Acute kidney injury laboratory findings: Difference between revisions
Farima Kahe (talk | contribs) |
|||
| Line 70: | Line 70: | ||
Another important index is the fractional excretion of urea (FE<sub>urea</sub>) calculated using the same equation for the fractional excretion of sodium. FE<sub>urea</sub> is of value in states of reduced effective circulating volume, and in cases where diuretics have been administered. In these situations, a low FEurea (<35%) has a higher sensitivity and specificity than FE<sub>Na</sub> in differentiating between prerenal azotemia and renal AKI.<ref name="pmid12427149">{{cite journal| author=Carvounis CP, Nisar S, Guro-Razuman S| title=Significance of the fractional excretion of urea in the differential diagnosis of acute renal failure. | journal=Kidney Int | year= 2002 | volume= 62 | issue= 6 | pages= 2223-9 | pmid=12427149 | doi=10.1046/j.1523-1755.2002.00683.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12427149 }} </ref> | Another important index is the fractional excretion of urea (FE<sub>urea</sub>) calculated using the same equation for the fractional excretion of sodium. FE<sub>urea</sub> is of value in states of reduced effective circulating volume, and in cases where diuretics have been administered. In these situations, a low FEurea (<35%) has a higher sensitivity and specificity than FE<sub>Na</sub> in differentiating between prerenal azotemia and renal AKI.<ref name="pmid12427149">{{cite journal| author=Carvounis CP, Nisar S, Guro-Razuman S| title=Significance of the fractional excretion of urea in the differential diagnosis of acute renal failure. | journal=Kidney Int | year= 2002 | volume= 62 | issue= 6 | pages= 2223-9 | pmid=12427149 | doi=10.1046/j.1523-1755.2002.00683.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12427149 }} </ref> | ||
{| | |||
{| | ! colspan="3" style="background:#4479BA; color: #FFFFFF;" align="center" + | Distinguishing Prerenal azotemia and ATN | ||
| | |||
|- | |- | ||
| | ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Parameter | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Prerenal AKI | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Acute Tubular Necrosis | |||
|- | |- | ||
| | | style="background:#DCDCDC;" align="center" + |'''Urinary sediment''' | ||
| style="background:#F5F5F5;" align="center" + | Normal/Hyaline casts | |||
| style="background:#F5F5F5;" align="center" + | Epithelial cell casts | |||
|- | |- | ||
| | | style="background:#DCDCDC;" align="center" + |'''Urine specific gravity''' | ||
| style="background:#F5F5F5;" align="center" + | >1.020 | |||
| style="background:#F5F5F5;" align="center" + | <1.020 | |||
|- | |- | ||
| | | style="background:#DCDCDC;" align="center" + |'''Urine sodium (mmol/L)''' | ||
| style="background:#F5F5F5;" align="center" + | <20 | |||
| style="background:#F5F5F5;" align="center" + | >40 | |||
|- | |- | ||
| | | style="background:#DCDCDC;" align="center" + |'''FE<sub>Na</sub>''' | ||
| style="background:#F5F5F5;" align="center" + | <1% | |||
| style="background:#F5F5F5;" align="center" + | >2% | |||
|- | |- | ||
| | | style="background:#DCDCDC;" align="center" + |'''FE<sub>urea</sub>''' | ||
| style="background:#F5F5F5;" align="center" + | <35% | |||
| style="background:#F5F5F5;" align="center" + | >50% | |||
|- | |- | ||
| | | style="background:#DCDCDC;" align="center" + |'''Urine osmolality (mOsmol/kg H<sub>2</sub>O)''' | ||
| style="background:#F5F5F5;" align="center" + | >500 | |||
| style="background:#F5F5F5;" align="center" + | <350 | |||
|- | |- | ||
| | | style="background:#DCDCDC;" align="center" + |'''Urine-Plasma creatinine ratio''' | ||
| style="background:#F5F5F5;" align="center" + | >40 | |||
| style="background:#F5F5F5;" align="center" + | <10 | |||
|- | |||
| style="background:#DCDCDC;" align="center" + |'''Plasma BUN-creatinine ratio''' | |||
| style="background:#F5F5F5;" align="center" + | >20 | |||
| style="background:#F5F5F5;" align="center" + | <15 | |||
|} | |} | ||
Revision as of 18:29, 2 July 2018
|
Acute kidney injury Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Acute kidney injury laboratory findings On the Web |
|
American Roentgen Ray Society Images of Acute kidney injury laboratory findings |
|
Risk calculators and risk factors for Acute kidney injury laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief:
Overview
An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name].
