Iron deficiency anemia pathophysiology
|
Iron deficiency anemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Iron deficiency anemia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Iron deficiency anemia pathophysiology |
|
Risk calculators and risk factors for Iron deficiency anemia pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Shyam Patel [2]
Overview
Iron is needed for haemoglobin synthesis which is essential for oxygen transport in the body. Iron is stored as ferritin in the body and transported as transferrin. The source of iron is diet and recycling iron from reticuloendothelial cells. The absorption of iron is highly regulated by hepcidin. Loss of iron from the body, inadequate intake or increased hepcidin can lead to iron deficiency anemia.
Pathophysiology
Physiology
- Iron is needed for the synthesis of haemoglobin and new DNA. It is a major component of oxidation and reduction enzymes (cytochromes)[1]
- In the human body, iron mainly exists as bound to protein (hemoprotein), as heme compounds (hemoglobin or myoglobin), heme enzymes, or nonheme compounds (flavin-iron enzymes, transferrin, and ferritin).[2]
- The body requires iron for the synthesis of its oxygen transport proteins, (hemoglobin and myoglobin), and for the formation of heme enzymes and other iron-containing enzymes involved in electron transfer and oxidation-reductions.
- Human iron metabolism is controlled by various factors.
- 60% of the body iron is found in the hemoglobin present in circulating erythrocytes, 25% is contained in transferrin and ferritin, and the remaining 15% is bound to myoglobin in muscle tissue and in a variety of enzymes involved in the oxidative metabolism and many other cell functions.[3]
- Iron is bound and transported in the body via transferrin and stored in ferritin molecules.
- Iron is delivered to tissues by circulating transferrin, a transporter that captures iron released into the plasma from intestinal enterocytes or reticuloendothelial macrophages.[4]
- The binding of transferrin to the cell-surface transferrin receptor (TfR) 1 results in endocytosis and uptake of iron.
- Internalized iron is transported to mitochondria for the synthesis of heme or other iron containing enzymes.
- Excess iron is stored in cytosolic ferritin.
Absorption of iron
- Iron absorption occurs by the enterocytes in the duodenum and upper jejunum.[5][6][7]
- Dietary iron occurs in two forms: heme and non-heme. The primary sources of heme iron are hemoglobin and myoglobin from consumption of meat, poultry, and fish, whereas non-heme iron is obtained from cereals, pulses, legumes, fruits, and vegetables.[8]
- In the blood, it is transported by transferrin to the cells or the bone marrow for erythropoiesis.[9]
- Iron absorption is controlled by ferroportin on the basolateral surface of the cell. Ferroportin allows or does not allow iron from the mucosal cell into the plasma.
- Iron is absorbed in Fe+2 (ferric) state.
- The iron is consumed in Fe+3 (ferrous) state and is reduced to Fe+2 state by the acidic gastric pH by enzyme ferric reductase.[10]
- Fe+2 is absorbed by the enterocytes and exported across the basolateral membrane into the bloodstream via Fe+2 transporter ferroportin.
- The ferroportin-mediated efflux of Fe+2 is coupled by its reoxidation to Fe+3, catalyzed by ferroxidase hephaestin that interacts with ferroportin.[11]
- The total iron content of transferrin is dynamic and undergoes changes to sustain erythropoiesis.
- Senescent RBCs are cleared by reticuloendothelial macrophages, which metabolize hemoglobin and heme and release iron into the bloodstream.
- The transferrin iron pool is replenished by iron recycled from RBCs and by newly absorbed dietary iron.
- Macrophages export Fe+2 from their plasma membrane via ferroportin, in a process coupled by reoxidation of Fe+2 to Fe+3 by ceruloplasmin and followed by the loading of Fe+3 to transferrin.
Regulation of iron homeostasis
- Iron balance is mainly regulated at the point of absorption.[12]
- Hepcidin is a circulating peptide hormone secreted by the liver that plays a central role in the regulation of iron homeostasis. Inflammatory conditions lead to increased IL-6 production, which stimulates hepcidin production.
- This hormone is produced by hepatocytes and is a negative regulator of iron entry into plasma. Hepcidin acts by binding to ferroportin.[13][14][15]
- Binding of hepcidin induces ferroportin degradation.
