Adrenal hemorrhage: Difference between revisions
No edit summary |
|||
| Line 91: | Line 91: | ||
*Color Doppler and power Doppler imaging allow confirmation of the avascular nature of the mass. | *Color Doppler and power Doppler imaging allow confirmation of the avascular nature of the mass. | ||
[http://www.radswiki.net Images courtesy of RadsWiki] | |||
<gallery> | <gallery> | ||
Revision as of 23:51, 24 January 2009
| Adrenal hemorrhage | |
 | |
|---|---|
| Ultrasonography: Adrenal hemorrhage | |
| ICD-10 | A39.1, E35.1 |
| ICD-9 | 036.3 |
| DiseasesDB | 29316 |
| eMedicine | med/3009 |
| MeSH | D014884 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Phone:617-632-7753
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Adrenal hemorrhage or Waterhouse-Friderichsen syndrome (WFS) is massive, usually bilateral, hemorrhage into the adrenal glands caused by fulminant meningococcemia.[1] WFS is characterised by overwhelming bacterial infection, rapidly progressive hypotension leading to shock, disseminated intravascular coagulation (DIC) with widespread purpura, particularly of the skin, and rapidly developing adrenocortical insufficiency associated with massive bilateral adrenal hemorrhage.
Epidemiology
Meningococcus is another term for the bacterial species Neisseria meningitidis, which causes the type of meningitis which usually underlies this syndrome. Meningococcal meningitis occurs most commonly in children and young adults, and can occur in epidemics. In the United States it is the cause of about 20% of meningitis cases. At one time it was common among military recruits, but administration of the preventive meningococcal vaccine has greatly reduced this number. Freshman college students living in dormitory housing who have not been vaccinated are another risk group.
WFS can also be caused by Streptococcus pneumoniae infections, a common bacterial pathogen typically associated with meningitis in the adult and elderly population.[1] Staphylococcus aureus has recently also been implicated in pediatric WFS.[2]
Routine vaccination against meningococcus is recommended for people who have poor splenic function (who, for example, have had their spleen removed or who have sickle-cell anemia which damages the spleen), or who have certain immune disorders, such as complement deficiency.[3]
Etiology
Adrenal hemorrhage occurs secondary to both traumatic conditions and atraumatic conditions. Atraumatic causes of adrenal hemorrhage include:
- Stress
- Hemorrhagic diathesis or coagulopathy
- Neonatal stress
- Underlying adrenal tumors
- Idiopathic disease
Historical
Waterhouse-Friderichsen syndrome is named after Rupert Waterhouse (1873–1958), an English physician, and Carl Friderichsen (1886–1979), a Danish pediatrician, who wrote papers on the syndrome, which had been previously described.[4][5]
Differential Diagnosis
- Adrenal adenoma
- Adrenal carcinoma
- Adrenal metastases
- Adrenal myelolipoma
- Genitourinary tuberculosis
- Neuroblastoma
Symptoms
Waterhouse-Friderichsen syndrome is the most severe form of meningococcal septicemia.
The onset of the illness is nonspecific with fever, rigors, vomiting and headache. Soon a rash appears; first macular, not much different from the rose spots of typhoid, and rapidly becoming petechial and purpuric with a dusky gray color. Hypotension is the rule and rapidly leads to septic shock. The cyanosis of extremities can be impressive and the patient is very prostrated or comatose. In this form of meningococcal disease, meningitis generally does not occur.
There is hypoglycemia with hyponatremia and hyperkalemia, and the Synachten test demonstrates the acute suprarenal failure. Leukocytosis need not to be extreme and in fact leukopenia may be seen and it is a very poor prognostic sign. CRP levels can be elevated or almost normal. Thrombocytopenia is sometimes extreme, with alteration in PT and PTT suggestive of DIC. Acidosis and acute renal failure can be seen as in any severe sepsis.
Meningococci can be readily cultured from blood or CSF, and can sometimes be seen in smears of cutaneous lesions.
Diagnosis
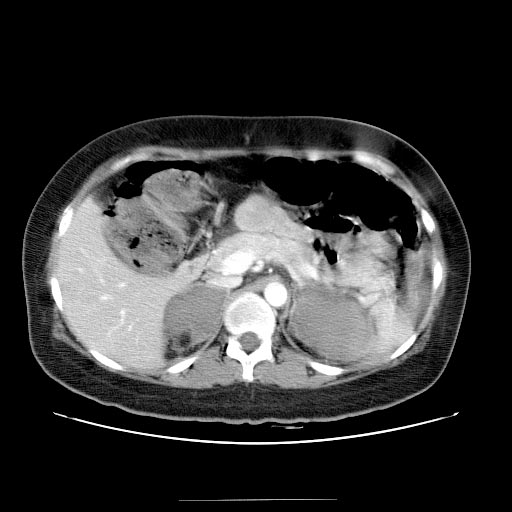
Computed Tomography
- Adenral hematomas characteristically appear round or oval
- Stranding of the periadrenal fat is evident as well.
- Attenuation value of adenal hematoma depends on its age.
- Acute to subacute hematomas contain areas of high attenuation that usually range from 50 to 90 HU.
