Alcoholism: Difference between revisions
No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
{{alcohealth}} | {{alcohealth}} | ||
{{ | {{Alcoholism}} | ||
{{CMG}} | {{CMG}} | ||
Revision as of 20:25, 31 August 2012
For patient information, click here
|
Alcoholism Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Alcoholism On the Web |
|
American Roentgen Ray Society Images of Alcoholism |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Alcoholism is a term with multiple and sometimes conflicting definitions. In common and historic usage, alcoholism refers to any condition that results in the continued consumption of alcoholic beverages despite the health problems and negative social consequences it causes. Medical definitions describe alcoholism as a disease which results in a persistent use of alcohol despite negative consequences. Alcoholism may also refer to a preoccupation with or compulsion toward the consumption of alcohol and/or an impaired ability to recognize the negative effects of excessive alcohol consumption. Although not all of these definitions specify current and on-going use of alcohol as a qualifier, some do, as well as remarking on the long-term effects of consistent, heavy alcohol use, including dependence and symptoms of withdrawal.
While the ingestion of alcohol is, by definition, necessary to develop alcoholism, the use of alcohol does not predict the development of alcoholism. The quantity, frequency and regularity of alcohol consumption required to develop alcoholism varies greatly from person to person. In addition, although the biological mechanisms underpinning alcoholism are uncertain, some risk factors, including social environment, emotional health and genetic predisposition, have been identified.

Definitions and terminology
The definitions of alcoholism and related terminology vary significantly between the medical community, treatment programs, and the general public.
Medical definitions
The Journal of the American Medical Association defines alcoholism as "a primary, chronic disease characterized by impaired control over drinking, preoccupation with the drug alcohol, use of alcohol despite adverse consequences, and distortions in thinking."[1]
The DSM-IV (the standard for diagnosis in psychiatry and psychology) defines alcohol abuse as repeated use despite recurrent adverse consequences.[2] It further defines alcohol dependence as alcohol abuse combined with tolerance, withdrawal, and an uncontrollable drive to drink.[2] (See DSM diagnosis below.)
According to the APA Dictionary of Psychology, alcoholism is the popular term for alcohol dependence.[2] Note that there is debate whether dependence in this use is physical (characterised by withdrawal), psychological (based on reinforcement), or both.
Terminology
Many terms are applied to a drinker's relationship with alcohol. Use, misuse, heavy use, abuse, addiction, and dependence are all common labels used to describe drinking habits, but the actual meaning of these words can vary greatly depending upon the context in which they are used. Even within the medical field, the definition can vary between areas of specialization. The introduction of politics and religion further muddles the issue.
Use refers to simple use of a substance. An individual who drinks any alcoholic beverage is using alcohol. Misuse, problem use, and heavy use do not have standard definitions, but suggest consumption of alcohol to the point where it causes physical, social, or moral harm to the drinker. The definitions of social and moral harm are highly subjective and therefore differ from individual to individual.
Within politics, abuse is often used to refer to the illegal use of any substance. Within the broad field of medicine, abuse sometimes refers to use of prescription medications in excess of the prescribed dosage, sometimes refers to use of a prescription drug without a prescription, and sometimes refers to use that results in long-term health problems. Within religion, abuse can refer to any use of a poorly regarded substance. The term is often avoided because it can cause confusion with audiences that do not necessarily share a single definition.
Remission is often used to refer to a state where an alcoholic is no longer showing symptoms of alcoholism. The American Psychiatric Association considers remission to be a condition where the physical and mental symptoms of alcoholism are no longer evident, regardless of whether or not the person is still drinking. They further subdivide those in remission into early or sustained, and partial or full. Some groups, most notably Alcoholics Anonymous, do not recognize remission. Instead, these groups use the term recovery to describe those who have completely stopped consumption of alcohol and are addressing underlying emotional and social factors.
