HIV AIDS natural history, complications, and prognosis
|
AIDS Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
HIV AIDS natural history, complications, and prognosis On the Web |
|
American Roentgen Ray Society Images of HIV AIDS natural history, complications, and prognosis |
|
FDA on HIV AIDS natural history, complications, and prognosis |
|
CDC on HIV AIDS natural history, complications, and prognosis |
|
HIV AIDS natural history, complications, and prognosis in the news |
|
Blogs on HIV AIDS natural history, complications, and prognosis |
|
Risk calculators and risk factors for HIV AIDS natural history, complications, and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Acquired immune deficiency syndrome (AIDS) is a collection of symptoms and infections resulting from the specific damage to the immune system caused by the human immunodeficiency virus (HIV) in humans,[1] and similar viruses in other species (SIV, FIV, etc.)
Natural History
Currently there is no cure for AIDS but taking treatment dramatically increased the amount of time people with HIV remain alive. Research continues in the areas of drug treatments and vaccine development. Unfortunately, HIV medications are not always available in the developing world, where the bulk of cases now occur.
Prognosis
Without treatment, the net median survival time after infection with HIV is estimated to be 9 to 11 years, depending on the HIV subtype, and the median survival rate after diagnosis of AIDS in resource-limited settings where treatment is not available ranges between 6 and 19 months, depending on the study.[2] In areas where it is widely available, the development of HAART as effective therapy for HIV infection and AIDS reduced the death rate from this disease by 80%, and raised the life expectancy for a newly-diagnosed HIV-infected person to about 20 years.[3]
Complications
HIV infection weakens patients immune system, making them highly susceptible to variety of infections and certain types of cancers.
1. Infections common to HIV/AIDS
- Tuberculosis (TB).
- Salmonellosis.
- Cytomegalovirus (CMV).
- Candidiasis.
- Cryptococcal meningitis.
- Toxoplasmosis.
- Cryptosporidiosis.
2. Cancers common to HIV/AIDS
- 2.A. Kaposi's sarcoma.
AIDS-associated Kaposi sarcoma presents with cutaneous lesions that begin as one or several red to purple-red macules, rapidly progressing to papules, nodules, and plaques, with a predilection for the head, neck, trunk, and mucous membranes.[4]
AIDS-associated Kaposi sarcoma simulated the greatest interest as one of the first illnesses associated with AIDS. Different from the classic form of Kaposi sarcoma, Tumors usually appear on the head, back, neck, muscular palate and the area of the gingiva.
In more advanced cases, they can be found in the stomach and intestines, the lymph nodes, and the lungs. KS-AIDS was first described in 1981 by three separate groups, most notably by Robert A. Schwartz and his collaborators at the University of Arizona.[5][6][7]
- 2.B. Lymphomas.
To read more about AIDS-related Lymphome, click here.
3. Other complications
- Wasting syndrome.
- Neurological complications.
Although HIV doesn't appear to invade the neuron, it can still cause neurological symptoms such as:
- Confusion
- Forgetfulness
- Depression
- Anxiety
One of the most common neurological complications in AIDS patient is AIDS dementia complex, to read more about it, click here
The strongest risk factor for excess mortality are:
- Viral load more than 400 copies/mL.
- CD4 count less than 200 cells/mL.
- Cytomegalovirus retinitis.
