Acne vulgaris medical therapy: Difference between revisions
Shanshan Cen (talk | contribs) No edit summary |
|||
| Line 10: | Line 10: | ||
Without restrained use of clinical lancing, it is harder for someone with serious acne to avoid causing damage to the [[dermis]], increased infection due to ruptured skin cells, and scarring. | Without restrained use of clinical lancing, it is harder for someone with serious acne to avoid causing damage to the [[dermis]], increased infection due to ruptured skin cells, and scarring. | ||
{| | * Acne vulgaris<ref>{{cite book | last = Gilbert | first = David | title = The Sanford guide to antimicrobial therapy | publisher = Antimicrobial Therapy | location = Sperryville, Va | year = 2015 | isbn = 978-1930808843 }}</ref> | ||
| | |||
| | |||
:* '''Earliest form, no inflammation''' | |||
::* Preferred regimen: [[Tretinoin]] (cream 0.025 or 0.05%) Topical qd {{or}} (gel 0.01 or 0.025%) qd | |||
::* Alternative regimen (1): [[Adapalene]] 0.1 % gel Topical qd | |||
::* Alternative regimen (2): [[Azelaic acid]] 20% cream Topical qd | |||
::* Alternative regimen (3): [[Tazarotene]] 0.1% cream Topical qd | |||
::* Note: Expect 40–70% decrease in comedones in 12 weeks | |||
:* '''Mild inflammation''' | |||
::* Preferred regimen: [[Erythromycin]] 3% Topical {{and}} [[Benzoyl peroxide]] 5% Topical bid | |||
::* Alternative regimen: [[Clindamycin]] 1% gel Topical bid {{and}} [[Benzoyl peroxide]] 5% Topical bid | |||
:* '''Moderate to severe inflammation''' | |||
::* Preferred regimen (1): [[Erythromycin]] 3% Topical {{and}} [[Benzoyl peroxide]] 5% bid {{withorwithout}} oral antibiotic | |||
::* Preferred regimen (2): [[Isotretinoin]] 0.1–1 mg/kg IV qd for 4–5 months for severe widespread nodular cystic lesions that fail oral antibiotic treatment | |||
::* Alternative regimen (1): [[Doxycycline]] 100 mg PO bid | |||
::* Alternative regimen (2):[[Minocycline]] 50 mg PO bid {{or}} [[Minocycline]] 1 mg/kg expensive extended release qd | |||
::* Note: Other alternatives include tetracycline, erythromycin, TMP-SMX, clindamycin | |||
===Other Treatments=== | ===Other Treatments=== | ||
Revision as of 15:42, 12 August 2015
|
Acne vulgaris Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Acne vulgaris medical therapy On the Web |
|
American Roentgen Ray Society Images of Acne vulgaris medical therapy |
|
Risk calculators and risk factors for Acne vulgaris medical therapy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Medical Therapy
Treatment ranges from knowledge of proper skin-care procedure to use of treatment products and diet control.
Acne Skincare
Proper clinical skincare of acne involves gentle hygiene and minimal and restrained interaction with pimples so that the skin (epidermis and dermis) is never bruised due to coarse crushing, which worsens infection and may lead to scarring. Clinical lancing with a sterilized needle evacuates matured pustules so that when they are pressed the fluids end up outside the dermis rather than further underneath. Without restrained use of clinical lancing, it is harder for someone with serious acne to avoid causing damage to the dermis, increased infection due to ruptured skin cells, and scarring.