Etymology
The term "alcoholism" was first used in 1849 by the physician Magnus Huss to describe the systematic adverse effects of alcohol. [3]
In the United States, use of the word "alcoholism" was largely popularized by the inception and growth of Alcoholics Anonymous in 1939. Although lacking a specific definition for alcoholism, AA's "Big Book" compares alcoholism to an allergy and an illness.[4]
A 1960 study by E. Morton Jellinek is considered the foundation of the modern disease theory of alcoholism.[5] Jellinek's definition restricted the use of the word "alcoholism" to those showing a particular natural history. The modern medical definition of alcoholism has been revised numerous times since then. The American Medical Association currently uses the word alcoholism to refer to a particular chronic primary disease. A minority within the medical field, notably Herbert Fingarette and Stanton Peele, argue against the existence of this disease. However, critics of the disease model acknowledge that the word "alcoholism" refers to a disease, and use the term "heavy drinking" when discussing the negative effects of alcohol consumption.
Epidemiology
Substance use disorders are a major public health problem facing many countries. "The most common substance of abuse/dependence in patients presenting for treatment is alcohol."[6] In the United Kingdom, the number of 'dependent drinkers' was calculated as over 2.8 million in 2001.[7] The World Health Organization estimates that about 140 million people throughout the world suffer from alcohol dependence.[8][9]
Within the medical community, there is broad consensus regarding alcoholism as a disease state. Outside the medical community, there is considerable debate regarding the Disease Theory of Alcoholism. Proponents argue that any structural or functional disorder having a predictable course, or progression, should be classified as a disease. Opponents cite the inability to pin down the behavioral issues to a physical cause as a reason for avoiding classification.
A 2002 study by the National Institute on Alcohol Abuse and Alcoholism surveyed a group of 4,422 adult alcoholics and found that after one year some were no longer alcoholics, even though only 25.5% of the group received any treatment,[10] with the breakdown as follows:
- 25% still dependent
- 27.3% in partial remission (some symptoms persist)
- 11.8% asymptomatic drinkers (consumption increases chances of relapse)
- 35.9% fully recovered — made up of 17.7% low-risk drinkers plus 18.2% abstainers.
Identification and diagnosis
Multiple tools are available to those wishing to conduct screening for alcoholism. Identification of alcoholism may be difficult because there is no detectable physiologic difference between a person who drinks frequently and a person with the condition. Identification involves an objective assessment regarding the damage that imbibing alcohol does to the drinker's life compared to the subjective benefits the drinker perceives from consuming alcohol. While there are many cases where an alcoholic's life has been significantly and obviously damaged, there are always borderline cases that can be difficult to classify.
Addiction Medicine specialists have extensive training with respect to diagnosing and treating patients with alcoholism.
Screening
Several tools may be used to detect a loss of control of alcohol use. These tools are mostly self reports in questionnaire form. Another common theme is a score or tally that sums up the general severity of alcohol use.
- The CAGE questionnaire, named for its four questions, is one such example that may be used to screen patients quickly in a doctor's office.
Two "yes" responses indicate that the respondent should be investigated further.
The questionnaire asks the following questions:
- The CAGE questionnaire, among others, has been extensively validated for use in identifying alcoholism. It is not valid for diagnosis of other substance use disorders, although somewhat modified versions of the CAGE are frequently implemented for such a purpose.
- The Alcohol Dependence Data Questionnaire is a more sensitive diagnostic test than the CAGE test.[13] It helps distinguish a diagnosis of alcohol dependence from one of heavy alcohol use.
- The Michigan Alcohol Screening Test (MAST) is a screening tool for alcoholism widely used by courts to determine the appropriate sentencing for people convicted of alcohol-related offenses,[14] driving under the influence being the most common.
- The Alcohol Use Disorders Identification Test (AUDIT) is a screening questionnaire developed by the World Health Organization. This test is unique in that it has been validated in six countries and is used internationally.[15] Like the CAGE questionnaire, it uses a simple set of questions - a high score earning a deeper investigation.
