavian steal syndrome]]
| |
| | |
| *[[Malignant hypertension]] can cause ischemia of the optic nerve head leading to transient monocular visual loss.<ref name="HayrehSS">Hayreh SS, Servais GE, Virdi PS. "Fundus lesions in malignant hypertension, V. hypertensive optic neuropathy." ''Ophthalmology.'' 1986;93:74-87.</ref>
| |
| | |
| *Drug abuse-related intravascular emboli<ref name="ASG" />
| |
| | |
| *[[Iatrogenic]]: Amaurosis fugax can present as a complication following [[carotid endarterectomy]], carotid [[angiography]], [[cardiac catheterization]], and [[CABG|CABG surgery]].<ref name="DigreK" />
| |
| | |
| ===Ocular origin===
| |
| Ocular causes include:
| |
| *[[Iritis]]<ref name="Sorensen">Sorensen PN. "Amaurosis fugax. A unselected material." ''Acta Ophthalmol (Copenh).'' 1983 Aug;61(4):583-8. PMID: 6637419.</ref>
| |
| *[[Keratitis]]<ref name="Bacigalupi">Bacigalupi, Michael. [http://ijahsp.nova.edu/articles/vol4num2/Bacigalupi.pdf "Amaurosis Fugax-A Clinical Review."] ''The Internet Journal of Allied Health Sciences and Practice.'' April 2006;4(2):1-6.</ref>
| |
| *[[Blepharitis]]<ref name="Bacigalupi" />
| |
| *[[Optic disc drusen]]<ref name="DigreK" />
| |
| *[[Posterior vitreous detachment]]<ref name="Bacigalupi" />
| |
| *[[glaucoma|Closed-angle glaucoma]]<ref name="Ravits">Ravits J, Seybold M. "Transient monocular visual loss from narrow-angle glaucoma." ''Arch Neurol.'' 1984;41:991-993.</ref>
| |
| *Transient elevation of intraocular pressure<ref name="ASG" /><ref name="Sorensen" />
| |
| *Intraocular [[hemorrhage]]<ref name="ASG" />
| |
| *[[Coloboma]]<ref name="DigreK" />
| |
| *[[Myopia]]<ref name="DigreK" />
| |
| *Orbital [[hemangioma]]<ref name="BrownGC">Brown GC, Shields JA. "Amaurosis fugax secondary to presumed cavernous hemangioma of the orbic." ''Ann Ophthalmol.'' 1981;13:1205-12O9.</ref>
| |
| *Orbital [[osteoma]]<ref name="WilkesSR">Wilkes SR, Troutmann JC, DeSanto LW, Campbell RJ. "Osteoma. An unusual cause of amaurosis fugax." ''Mayo Clin Proc.'' 1979;54:258-260.</ref>
| |
| *[[Keratoconjunctivitis sicca]]<ref name="DigreK" />
| |
| | |
| ===Neurologic origin===
| |
| Neurological causes include:
| |
| *[[Optic neuritis]]<ref name="ASG" />
| |
| | |
| *Compressive [[optic neuropathy|optic neuropathies]]<ref name="ASG" /><ref name="DigreK">Digre, Kathleen. [http://intl.elsevierhealth.com/e-books/pdf/783.pdf "Amaurosis Fugax and Not So Fugax—Vascular Disorders of the Eye."] ''Practical Viewing of the Optic Disc.'' Butterworth Heinemann: November 2002:269-344.</ref>
| |
| | |
| *[[Papilledema]]: "The underlying mechanism for visual obscurations in all of these patients appear to be transient ischemia of the optic nerve head consequent to increased tissue pressure. Axonal swelling, intraneural masses, and increased influx of interstitial fluid may all contribute to increases in tissue pressure in the optic nerve head. The consequent reduction in perfusion pressure renders the small, low-pressure vessels that supply the optic nerve head vulnerable to compromise. Brief fluctuations in intracranial or systemic blood pressure may then result in transient loss of function in the eyes."<ref name="Sadun">AU Hayreh SS; Podhajsky PA; Zimmerman B. "Transient visual obscurations with elevated optic discs." ''Ann Neurol.'' 1984 Oct;16(4):489-94. PMID 6497356.</ref> Generally, this transient visual loss is also associated with a headache and optic disk swelling.