- The loss of ferroportin from the cell surface prevents iron entry into plasma and decreased iron levels in the body.[16]
- Decreased expression of hepcidin leads to increased cell surface ferroportin and increased iron absorption.
- Plasma hepcidin levels are regulated by cytokines, plasma iron, anemia, and hypoxia.
- Overexpression of hepcidin leads to the anemia of chronic disease, while low hepcidin production results in hereditary hemochromatosis (HFE).
Storage
- Ferritin concentration together with that of hemosiderin reflects the body iron stores.[17][18][19][20][21][21]
- They store iron in an insoluble form and are present primarily in the liver, spleen, and bone marrow.
- Serum ferritin is the most convenient laboratory test to estimate iron stores.
Factors effecting iron absorption
- Factors that enhance iron uptake are:
- Factors inhibiting iron absorption are:
- Phytate (myo-inositol hexakisphosphate) is the main inhibitor of iron absorption[24][25][26].
- Calcium
- Animal proteins such as milk proteins, egg proteins, and albumin, have been shown to inhibit iron absorption.
- Proteins from soybean also decrease iron absorption.
- Suppresion of gastric acid such as use of antacids suprress iron absorption.
- Lead competes with iron for the absorption and blocks its absorption by competetive inhibition.
Iron requirement
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| Birth to 6 months | 0.27 mg* | 0.27 mg* | ||
| 7–12 months | 11 mg | 11 mg | ||
| 1–3 years | 7 mg | 7 mg | ||
| 4–8 years | 10 mg | 10 mg | ||
| 9–13 years | 8 mg | 8 mg | ||
| 14–18 years | 11 mg | 15 mg | 27 mg | 10 mg |
| 19–50 years | 8 mg | 18 mg | 27 mg | 9 mg |
| 51+ years | 8 mg | 8 mg |
Pathogenesis
- Iron deficiency anemia occurs when there is[27][28]:
- Low dietary intake
- Increased demands of iron
- Impaired absorption of iron
- Excessive loss of iron (blood loss)
- Increased hepcidin (chronic inflammation)
- Low dietary intake:
- Iron is obtained from foods such as:
- meat, such as lamb, pork, chicken, and beef
- beans
- pumpkin and squash seeds
- leafy greens, such as spinach
- raisins and other dried fruit
- eggs
- seafood, such as clams, sardines, shrimp, and oysters
- Iron-fortified dry and instant cereals Foods high in vitamin C include:
- Fruits such as oranges, grapefruits, strawberries, kiwis, guavas, papayas, pineapples, melons, and mangoes
- Red and green bell peppers
- Brussels sprouts
- Cauliflower
- Tomatoes
- Leafy greens
- Increased demands of iron
- Growth, the requirement of iron increases during the developmental period from infancy to adolescence and during adolescence.
- Pregnancy, during pregnancy the demand for iron is increased.
- Impaired absorption of iron:
- Malabsorption
- Deficiency of vitamin C in diet