- The Paddington Alcohol Test (PAT) was designed to screen for alcohol related problems amongst those attending Accident and Emergency departments. It concords well with the AUDIT questionnaire but is administered in a fifth of the time.[16]
Genetic predisposition testing
Psychiatric geneticists John I. Nurnberger, Jr., and Laura Jean Bierut suggest that alcoholism does not have a single cause—including genetic—but that genes do play an important role "by affecting processes in the body and brain that interact with one another and with an individual's life experiences to produce protection or susceptibility." They also report that less than a dozen alcoholism-related genes have been identified, but that more likely await discovery.[17]
At least one genetic test exists for an allele that is correlated to alcoholism and opiate addiction.[18] Human dopamine receptor genes have a detectable variation referred to as the DRD2 TaqI polymorphism. Those who possess the A1 allele (variation) of this polymorphism have a small but significant tendency towards addiction to opiates and endorphin releasing drugs like alcohol.[19] Although this allele is slightly more common in alcoholics and opiate addicts, it is not by itself an adequate predictor of alcoholism, and some researchers argue that evidence for DRD2 is contradictory.[17]
DSM diagnosis
The DSM-IV diagnosis of alcohol dependence represents one approach to the definition of alcoholism. In part this is to assist in the development of research protocols in which findings can be compared with one another. According to the DSM-IV, an alcohol dependence diagnosis is:
...maladaptive alcohol use with clinically significant impairment as manifested by at least three of the following within any one-year period: tolerance; withdrawal; taken in greater amounts or over longer time course than intended; desire or unsuccessful attempts to cut down or control use; great deal of time spent obtaining, using, or recovering from use; social, occupational, or recreational activities given up or reduced; continued use despite knowledge of physical or psychological sequelae.
Urine and blood tests
There are reliable tests for the actual use of alcohol, one common test being that of blood alcohol content (BAC). These tests do not differentiate alcoholics from non-alcoholics; however, long-term heavy drinking does have a few recognizable effects on the body, including:
- Macrocytosis (enlarged MCV)1
- Elevated GGT²
- Moderate elevation of AST and ALT and an AST:ALT ratio of 2:1.
- High carbohydrate deficient transferrin (CDT)
However, none of these blood tests for biological markers are as sensitive as screening questionaires.
Effects
The primary effect of alcoholism is to encourage the sufferer to drink at times and in amounts that are damaging. The secondary damage caused by an inability to control one's drinking manifests in many ways.
It is common for a person suffering from alcoholism to drink well after physical health effects start to manifest. The physical health effects associated with alcohol consumption may include cirrhosis of the liver, pancreatitis, epilepsy, polyneuropathy, alcoholic dementia, heart disease, increased chance of cancer, nutritional deficiencies, sexual dysfunction, and death from many sources.
Social effects
The social problems arising from alcoholism can be significant. Being drunk or hung over during work hours can result in loss of employment, which can lead to financial problems including the loss of living quarters. Drinking at inappropriate times, and behavior caused by reduced judgment, can lead to legal consequences, such as criminal charges for drunk driving or public disorder, or civil penalties for tortious behavior. An alcoholic's behavior and mental impairment while drunk can profoundly impact surrounding family and friends, possibly leading to marital conflict and divorce, or contributing to domestic violence. This can contribute to lasting damage to the emotional development of the alcoholic's children, even after they reach adulthood. The alcoholic could suffer from loss of respect from others who may see the problem as self-inflicted and easily avoided.
Alcohol withdrawal
Alcohol withdrawal differs significantly from most other drugs because it can be directly fatal. While it is possible for heroin addicts, for instance, to die from other health problems made worse by the strain of withdrawal, an otherwise healthy alcoholic can die from the direct effects of withdrawal if it is not properly managed. Heavy consumption of alcohol reduces the production of GABA, which is a neuroinhibitor. An abrupt stop of alcohol consumption can induce a condition where neither alcohol nor GABA exists in the system in adequate quantities, causing uncontrolled firing of the synapses. This manifests as hallucinations, shakes, convulsions, seizures, and possible heart failure, all of which are collectively referred to as delirium tremens. All of these withdrawal issues can be safely controlled with a medically supervised detoxification program.