| |
| | |
| *[[Multiple Sclerosis]] can cause amaurosis fugax due to a unilateral conduction block, which is a result of demyelination and inflammation of the optic nerve, and "...possibly by defects in synaptic transmission and putative circulating blocking factors."<ref name="Smith">AU Smith KJ; McDonald WI. "The pathophysiology of multiple sclerosis: the mechanisms underlying the production of symptoms and the natural history of the disease." ''Philos Trans R Soc Lond B Biol Sci.'' 1999 October 29;354(1390):1649-73. PMID 10603618.</ref>
| |
| | |
| *[[Migrane]]<ref name="mattsson">Mattsson, Lundberg. "Characteristics and prevalence of transient visual disturbances indicative of migraine visual aura." ''Cephalalgia.'' June 1999;19(5):447.</ref><ref name="cologno">Cologno, Torelli, Manzoni. "Transient vidual disturbances during migraine without aura attacks." ''Headache.'' October 2002;42(9):930-933.</ref><ref name="ConnorRCR">Connor RCR. "Complicated migraine: A study of permanent neurological and visual defects caused by migraine." ''Lancet.'' 1962;2:1072-1075.</ref><ref name="CarrollD">Carroll D. "Retinal migraine." ''Headache.'' 1970;10:9-13.</ref><ref name="McDonaldWI">McDonald WI, Sanders MD. "Migraine complicated by ischemic papillopathy." ''Lancet.'' 1971;2:521-523.</ref><ref name="WolterJR">Wolter JR, Burchfield WJ. "Ocular migraine in a young man resulting in unilateral transient blindness and retinal edema." ''Pediatr Ophthalmol.'' 1971;8:173-176.</ref><ref name="KlineLB">Kline LB, Kelly CL. "Ocular migraine in a patient with cluster headaches." ''Headache.'' 1980;20:253-257.</ref><ref name="CorbettJJ">Corbett JJ. "Neuro-ophthalmologic complications of migraine and cluster headaches." ''Neurol Clin.'' 1983;l:973-995.</ref>
| |
|
| |
|
| *[[Pseudotumor cerebri]]<ref name="HedgesT" />
| | [[Amaurosis fugax medical therapy|Medical Therapy]] | [[Amaurosis fugax surgery|Surgery]] | [[Amaurosis fugax primary prevention|Primary Prevention]] | [[Amaurosis fugax secondary prevention|Secondary Prevention]] | [[Amaurosis fugax cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Amaurosis fugax future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| *[[Intracranial tumor]]<ref name="HedgesT">Hedges, Thomas. [http://stroke.ahajournals.org/cgi/reprint/15/5/907.pdf "The Terminology of Transient Visual Loss Due to Vascular Insufficiency."] ''Stroke.'' 1984; 15(5):907-908.</ref>
| | ==Case Studies== |
| | | :[[Amaurosis fugax case study one|Case #1]] |
| *[[Psychogenic]]<ref name="Bacigalupi" />
| |
| | |
| ==Symptoms== | |
| The experience of amaurosis fugax is classically described as a transient monocular vision loss that appears as a "[[curtain]] coming down vertically into the [[visual field|field of vision]] in one eye;" however, this altitudinal visual loss is relatively uncommon. In one study, only 23.8 percent of patients with transient monocular vision loss experienced the classic "curtain" or "shade" descending over their vision.<ref name="noauthor">"Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis." ''N Engl J Med.'' 1991 August 15;325(7):445-53. PMID 1852179.</ref> Other descriptions of this experience include a monocular blindness, dimming, fogging, or blurring.<ref name="Lord">Lord RS. "Transient monocular blindness." ''Aust N Z J Ophthalmol.'' 1990 Aug;18(3):299-305. PMID 2261177.</ref> Total or sectorial [[vision loss]] typically lasts only a few seconds, but may last minutes or even hours. Duration depends on the etiology of the vision loss. Obscured vision due to papilledema may last only seconds, while a severely atherosclerotic carotid artery may be associated with a duration of one to ten minutes.<ref name="Donders">Donders RC. "Clinical features of transient monocular blindness and the likelihood of atherosclerotic lesions of the internal carotid artery." ''J Neurol Neurosurg Psychiatry.'' 2001 Aug;71(2):247-9. PMID 11459904.</ref> Certainly, additional symptoms may be present with the amaurosis fugax, and those findings will depend on the etiology of the transient monocular vision loss.