- Acne vulgaris[1]
- Earliest form, no inflammation
- Preferred regimen: Tretinoin (cream 0.025 or 0.05%) Topical qd OR (gel 0.01 or 0.025%) qd
- Alternative regimen (1): Adapalene 0.1 % gel Topical qd
- Alternative regimen (2): Azelaic acid 20% cream Topical qd
- Alternative regimen (3): Tazarotene 0.1% cream Topical qd
- Note: Expect 40–70% decrease in comedones in 12 weeks
- Mild inflammation
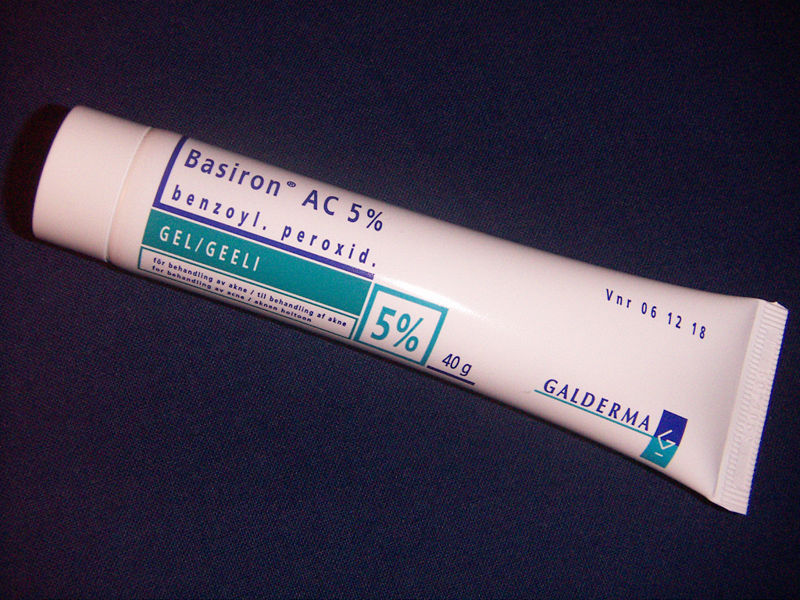
- Preferred regimen: Erythromycin 3% Topical AND Benzoyl peroxide 5% Topical bid
- Alternative regimen: Clindamycin 1% gel Topical bid AND Benzoyl peroxide 5% Topical bid
- Moderate to severe inflammation
- Preferred regimen (1): Erythromycin 3% Topical AND Benzoyl peroxide 5% bid ± oral antibiotic
- Preferred regimen (2): Isotretinoin 0.1–1 mg/kg IV qd for 4–5 months for severe widespread nodular cystic lesions that fail oral antibiotic treatment
- Alternative regimen (1): Doxycycline 100 mg PO bid
- Alternative regimen (2):Minocycline 50 mg PO bid OR Minocycline 1 mg/kg expensive extended release qd
- Note: Other alternatives include tetracycline, erythromycin, TMP-SMX, clindamycin
Other Treatments
- Oral contraceptives: May help in women; estrogen decreases androgens and thereby suppresses sebum secretion.
- Spironolactone: used off label to due to anti-androgen effect.
Available Treatment Products
There are many products sold for the treatment of acne, many of them without any scientifically-proven effects. Generally speaking successful treatments give little improvement within the first week or two; and then the acne decreases over approximately 3 months, after which the improvement starts to flatten out. Many treatments that promise big improvements within 2 weeks are likely to be largely disappointing. However short bursts of cortisone can give very quick results, and other treatments can rapidly improve some active spots, but not usually all active spots.
Modes of improvement are not necessarily fully understood but in general treatments are believed to work in at least 4 different ways (with many of the best treatments providing multiple simultaneous effects):
- Normalized shedding into the pore to prevent blockage
- Killing P. acnes
- Anti-inflammatory effects
- Hormonal manipulation
A combination of treatments can greatly reduce the amount and severity of acne in many cases. Those treatments that are most effective tend to have greater potential for side effects and need a greater degree of monitoring, so a step-wise approach is often taken. Many people consult with doctors when deciding which treatments to use, especially when considering using any treatments in combination. There are a number of treatments that have been proven effective:
Topical Bactericidals
Widely available OTC bactericidal products containing benzoyl peroxide may be used in mild to moderate acne. The gel or cream containing benzoyl peroxide is rubbed, twice daily, into the pores over the affected region. Bar soaps or washes may also be used and vary from 2 to 10% in strength. In addition to its therapeutic effect as a keratolytic (a chemical that dissolves the keratin plugging the pores) benzoyl peroxide also prevents new lesions by killing P.acnes. In one study, roughly 70% of participants using a 10% benzoyl peroxide solution experienced a reduction in acne lesions after 6 weeks.[2]Unlike antibiotics, benzoyl peroxide has the advantage of being a strong oxidizer (essentially a mild bleach) and thus does not appear to generate bacterial resistance. However, it routinely causes dryness, local irritation and redness. A sensible regimen may include the daily use of low-concentration (2.5%) benzoyl peroxide preparations, combined with suitable non-comedogenic moisturisers to help avoid overdrying the skin.[3]
Care must be taken when using benzoyl peroxide, as it can very easily bleach any fabric or hair it comes in contact with.