Treatments
Treatments for alcoholism are quite varied because there are multiple perspectives for the condition itself. Those who approach alcoholism as a medical condition or disease recommend differing treatments than, for instance, those who approach the condition as one of social choice.
Most treatments focus on helping people discontinue their alcohol intake, followed up with life training and/or social support in order to help them resist a return to alcohol use. Since alcoholism involves multiple factors which encourage a person to continue drinking, they must all be addressed in order to successfully prevent a relapse. An example of this kind of treatment is detoxification followed by a combination of supportive therapy, attendance at self-help groups, and ongoing development of coping mechanisms. The treatment community for alcoholism typically supports an abstinence-based zero tolerance approach; however, there are some who promote a harm-reduction approach as well.[6]
Effectiveness
The effectiveness of alcoholism treatments varies widely. When considering the effectiveness of treatment options, one must consider the success rate based on those who enter a program, not just those who complete it. Since completion of a program is the qualification for success, success among those who complete a program is generally near 100%. It is also important to consider not just the rate of those reaching treatment goals but the rate of those relapsing. Results should also be compared to the roughly 5% rate at which people will quit on their own.[20] A year after completing a rehab program, about a third of alcoholics are sober, an additional 40 percent are substantially improved but still drink heavily on occasion, and a quarter have completely relapsed.[21]
Detoxification
Alcohol detoxification or 'detox' for alcoholics is an abrupt stop of alcohol drinking coupled with the substitution of drugs that have similar effects to prevent alcohol withdrawal.
Detoxification treats the physical effects of prolonged use of alcohol, but does not actually treat alcoholism. After detox is complete, relapse is likely without further treatment. These rehabilitations (or 'rehabs') may take place in an inpatient or outpatient setting.
Group therapy and psychotherapy
After detoxification, various forms of group therapy or psychotherapy can be used to deal with underlying psychological issues that are related to alcohol addiction, as well as provide relapse prevention skills.
The mutual-help group-counseling approach is one of the most common ways of helping alcoholics maintain sobriety. Many organizations have been formed to provide this service. Alcoholics Anonymous was the first group, and has more adherents than all other programs combined. Some of the others include LifeRing Secular Recovery, Rational Recovery, SMART Recovery, and Women For Sobriety.
Rationing and moderation
Rationing and moderation programs such as Moderation Management and The HAMS Harm Reduction Network do not mandate complete abstinence. While most alcoholics are unable to limit their drinking in this way, some return to moderate drinking. A 2002 U.S. study by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) showed that 17.7% of individuals diagnosed as alcohol dependent more than one year prior returned to low-risk drinking. However, this group showed fewer initial symptoms of dependency.[22] A follow-up study, using the same NESARC subjects that were judged to be in remission in 2001-2002, examined the rates of return to problem drinking in 2004-2005. The major conclusion made by the authors of this NIAAA study was "Abstinence represents the most stable form of remission for most recovering alcoholics". [23]
Medications
A variety of medications may be prescribed as part of treatment for alcoholism.
- Antabuse (disulfiram) prevents the elimination of acetaldehyde, a chemical the body produces when breaking down ethanol. Acetaldehyde itself is the cause of many hangover symptoms from alcohol use. The overall effect is severe discomfort when alcohol is ingested: an extremely fast-acting and long-lasting uncomfortable hangover. This discourages an alcoholic from drinking in significant amounts while they take the medicine. A recent 9-year study found that incorporation of supervised disulfiram and a related compound carbamide into a comprehensive treatment program resulted in an abstinence rate of over 50%. [24]
- Naltrexone is a competitive antagonist for opioid receptors, effectively blocking our ability to use endorphins and opiates. Naltrexone is used in two very different forms of treatment. The first treatment uses naltrexone to decrease cravings for alcohol and encourage abstinence. The other treatment, called pharmacological extinction, combines naltrexone with normal drinking habits in order to reverse the endorphin conditioning that causes alcohol addiction.
Naltrexone comes in two forms. Oral naltrexone, originally but no longer available as the brand ReVia, is a pill form and must be taken daily to be effective. Vivitrol is a time-release formulation that is injected in the buttocks once a month.