| |
| | |
| ==Diagnostic Evaluation==
| |
| Despite the temporary nature of the vision loss, those experiencing amaurosis fugax are usually advised to consult a [[physician]] immediately as it is a [[symptom]] that usually heralds serious vascular events, including [[stroke]].<ref name="benavente">Benavente, Eliasziw, Steifler, Fox, et al. "Prognosis after transient monocular blindness associated with carotid-artery stenosis." ''N Engl J Med.'' 2001;345(15):1084-1090.</ref><ref name="rothwell">Rothwell, Warlow. "Timing of TIA's preceding stroke: time window for prevention is very short." ''Neurology.'' 2005;64:817.</ref> Restated, “because of the brief interval between the transient event and a stroke or blindness from temporal arteritis, the workup for transient monocular blindness should be undertaken without delay.” If the patient has no history of giant cell arteritis, the probability of vision preservation is high; however, the chance of a stroke reaches that for a hemispheric TIA. Therefore, investigation of cardiac disease is justified.<ref name="ASG" />
| |
| | |
| A diagnostic evaluation should begin with the patient's history, followed by a physical exam, with particular importance being paid to the ophthalmic examination with regards to signs of ocular ischemia. When investigating amaurosis fugax, an ophthalmologic consult is absolutely warranted if available. Several concomitant laboratory tests should also be ordered to investigate some of the more common, systemic causes listed above, including a complete blood count, erythrocyte sedimentation rate, lipid panel, and blood glucose level. If a particular etiology is suspected based on the history and physical, additional relevant labs should be ordered.<ref name="ASG" />
| |
| | |
| If laboratory tests are abnormal, a systemic disease process is likely, and, if the ophthalmologic examinaton is abnormal, ocular disease is likely. However, in the event that both of these routes of investigation yield normal findings, or an inadequate explanation, noninvasive duplex ultrasound studies are recommended to identify carotid artery disease. Most episodes of amaurosis fugax are the result of stenosis of the ipsilateral carotid artery.<ref name="smit">Smit, Ronald; G. Seerp Baarsma and Peter J. Koudstaal [http://www.iovs.org/cgi/reprint/1/1/136.pdf "The source of embolism in amaurosis fugax and retinal artery occlusion."] ''International Ophthalmology.'' 1994 March;18(2):83-86. ISSN 0165-5701.</ref> With that being the case, researchers investigated how best to evaluate these episodes of vision loss, and concluded that for patients ranging from 36-74 years old, "...carotid artery duplex scanning should be performed...as this investigation is more likely to provide useful information than an extensive cardiac screening (ECG, Holler 24-hour monitoring and precordial echocardiography)."<ref name="smit"/> Additionally, concomitant head CT or MRI imaging is also recommended to investigate the presence of a “clinically silent cerebral embolism.”<ref name="ASG" />
| |
| | |
| If the results of the ultrasound and intracranial imaging are normal, “renewed diagnostic efforts may be made,” during which [[fluorescein angiography]] is an appropriate consideration. However, carotid angiography is not advisable in the presence of a normal ultrasound and CT.<ref name="walsh">Walsh J, Markowitz I, Kerstein MD. "Carotid endarterectomy for amaurosis fugax without angiography." ''Am J Surg.'' 1986 Aug;152(2):172-4. PMID 3526933.</ref>
| |
| | |
| ==Differential Diagnosis of Amaurosis fugax==
| |
| {|style="width:80%; height:100px" border="1"
| |
| |style="height:100px"; style="width:25%" border="1" bgcolor="LightSteelBlue" | '''Cardiovascular'''
| |
| |style="height:100px"; style="width:75%" border="1" bgcolor="Beige" | No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Chemical / poisoning'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Dermatologic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Drug Side Effect'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Ear Nose Throat'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Endocrine'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Environmental'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Gastroenterologic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Genetic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Hematologic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Iatrogenic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Infectious Disease'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Musculoskeletal / Ortho'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Neurologic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Nutritional / Metabolic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Oncologic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Opthalmologic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Overdose / Toxicity'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Psychiatric'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Pulmonary'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Renal / Electrolyte'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Rheum / Immune / Allergy'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Trauma'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Miscellaneous'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |}
| |
| | |
| ==Treatment==
| |
| | |
| If the diagnostic workup reveals a systemic disease process, directed therapies to treat that underlying etiology should be initiated. If the amaurosis fugax is caused by an atherosclerotic lesion, [[aspirin]] is indicated, and a [[carotid endarterectomy]] if the stenosis is surgically accessible. Generally, if the carotid artery is still patent, the greater the stenosis, the greater the indication for endarterectomy. "Amaurosis fugax appears to be a particularly favorable indication for carotid endarterectomy. Left untreated, this event carries a high risk of stroke; after carotid endarterectomy, which has a low operative risk, there is a very low postoperative stroke rate."<ref name="bernstein">Bernstein EF, Dilley RB. "Late results after carotid endarterectomy for amaurosis fugax." ''J Vasc Surg.'' 1987 Oct;6(4):333-40. PMID 3656582.</ref> If the full diagnostic workup is completely normal, patient observation is recommended.<ref name="ASG" />
| |
|
| |
|
| ==Related Chapters== | | ==Related Chapters== |
| *[[Ocular ischemic syndrome]] | | *[[Ocular ischemic syndrome]] |
| *[[Amaurosis]] | | *[[Amaurosis]] |
|
| |
| ==References==
| |
| {{reflist|2}}
| |
|
| |
|
| |
|
| |
|
| {{Diseases of the nervous system}} | | {{Diseases of the nervous system}} |
| [[de:Retinaler Arterienverschluss]]
| |
| [[zh:一过性黑蒙]] | | [[zh:一过性黑蒙]] |
|
| |
|
| |
|
| |
|
| [[Category:Cardiovascular diseases]] | | [[Category:Cardiovascular diseases]] |
| [[Category:Ophthalmology]] | | [[Category:Ophthalmology]] |
| [[Category:Neurology]] | | [[Category:Neurology]] |
| [[Category:Symptoms]]
| |
| [[Category:Signs and symptoms]]
| |
| [[Category:Ddx]] | | [[Category:Ddx]] |
| {{WikiDoc Help Menu}} | | |
| {{WikiDoc Sources}} | | {{WH}} |
| | {{WS}} |