- Adrenal hematomas decrease in size and attenuation over time, and most resolve completely.
- Adrenal hematoma may calcify after 1 year.
- Organized chronic adrenal hematoma appears as a mass with a hypoattenuating center with or without calcifications. Such masses are termed adrenal pseudocysts.
-
Computed Tomography: Bilateral adrenal hemorrhage
-
Computed Tomography: Bilateral adrenal hemorrhage
-
Computed Tomography: Follow up scan
-
Computed Tomography: Follow up scan
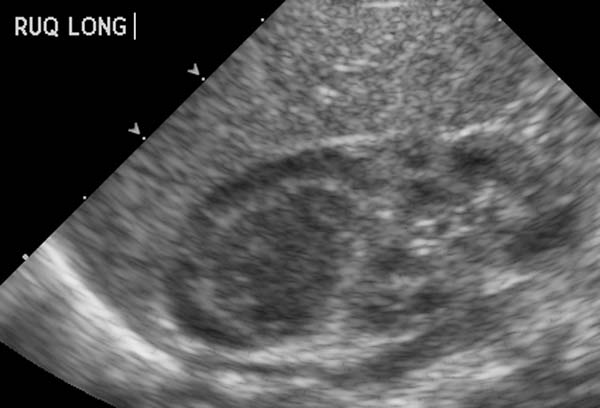
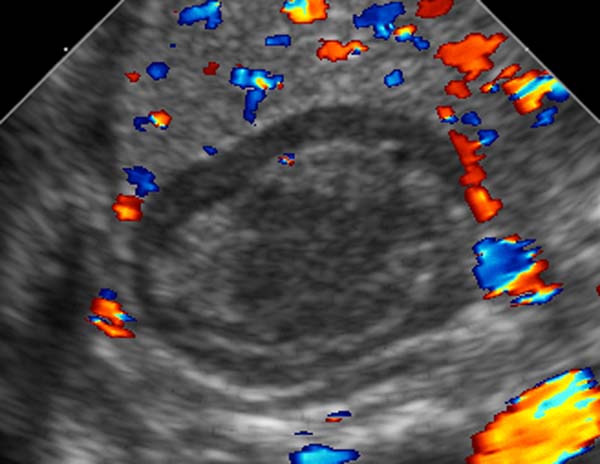
Ultrasonography
- Pattern of echogenicity of an adrenal hematoma depends on its age
- Early-stage hematoma appears solid with diffuse or inhomogeneous echogenicity.
- As liquefaction occurs, the mass demonstrates mixed echogenicity with a central hypoechoic region and eventually becomes completely anechoic and cystlike.
- Calcifications may be seen in the walls of the hematoma as early as 1–2 weeks after onset and gradually compact as the blood is absorbed.
- Color Doppler and power Doppler imaging allow confirmation of the avascular nature of the mass.
-
Ultrasonography: Adrenal hemorrhage
-
Ultrasonography: Adrenal hemorrhage
Magnetic Resonance Imaging
- Acute stage (less than 7 days after onset): the hematoma typically appears isointense or slightly hypointense on T1-weighted images and markedly hypointense on T2-weighted images.
- Subacute stage (7 days to 7 weeks after onset): the hematoma appears hyperintense on T1- and T2-weighted images.
- Chronic stage (which typically begins 7 weeks after onset): a hypointense rim is present on T1- and T2-weighted images, which is attributed to hemosiderin deposition and the presence of a fibrous capsule.
Treatment
Fulminant meningococcemia is a medical emergency and need to be treated with adequate antibiotics as fast as possible. Benzylpenicillin is the drug of choice with chloramphenicol as a good alternative in allergic patients. Hydrocortisone can sometimes reverse the hypoadrenal shock. Sometimes plastic surgery and grafting is needed to deal with tissue necrosis.
Ceftriaxone is an antibiotic commonly employed today.
References
- ↑ 1.0 1.1 Kumar V, Abbas A, Fausto N (2005). Robins and Coltran: Pathological Basis of Disease (7th ed.). Elsevier. pp. pp. 1214&ndash, 5. ISBN 978-0721601878.
- ↑ Adem P, Montgomery C, Husain A, Koogler T, Arangelovich V, Humilier M, Boyle-Vavra S, Daum R (2005). "Staphylococcus aureus sepsis and the Waterhouse-Friderichsen syndrome in children". N Engl J Med. 353 (12): 1245–51. PMID 16177250.
- ↑ Rosa D, Pasqualotto A, de Quadros M, Prezzi S (2004). "Deficiency of the eighth component of complement associated with recurrent meningococcal meningitis--case report and literature review". Braz J Infect Dis. 8 (4): 328–30. PMID 15565265.
- ↑ Waterhouse R (1911). "A case of suprarenal apoplexy". Lancet. 1: 577&ndash, 8. doi:10.1016/S0140-6736(01)60988-7.
- ↑ Friderichsen C (1918). "Nebennierenapoplexie bei kleinen Kindern". Jahrb Kinderheilk. 87: 109&ndash, 25.
External links
- Whonamedit.com page on the eponym
Acknowledgements
The content on this page was first contributed by: C. Michael Gibson, M.S., M.D.
Template:Bacterial diseases Template:SIB