- Acamprosate (also known as Campral) is thought to stabilize the chemical balance of the brain that would otherwise be disrupted by alcoholism. The Food and Drug Administration (FDA) approved this drug in 2004, saying "While its mechanism of action is not fully understood, Campral is thought to act on the brain pathways related to alcohol abuse...Campral proved superior to placebo in maintaining abstinence for a short period of time..."[25] While effective alone, it is often paired with other medication treatments like naltrexone with great success.[26][27] Acamprosate reduces glutamate release. The COMBINE study was unable to demonstrate efficacy for Acamprosate.[28]
- Topiramate (brand name Topamax), a derivative of the naturally occurring sugar monosaccharide D-fructose, has been found effective in helping alcoholics quit or cut back on the amount they drink. In one study heavy drinkers were six times more likely to remain abstinent for a month if they took the medication, even in small doses.[29] In another study, those who received topiramate had fewer heavy drinking days, fewer drinks per day and more days of continuous abstinence than those who received the placebo.[30] Topiramate works by reducing dopamine so that drinkers no longer get any pleasure from consuming alcohol and is the only medication shown to be effective for persons who are still drinking.
Societal impact
The various health problems associated with long-term alcohol consumption are generally perceived as detrimental to society, for example, money due to lost labor-hours, medical costs, and secondary treatment costs. Alcohol use is a major contributing factor for head injuries, motor vehicle accidents, violence, and assaults. Beyond money, there is also the pain and suffering of the all individuals besides the alcoholic affected. For instance, alcohol consumption by a pregnant woman can lead to Fetal alcohol syndrome,[31] an incurable and damaging condition.[32]
Estimates of the economic costs of alcohol abuse, collected by the World Health Organization, vary from one to six per cent of a country's GDP.[33] One Australian estimate pegged alcohol's social costs at 24 per cent of all drug abuse costs; a similar Canadian study concluded alcohol's share was 41 per cent.[34]
A study quantified the cost to the UK of all forms of alcohol misuse as £18.5–20 billion annually (2001 figures).[35][7]
Stereotypes
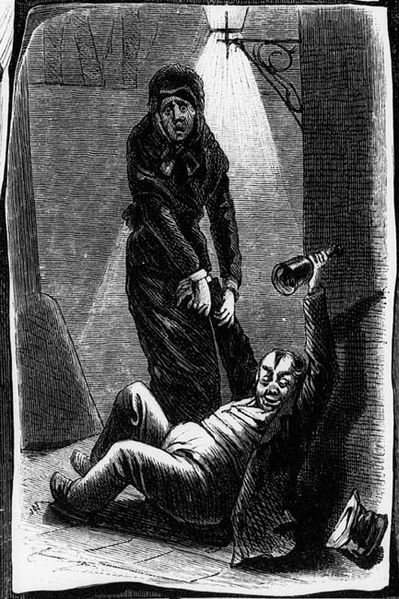
Stereotypes of alcoholics are often found in fiction and popular culture. The 'town drunk' is a stock character in Western popular culture.
Stereotypes of drunkenness may be based on racism, as in the depiction of the Irish as heavy drinkers.[36][37] In Australia and Canada, Aboriginal people have similarly been stereotyped as alcoholics.
Politics and public health
Because alcohol use disorders are perceived as impacting society as a whole, governments and parliaments have formed alcohol policies in order to reduce the harm of alcoholism. The World Health Organization, the European Union and other regional bodies are working on alcohol action plans and programs.
