Acute lymphoblastic leukemia pathophysiology
| https://https://www.youtube.com/watch?v=itkRVTqfPsE%7C350}} |
|
Acute lymphoblastic leukemia Microchapters |
|
Differentiating Acute lymphoblastic leukemia from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Acute lymphoblastic leukemia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Acute lymphoblastic leukemia pathophysiology |
|
Directions to Hospitals Treating Acute lymphoblastic leukemia |
|
Risk calculators and risk factors for Acute lymphoblastic leukemia pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2]Shivali Marketkar, M.B.B.S. [3] Carlos A Lopez, M.D. [4]
Overview
Acute lymphoid leukemia arises from lymphoblasts, which are hematologic white cells that are normally involved in the hematopoiesis. Chromosomal translocations involved in the pathogenesis of acute lymphoid leukemia include translocations between the chromosomes 9 and 22, t(9;22) (q34;q11.2) BCR-ABL1, translocations between the chromosomes 12 and 21, t(12;21)(p13;q22) TEL-AML1, translocations between the chromosomes 5 and 14, t(5;14)(q31;q32)IL3-IGH and translocations between chromosomes 1 and 19 t(1;19)(q23;p13.3) TCF3-PBX1.
Pathophysiology
Physiology
The normal physiology of acute lymphoblastic leukemia can be understood as follows:
- A lymphoblast is a remodeled naive lymphocyte with recasted cell morphology
- This happens when the lymphocyte is triggered by an antigen (from antigen-presenting cells) and enlarged in volume by nucleus and cytoplasmic growth as well as new mRNA and protein synthesis
- The lymphoblast then starts multiplying two to four times every 24-hours for 3-5 days, with a single lymphoblast producing approximately 1000 clones of its original naive lymphocyte, with each embodying the originally unique antigen specificity
- Finally the dividing cells transforms into effector cells, known as Plasma Cells (for B cells), Cytotoxic T cells, and Helper T cells.
Pathogenesis
- The cause of most acute lymphoblastic leukemia is not known
- In general, cancer is caused by damage to DNA that leads to uncontrolled cellular growth and spread throughout the body, either by increasing chemical signals that cause growth or interrupting chemical signals that control growth
- This damage may be caused by environmental factors such as:[1]
- chemicals
- drugs
- radiation
- In leukemias including acute lymphoblastic leukemia, chromosomal translocation occur regularly
- It is thought that most translocations occur before birth during fetal development
- These translocations may trigger oncogenes to "turn on", causing unregulated mitosis where cells divide too quickly and abnormally, resulting in leukemia.
- According with the World Health Organization (WHO) classification of acute lymphoblastic leukemia, B lymphoblastic leukemia/lymphoma with recurrent genetic abnormalities include:
- B lymphoblastic leukemia/lymphoma with t(9;22)(q34;q11.2), BCR-ABL1
- B lymphoblastic leukemia/lymphoma with t(v;11q23); MLL rearranged
- B lymphoblastic leukemia/lymphoma with t(12;21)(p13;q22) TEL-AML1 (ETV6-RUNX1)
- B lymphoblastic leukemia/lymphoma with hyperdiploidy
- B lymphoblastic leukemia/lymphoma with hypodiploidy
- B lymphoblastic leukemia/lymphoma with t(5;14)(q31;q32) IL3-IGH
- B lymphoblastic leukemia/lymphoma with t(1;19)(q23;p13.3) TCF3-PBX1
- According with the French-American-British (FAB) classification of acute lymphoblastic leukemia is divided into 3 subtypes:
- ALL-L1: small uniform cells
- ALL-L2: large varied cells
- ALL-L3: large varied cells with vacuoles (bubble-like features)
Malignant, immature white blood cells continuously multiply and are overproduced in the bone marrow. Acute lymphoblastic leukemia causes damage and death by crowding out normal cells in the bone marrow, and by spreading (metastasizing) to other organs.
Markers
B-cell acute lymphoblastic leukemia:[2]
T-cell acute lymphoblastic leukemia:
Genetics
Cytogenetics, the study of characteristic large changes in the chromosomes of cancer cells, has been increasingly recognized as an important predictor of outcome in acute lymphoblastic leukemia.[3]
It has been recognized for many years that some patients presenting with acute leukemia may have a cytogenetic abnormality that is cytogenetically indistinguishable from the Philadelphia chromosome (Ph1). This occurs in about 20% of adults and a small percentage of children with acute Lymphoblastic leukemia [2]
| Cytogenetic change | Risk category |
|---|---|
| Philadelphia chromosome | Poor prognosis |
| t(4;11)(q21;q23) | Poor prognosis |
| t(8;14)(q24.1;q32) | Poor prognosis |
| Complex karyotype (more than four abnormalities) | Poor prognosis |
| Low hypodiploidy or near triploidy | Poor prognosis |
| High hypodiploidy | Good prognosis |
| del(9p) | Good prognosis |
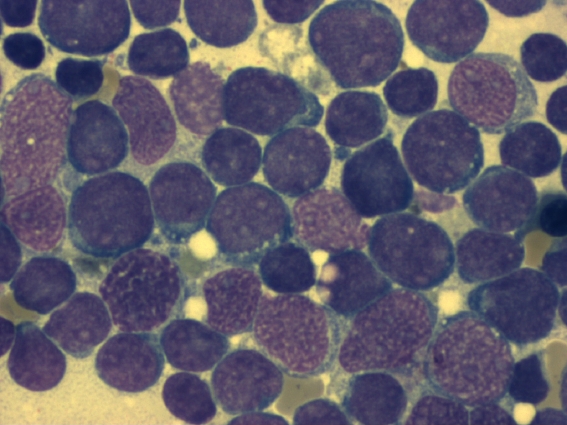
Gallery
References
- ↑ Inaba H, Greaves M, Mullighan CG (June 2013). "Acute lymphoblastic leukaemia". Lancet. 381 (9881): 1943–55. doi:10.1016/S0140-6736(12)62187-4. PMC 3816716. PMID 23523389.
- ↑ 2.0 2.1 "National Cancer Institute".
- ↑ Moorman A, Harrison C, Buck G, Richards S, Secker-Walker L, Martineau M, Vance G, Cherry A, Higgins R, Fielding A, Foroni L, Paietta E, Tallman M, Litzow M, Wiernik P, Rowe J, Goldstone A, Dewald G (2007). "Karyotype is an independent prognostic factor in adult acute lymphoblastic leukemia (ALL): analysis of cytogenetic data from patients treated on the Medical Research Council (MRC) UKALLXII/Eastern Cooperative Oncology Group (ECOG) 2993 trial". Blood. 109 (8): 3189–97. PMID 17170120.