- Excessive loss of iron (blood loss)
- The only means of excretion for iron is through blood loss
- Any source of external and internal bleeding can cause iron deficiency depending on the blood loss
- Increased hepcidin
- In chonric inflammatory conditions, the levels of hepcidin increase
- Increased hepcidin causes ferriportin degeneration and impaired iron absorption
- Iron is obtained from foods such as:
- Iron is required for haemoglobin synthesis, so deficiency of iron leads to depletion of haemoglobin
- Decrease in haemoglobin leads to anemia
- Due to low haemoglobin, oxygen is not tranported effectively to cells and results in hypoxia
| Population | Hb Diagnostic of anaemia (g/dL) |
|---|---|
| Children aged 6 months to 6 years old | <11.0 |
| Children aged 6-14 years old | <12.0 |
| Adult men | <13.0 |
| Adult non-pregnant women | <12.0 |
| Adult pregnant women | <11.0 |
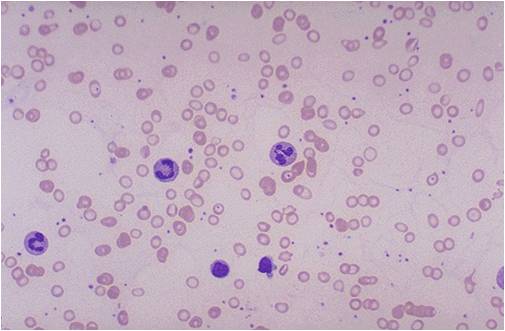
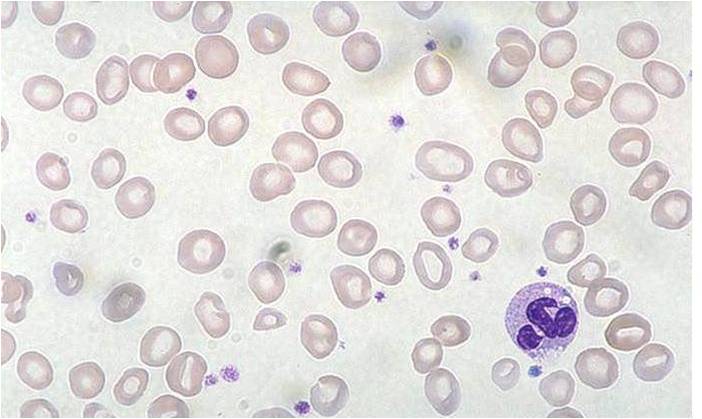
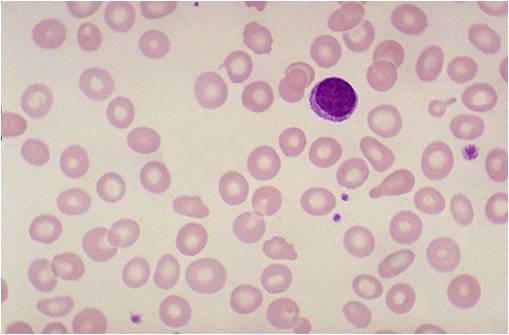
Histology
(Images shown below are courtesy of Melih Aktan MD, Istanbul Medical Faculty - Turkey)
-
Iron deficiency anemia
-
Iron deficiency anemia
-
Iron deficiency anemia
Video
{{#ev:youtube|7uDbu7esZik}}
External Link
Center for disease control and prevention
References
- ↑ Brissot P, Troadec MB, Loréal O, Brissot E (2018). "Pathophysiology and classification of iron overload diseases; update 2018". Transfus Clin Biol. doi:10.1016/j.tracli.2018.08.006. PMID 30173950.
- ↑ Murray-Kolb LE (2018). "Examining Consequence of Brain Iron Deficiency in the Absence of Anemia". J Nutr. doi:10.1093/jn/nxy186. PMID 30169646.
- ↑ Ghaffari S, Pourafkari L (2018). "Koilonychia in Iron-Deficiency Anemia". N Engl J Med. 379 (9): e13. doi:10.1056/NEJMicm1802104. PMID 30157401.
- ↑ Kassebaum NJ, Jasrasaria R, Naghavi M, Wulf SK, Johns N, Lozano R; et al. (2014). "A systematic analysis of global anemia burden from 1990 to 2010". Blood. 123 (5): 615–24. doi:10.1182/blood-2013-06-508325. PMC 3907750. PMID 24297872.
- ↑ Price EA, Mehra R, Holmes TH, Schrier SL (2011). "Anemia in older persons: etiology and evaluation". Blood Cells Mol Dis. 46 (2): 159–65. doi:10.1016/j.bcmd.2010.11.004. PMID 21208814.
- ↑ Mast AE, Bialkowski W, Bryant BJ, Wright DJ, Birch R, Kiss JE; et al. (2016). "A randomized, blinded, placebo-controlled trial of education and iron supplementation for mitigation of iron deficiency in regular blood donors". Transfusion. 56 (6 Pt 2): 1588–97. doi:10.1111/trf.13469. PMC 4905782. PMID 26813849.
- ↑ Shams S, Asheri H, Kianmehr A, Ziaee V, Koochakzadeh L, Monajemzadeh M; et al. (2010). "The prevalence of iron deficiency anaemia in female medical students in Tehran". Singapore Med J. 51 (2): 116–9. PMID 20358149.