- Stigma associated with AIDS
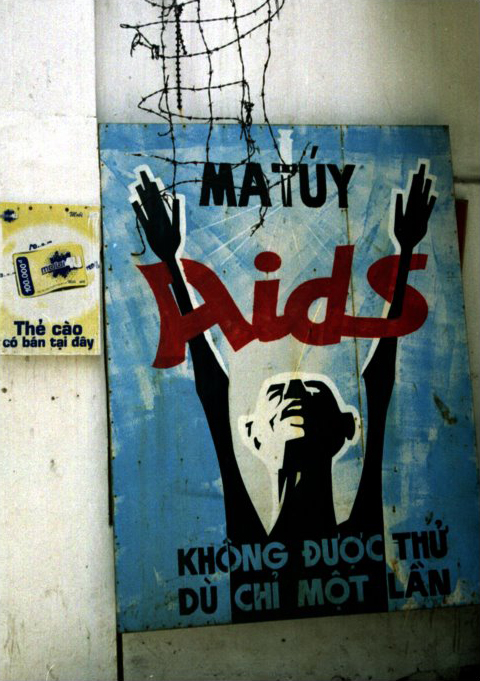
AIDS stigma exists around the world in a variety of ways, including ostracism, rejection, discrimination and avoidance of HIV infected people; compulsory HIV testing without prior consent or protection of confidentiality; violence against HIV infected individuals or people who are perceived to be infected with HIV; and the quarantine of HIV infected individuals.[8] Stigma-related violence or the fear of violence prevents many people from seeking HIV testing, returning for their results, or securing treatment, possibly turning what could be a manageable chronic illness into a death sentence and perpetuating the spread of HIV.[9]
AIDS stigma has been further divided into the following three categories:
- Instrumental AIDS stigma—a reflection of the fear and apprehension that are likely to be associated with any deadly and transmissible illness.[10]
- Symbolic AIDS stigma—the use of HIV/AIDS to express attitudes toward the social groups or lifestyles perceived to be associated with the disease.[10]
- Courtesy AIDS stigma—stigmatization of people connected to the issue of HIV/AIDS or HIV- positive people.[11]
Often, AIDS stigma is expressed in conjunction with one or more other stigmas, particularly those associated with homosexuality, bisexuality, promiscuity, and intravenous drug use.
In many developed countries, there is an association between AIDS and homosexuality or bisexuality, and this association is correlated with higher levels of sexual prejudice such as anti-homosexual attitudes.[12] There is also a perceived association between AIDS and all male-male sexual behavior, including sex between uninfected men.[10]
References
- ↑ "The Relationship Between the Human Immunodeficiency Virus and the Acquired Immunodeficiency Syndrome". NIAID. Retrieved 2008-03-10.
- ↑ Template:Cite paper
- ↑ Knoll B, Lassmann B, Temesgen Z (2007). "Current status of HIV infection: a review for non-HIV-treating physicians". Int J Dermatol. 46 (12): 1219–28. doi:10.1111/j.1365-4632.2007.03520.x. PMID 18173512.
- ↑ James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. ISBN 0-7216-2921-0.
- ↑ Schwartz, Robert A. (1994). "Kaposi's sarcoma presenting in a homosexual man — a new and striking phenomenon". Ariz Med. 38 (12): 902–4. Unknown parameter
|coauthors=ignored (help);|access-date=requires|url=(help) - ↑ Hausen, Harald Zur (2006). "Rhadinoviruses". Infections Causing Human Cancer. Weinheim: Wiley-VCH.
|access-date=requires|url=(help) - ↑ Drabell, Fredrick G (2006). "Kaposi's Sarcoma and Renal Diseases". New Topics in Cancer Research. New York: Nova Biomedical Books.
|access-date=requires|url=(help) - ↑ "The impact of AIDS on people and societies" (PDF). 2006 Report on the global AIDS epidemic (PDF)
|format=requires|url=(help). UNAIDS. 2006. Retrieved 2006-06-14. - ↑ Ogden J, Nyblade L (2005). "Common at its core: HIV-related stigma across contexts" (PDF). International Center for Research on Women. Retrieved 2007-02-15.
- ↑ 10.0 10.1 10.2 Herek GM, Capitanio JP (1999). "AIDS Stigma and sexual prejudice" (PDF). American Behavioral Scientist. 42 (7): 1130–1147. doi:10.1177/0002764299042007006. Retrieved 2006-03-27.
- ↑ Snyder M, Omoto AM, Crain AL (1999). "Punished for their good deeds: stigmatization for AIDS volunteers". American Behavioral Scientist. 42 (7): 1175&ndash, 1192. doi:10.1177/0002764299042007009.
- ↑ Herek GM, Capitanio JP, Widaman KF (2002). "HIV-related stigma and knowledge in the United States: prevalence and trends, 1991-1999" (PDF). Am J Public Health. 92 (3): 371–7. PMID 11867313. Retrieved 2008-03-10.