See also
- Adult Children of Alcoholics
- Alcohol consumption and health
- Alcohol tolerance
- Drunkenness
- Substance abuse
- Wernicke-Korsakoff syndrome
- Medical diagnostics to test for alcohol use
References
- ↑ The definition of alcoholism, The Joint Committee of the National Council on Alcoholism and Drug Dependence and the American Society of Addiction Medicine to Study the Definition and Criteria for the Diagnosis of Alcoholism, The Journal of the American Medical Association, 268(8), August 26, 1992
- ↑ 2.0 2.1 2.2 APA Dictionary of Psychology, 1st ed., Gary R. VandenBos, ed., Washington: American Psychological Association, 2007
- ↑ Template:Citeweb
- ↑ Template:Citeweb
- ↑ Template:Citeweb
- ↑ 6.0 6.1 Gabbard: "Treatments of Psychiatric Disorders". Published by the American Psychiatric Association: 3rd edition, 2001, ISBN 0-88048-910-3
- ↑ 7.0 7.1 Cabinet Office Strategy Unit Alcohol misuse: How much does it cost? September 2003
- ↑ WHO European Ministerial Conference on Young People and Alcohol
- ↑ WHO to meet beverage company representatives to discuss health-related alcohol issues
- ↑ National Institute on Alcohol Abuse and Alcoholism 2001-2002 Survey Finds That Many Recover From Alcoholism Press release 18 January 2005.
- ↑ Ewing, John A. “Detecting Alcoholism: The CAGE Questionnaire” JAMA 252: 1905-1907, 1984
- ↑ CAGE Questionnaire (PDF)
- ↑ Alcohol Dependence Data Questionnaire (SADD)
- ↑ Michigan Alcohol Screening Test (MAST)
- ↑ AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care
- ↑ Smith, SG (Sep 1996). "Detection of alcohol misusing patients in accident and emergency departments: the Paddington alcohol test (PAT)". Journal of Accident and Emergency Medicine. British Association for Accident and Emergency Medicine. 13 (5): 308–312. Retrieved 2006-11-19. Unknown parameter
|coauthors=ignored (help) - ↑ 17.0 17.1 Nurnberger, Jr., John I., and Bierut, Laura Jean. "Seeking the Connections: Alcoholism and our Genes." Scientific American, Apr2007, Vol. 296, Issue 4.
- ↑ New York Daily News (William Sherman) Test targets addiction gene 11 February 2006
- ↑ Ulf Berggren, Claudia Fahlke, Erik Aronsson, Aikaterini Karanti, Matts Eriksson, Kaj Blennow, Dag Thelle, Henrik Zetterberg and Jan Balldin The TaqIA DRD2 A1 Allele Is Associated with Alcohol-Dependence although its Effect Size Is Small Alcohol and Alcoholism 2006 41(5):479-485; doi:10.1093/alcalc/agl043
- ↑ Spontaneous Recovery in Alcoholics: A Review and Analysis of the Available Research, by R. G. Smart Drug and Alcohol Dependence, Vol. 1, 1975-1976, p. 284.
- ↑ Based on information from Dr. Mark Willenbring of the National Institute on Alcohol Abuse and Alcoholism, the February 2007 issue of Newsweek - Adler, Jerry; Underwood, Anne; Kelley, Raina; Springen, Karen; Breslau, Karen. "Rehab Reality Check" Newsweek, 2/19/2007, Vol. 149 Issue 8, p44-46, 3p, 4c
- ↑ Dawson DA, Grant BF, Stinson FS, Chou PS, Huang B, Ruan WJ. 2005. Recovery from DSM-IV alcohol dependence: United States, 2001-2002. : Addiction. Mar;100(3):281-92
- ↑ Dawson DA, Goldstein RB, Grant BF. 2007. Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: a 3-year follow-up. Alcohol Clin Exp Res. 2007 Dec;31(12):2036-45.
- ↑ Krampe, H., Stawicki, S., Wagner, T., Bartels, C., Aust, C., Ru¨ ther, E., Poser, W., and Ehrenreich, H. 2006. Follow-up of 180 Alcoholic Patients for up to 7 Years After Outpatient Treatment: Impact of Alcohol Deterrents on Outcome. Alcohol Clin Exp Res,30(1):86-95.
- ↑ "FDA Approves New Drug for Treatment of Alcoholism". Retrieved 2006-04-02."
- ↑ "Effect of oral acamprosate on abstinence in patients with alcohol dependence in a double-blind, placebo-controlled trial: The role of patient motivation". 2006-03-17. Retrieved 2006-04-10.