Other antibacterials that have been used include triclosan, or chlorhexidine gluconate but these are often less effective.
Prescription-strength benzoyl peroxide preparations do not necessarily differ with regard to the maximum concentration of the active ingredient (10%), but the drug is made available dissolved in a vehicle that more deeply penetrates the pores of the skin.
Topical Antibiotics
Externally applied antibiotics such as erythromycin, clindamycin, stiemycin, or tetracycline aim to kill the bacteria that are harbored in the blocked follicles. Whilst topical use of antibiotics is equally as effective as oral, this method avoids possible side effects of stomach upset or drug interactions (e.g. it will not affect the oral contraceptive pill), but may prove awkward to apply over larger areas than just the face alone.
Oral Antibiotics
Oral antibiotics used to treat acne include erythromycin or one of the tetracycline antibiotics (tetracycline, the better absorbed oxytetracycline, or one of the once daily doxycycline, minocycline or lymecycline). Trimethoprim is also sometimes used (off-label use in UK). However, reducing the P. acnes bacteria will not, in itself, do anything to reduce the oil secretion and abnormal cell behaviour that is the initial cause of the blocked follicles. Additionally the antibiotics are becoming less and less useful as resistant P. acnes are becoming more common. Acne will generally reappear quite soon after the end of treatment—days later in the case of topical applications, and weeks later in the case of oral antibiotics.
It has been found that sub-antimicrobial doses of antibiotics such as minocycline also improve acne. It is believed that minocycline's anti-inflammatory effect also prevents acne. These low doses do not kill bacteria and hence cannot induce resistance. Oral antibiotics such as Doxycycline have better results on the treatment of acne[4] and generally will work better if started with at a higher dose.
Hormonal Treatments
In females, acne can be improved with hormonal treatments. The common combined estrogen/progestogen methods of hormonal contraception have some effect, but the anti-testosterone, Cyproterone, in combination with an estrogen (Diane 35) is particularly effective at reducing androgenic hormone levels. Diane-35 is not available in the USA, but a newer oral contraceptive containing the progestin drospirenone is now available with fewer side effects than Diane 35 / Dianette. Both can be used where blood tests show abnormally high levels of androgens, but are effective even when this is not the case. Along with this, treatment with low dose spironolactone can have anti-androgenetic properties, especially in patients with polycystic ovarian syndrome.
If a pimple is large and/or does not seem to be affected by other treatments, a dermatologist may administer an injection of cortisone directly into it, which will usually reduce redness and inflammation almost immediately. This has the effect of flattening the pimple, thereby making it easier to cover up with makeup, and can also aid in the healing process. Side effects are minimal, but may include a temporary whitening of the skin around the injection point. This method also carries a much smaller risk of scarring than surgical removal.
Topical Retinoids
A group of medications for normalizing the follicle cell lifecycle are topical retinoids such as tretinoin (brand name Retin-A), adapalene (brand name Differin) and tazarotene (brand name Tazorac). Like isotretinoin, they are related to vitamin A, but they are administered as topicals and generally have much milder side effects. They can, however, cause significant irritation of the skin. The retinoids appear to influence the cell creation and death lifecycle of cells in the follicle lining. This helps prevent the hyperkeratinization of these cells that can create a blockage. Retinol, a form of vitamin A, has similar but milder effects and is used in many over-the-counter moisturizers and other topical products. Effective topical retinoids have been in use over 30 years but are available only on prescription so are not as widely used as the other topical treatments. Topical retinoids often cause an initial flare up of acne and facial flushing (physiology).