OR
Laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
OR
[Test] is usually normal for patients with [disease name].
OR
Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication].
OR
There are no diagnostic laboratory findings associated with [disease name].
Laboratory Findings
| Disease specific blood laboratory findings | |
|---|---|
| Blood Laboratory Finding | Related Etiologies |
| Severe hyperphosphatemia, hypocalcemia, elevated CPK and uric acid | Tumor Lysis Syndrome, Rhabdomyolysis |
| Increased anion gap and osmolal gap | Ethylene Glycol Poisoning |
| Low anion gap | Multiple Myeloma |
| Low complement levels and high titers of ANAs, ANCAs and cryoglobulins | Vasculitides |
| Severe anemia in the absence of bleeding | Hemolysis, Multiple Myeloma |
| Anemia, thrombocytopenia, schistocytes on peripheral blood smear, elevated LDH, and low haptoglobin | TTP, HUS, DIC |
| Peripheral eosinophilia | Acute interstitial nephritis, atheroembolic disease, polyarteritis nodosa, Churg-Strauss |
| Elevated BNP | Heart Failure |
| Bacteremia | Sepsis |
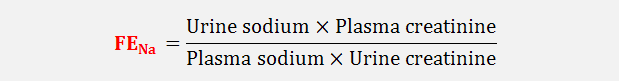
In prerenal azotemia, tubular function is preserved and sodium reabsorption increases with the associated renal vasoconstriction. Hence the FENa is usually <1% in prerenal azotemia. A high FENa in the context of prerenal azotemia is possible during diuretic treatment and glycosuria.
Another important index is the fractional excretion of urea (FEurea) calculated using the same equation for the fractional excretion of sodium. FEurea is of value in states of reduced effective circulating volume, and in cases where diuretics have been administered. In these situations, a low FEurea (<35%) has a higher sensitivity and specificity than FENa in differentiating between prerenal azotemia and renal AKI.[5]
| Distinguishing Prerenal azotemia and ATN | ||
|---|---|---|
| Parameter | Prerenal AKI | Acute Tubular Necrosis |
| Urinary sediment | Normal/Hyaline casts | Epithelial cell casts |
| Urine specific gravity | >1.020 | <1.020 |
| Urine sodium (mmol/L) | <20 | >40 |
| FENa | <1% | >2% |
| FEurea | <35% | >50% |
| Urine osmolality (mOsmol/kg H2O) | >500 | <350 |
| Urine-Plasma creatinine ratio | >40 | <10 |
| Plasma BUN-creatinine ratio | >20 | <15 |
References
- ↑ Combadière C, Raoul W, Guillonneau X, Sennlaub F (2013). "Comment on "Ccl2, Cx3cr1 and Ccl2/Cx3cr1 chemokine deficiencies are not sufficient to cause age-related retinal degeneration" by Luhmann et al. (Exp. Eye Res. 2013; 107: 80.doi: 10.1016)". Exp Eye Res. 111: 134–5. doi:10.1016/j.exer.2013.02.002. PMID 23402809.
- ↑ Schrier RW, Wang W, Poole B, Mitra A (2004). "Acute renal failure: definitions, diagnosis, pathogenesis, and therapy". J Clin Invest. 114 (1): 5–14. doi:10.1172/JCI22353. PMC 437979. PMID 15232604.
- ↑ Ostermann M, Joannidis M (September 2016). "Acute kidney injury 2016: diagnosis and diagnostic workup". Crit Care. 20 (1): 299. doi:10.1186/s13054-016-1478-z. PMC 5037640. PMID 27670788.
- ↑ Matheny ME, Peterson JF, Eden SK, Hung AM, Speroff T, Abdel-Kader K, Parr SK, Ikizler TA, Siew ED (2014). "Laboratory test surveillance following acute kidney injury". PLoS ONE. 9 (8): e103746. doi:10.1371/journal.pone.0103746. PMC 4130516. PMID 25117447.
- ↑ Carvounis CP, Nisar S, Guro-Razuman S (2002). "Significance of the fractional excretion of urea in the differential diagnosis of acute renal failure". Kidney Int. 62 (6): 2223–9. doi:10.1046/j.1523-1755.2002.00683.x. PMID 12427149.