- ↑ "COMBINED ACAMPROSATE AND NALTREXONE, WITH COGNITIVE BEHAVIOURAL THERAPY IS SUPERIOR TO EITHER MEDICATION ALONE FOR ALCOHOL ABSTINENCE: A SINGLE CENTRES' EXPERIENCE WITH PHARMACOTHERAPY". 2006-02-08. Retrieved 2006-04-10.
- ↑ "Naltrexone or Specialized Alcohol Counseling an Effective Treatment for Alcohol Dependence When Delivered with Medical Management". 2006-05-02.
- ↑ Johnson, Bankole A., et al. Oral topiramate for treatment of alcohol dependence: a randomised controlled trial. The Lancet, 2003, 361(9370), 1677-1685: Swift, B. Topiramate for the treatment of alcohol dependence: initiating abstinence. The Lancet, 2003, 361(9370), 1666-1667
- ↑ Johnson, Bankole A., et al. Topiramate for Treating Alcohol Dependence - A Randomized Controlled Trial. Journal of the American Medical Association, 2007 (October), 298(14), 1641-1651
- ↑ CDC. (2004). Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. Can be downloaded at http://www.cdc.gov/fas/faspub.htm
- ↑ Streissguth, A. (1997). Fetal Alcohol Syndrome: A Guide for Families and Communities. Baltimore: Brookes Publishing. ISBN 1-55766-283-5.
- ↑ "Global Status Report on Alcohol 2004" (PDF). World Health Organization. Retrieved 2007-01-03.
- ↑ "Economic cost of alcohol consumption". World Health Organization Global Alcohol Database. Retrieved 2007-01-03.
- ↑ "Q&A: The costs of alcohol". BBC. 19 September 2003.
- ↑ "World/Global Alcohol/Drink Consumption 2007".
- ↑ "The World's Drunks: The Irish".
Further reading
- Berry, Ralph E.; Boland James P. The Economic Cost of Alcohol Abuse The Free Press, New York, 1977 ISBN 0-02-903080-3
- Royce, James E. and Scratchley, David Alcoholism and Other Drug Problems Free Press, March 1996 ISBN-10: 0-684-82314-4 ISBN-13: 978-0-684-82314-0
- Valliant, George E., The Natural History of Alcoholism Revisited, Harvard University Press, May 1995 ISBN-10: 0-674-60378-8 ISBN-13: 978-0-674-60378-3
- Pence, Gregory, "Kant on Whether Alcoholism is a Disease," Ch. 2, The Elements of Bioethics, McGraw-Hill Books, 2007 ISBN-10: 0-073-13277-2.
- Milam, Dr. James R. and Ketcham, Katherine Under The Influence: A Guide to the Myths and Realities of Alcoholism. Bantam, 1983, ISBN 0-553-27487-2
- Warren Thompson, MD, FACP. “Alcoholism.” Emedicine.com, June 6, 2007. Retrieved 2007-09-02.
- Etiology and Natural History of Alcoholism. National Institute on Alcohol Abuse and Alcoholism.
Template:Link FA Template:Link FA
ar:إدمان كحولي zh-min-nan:Chiú-cheng tiòng-to̍k bs:Alkoholizam bg:Алкохолизъм ca:Alcoholisme cs:Alkoholismus cy:Alcoholiaeth da:Alkoholisme de:Alkoholkrankheit et:Alkoholism eo:Alkoholismo eu:Alkoholismo fa:الکلیسم gl:Alcoholismo hr:Alkoholizam id:Alkoholisme is:Alkóhólismi it:Alcolismo he:אלכוהוליזם jv:Alkoholisme lt:Alkoholizmas mk:Алкохолизам mt:Alkoħoliżmu ms:Alkoholisme nl:Alcoholisme no:Alkoholisme nn:Alkoholmisbruk oc:Alcolisme simple:Alcoholism sk:Alkoholizmus sl:Alkoholizem sr:Алкохолизам sh:Alkoholizam fi:Alkoholismi sv:Alkoholism tl:Alkoholismo tg:Алкоголизм uk:Алкоголізм yi:אלקאהאליזם