Oral Retinoids
A daily oral intake of vitamin A derivatives like isotretinoin (marketed as Accutane, Sotret, Claravis) over a period of 4-6 months can cause long-term resolution or reduction of acne by reducing the secretion of oils from the glands. It is believed that isotretinoin works primarily by reducing the secretion of oils from the glands, however some studies suggest that it affects other acne-related factors as well. Isotretinoin has been shown to be very effective in treating severe acne and can either improve or clear well over 80% of patients. The drug has a much longer effect than anti-bacterial treatments and will often cure acne for good. The treatment requires close medical supervision by a dermatologist because the drug has many known side effects (many of which can be severe). About 25% of patients may relapse after one treatment. In those cases, a second treatment for another 4-6 months may be indicated to obtain desired results. It is often recommended that one lets a few months pass between the two treatments, because the condition can actually improve somewhat in the time after stopping the treatment and waiting a few months also gives the body a chance to recover. Occasionally a third or even a fourth course is used, but the benefits are often less substantial. The most common side effects are dry skin and occasional nosebleeds (secondary to dry nasal mucosa). Oral retinoids also often cause an initial flare up of acne within a month or so, which can be severe. There are reports that the drug has damaged the liver of patients. For this reason, it is recommended that patients have blood samples taken and examined before and during treatment. In some cases, treatment is terminated due to elevated liver enzymes in the blood, which might be related to liver damage. Others claim that the reports of permanent damage to the liver are unsubstantiated, and routine testing is considered unnecessary by some dermatologists. Blood triglycerides also need to be monitored. However, routine testing are part of the official guidelines for the use of the drug in many countries. Some press reports suggest that isotretinoin may cause depression but as of September 2005 there is no agreement in the medical literature as to the risk. The drug also causes birth defects if women become pregnant while taking it or take it while pregnant. For this reason, female patients are required to use two separate forms of birth control or vow abstinence while on the drug. Because of this, the drug is supposed to be given to females as a last resort after milder treatments have proven insufficient. Restrictive rules (see iPledge Program) for use were put into force in the USA beginning in March 2006 to prevent misuse.[5] This has occasioned widespread editorial comment.[6]
Preferred Treatments by Types of Acne Vulgaris
- Comedonal (non-inflammatory) acne: local treatment with azelaic acid, salicylic acid, topical retinoids, benzoyl peroxide.
- Mild papulo-pustular (inflammatory) acne: benzoyl peroxide or topical retinoids, topical antibiotics (such as erythromycin).
- Moderate inflammatory acne: benzoyl peroxide or topical retinoids combined with oral antibiotics (tetracyclines). Isotretinoin is an option.
- Severe inflammatory acne, nodular acne, acne resistant to the above treatments: isotretinoin or contraceptive pills with cyproterone for females with virilization or drospirenone.
Antimicrobial Regimen
- Propiobacterium acnes [7]
- 1. Systemic infection
- Preferred regimen: Penicillin G 2 MU IV q4h for 2-4 weeks
- Alternative regimen (1): Clindamycin 600 mg IV q8h for 2-4 weeks
- Alternative regimen (2): Vancomycin 15 mg/kg IV q12h for 2-4 weeks
- 2. Shoulder prosthesis infection
- Preferred regimen: Amoxicillin AND Rifampin for 3-6 months
- 3. Acne vulgaris
- Topical antibiotics: Erythromycin OR Clindamycin
- Systemic antibiotics: Minocycline OR Doxycycline OR Trimethoprim-Sulfamethoxazole
References
- ↑ Gilbert, David (2015). The Sanford guide to antimicrobial therapy. Sperryville, Va: Antimicrobial Therapy. ISBN 978-1930808843.
- ↑ Comparative evaluation of retinoic acid, benzoyl peroxide and erythromycin lotion in acne vulgarils
- ↑ Kern, Daniel W. "Clear skin regimen: A free, step by step program." Acne.org. Instructions
- ↑ Thiboutot, D, (2000). "Prescription Medications for Treating Acne". Acne Net. 9 (7–8): 179–187. PMID 15636181.
- ↑ "The iPLEDGE Program - Guide to Best Practices for Isotretinoin - "The resource to help the prescriber prepare, plan treatments, and prevent pregnancies during the course of isotretinoin therapy"" (PDF). 2005.
- ↑ Bernadine Healy (2005-05-09). "Pledging for Accutane". US News Best Health. Check date values in:
|date=(help) - ↑ Bartlett, John (2012). Johns Hopkins ABX guide : diagnosis and treatment of infectious diseases. Burlington, MA: Jones and Bartlett Learning. ISBN 978-1449625580.