- ↑ Fonseca C, Marques F, Robalo Nunes A, Belo A, Brilhante D, Cortez J (2016). "Prevalence of anaemia and iron deficiency in Portugal: the EMPIRE study". Intern Med J. 46 (4): 470–8. doi:10.1111/imj.13020. PMID 26841337.
- ↑ Cook JD, Skikne BS (1989). "Iron deficiency: definition and diagnosis". J Intern Med. 226 (5): 349–55. PMID 2681511.
- ↑ Annibale B, Capurso G, Chistolini A, D'Ambra G, DiGiulio E, Monarca B; et al. (2001). "Gastrointestinal causes of refractory iron deficiency anemia in patients without gastrointestinal symptoms". Am J Med. 111 (6): 439–45. PMID 11690568.
- ↑ Lopez A, Cacoub P, Macdougall IC, Peyrin-Biroulet L (2016). "Iron deficiency anaemia". Lancet. 387 (10021): 907–16. doi:10.1016/S0140-6736(15)60865-0. PMID 26314490.
- ↑ Khadem G, Scott IA, Klein K (2012). "Evaluation of iron deficiency anaemia in tertiary hospital settings: room for improvement?". Intern Med J. 42 (6): 658–64. doi:10.1111/j.1445-5994.2012.02724.x. PMID 22288902.
- ↑ Ioannou GN, Rockey DC, Bryson CL, Weiss NS (2002). "Iron deficiency and gastrointestinal malignancy: a population-based cohort study". Am J Med. 113 (4): 276–80. PMID 12361812. Review in: ACP J Club. 2003 May-Jun;138(3):80
- ↑ Unsworth DJ, Lock FJ, Harvey RF (1999). "Iron-deficiency anaemia in premenopausal women". Lancet. 353 (9158): 1100. PMID 10199377.
- ↑ Corazza GR, Valentini RA, Andreani ML, D'Anchino M, Leva MT, Ginaldi L; et al. (1995). "Subclinical coeliac disease is a frequent cause of iron-deficiency anaemia". Scand J Gastroenterol. 30 (2): 153–6. PMID 7732338.
- ↑ Unsworth DJ, Lock RJ, Harvey RF (2000). "Improving the diagnosis of coeliac disease in anaemic women". Br J Haematol. 111 (3): 898–901. PMID 11122153.
- ↑ Camaschella C (2015). "Iron deficiency: new insights into diagnosis and treatment". Hematology Am Soc Hematol Educ Program. 2015: 8–13. doi:10.1182/asheducation-2015.1.8. PMID 26637694.
- ↑ Hershko C, Hoffbrand AV, Keret D, Souroujon M, Maschler I, Monselise Y; et al. (2005). "Role of autoimmune gastritis, Helicobacter pylori and celiac disease in refractory or unexplained iron deficiency anemia". Haematologica. 90 (5): 585–95. PMID 15921373.
- ↑ Kalantar-Zadeh K, Höffken B, Wünsch H, Fink H, Kleiner M, Luft FC (1995). "Diagnosis of iron deficiency anemia in renal failure patients during the post-erythropoietin era". Am J Kidney Dis. 26 (2): 292–9. PMID 7645533.
- ↑ Eschbach JW, Cook JD, Scribner BH, Finch CA (1977). "Iron balance in hemodialysis patients". Ann Intern Med. 87 (6): 710–3. PMID 931207.
- ↑ 21.0 21.1 Hershko C, Camaschella C (2014). "How I treat unexplained refractory iron deficiency anemia". Blood. 123 (3): 326–33. doi:10.1182/blood-2013-10-512624. PMID 24215034.
- ↑ Iolascon A, d'Apolito M, Servedio V, Cimmino F, Piga A, Camaschella C (2006). "Microcytic anemia and hepatic iron overload in a child with compound heterozygous mutations in DMT1 (SCL11A2)". Blood. 107 (1): 349–54. doi:10.1182/blood-2005-06-2477. PMID 16160008.
- ↑ Coates A, Mountjoy M, Burr J (2017). "Incidence of Iron Deficiency and Iron Deficient Anemia in Elite Runners and Triathletes". Clin J Sport Med. 27 (5): 493–498. doi:10.1097/JSM.0000000000000390. PMID 27606953.
- ↑ Thomas DW, Hinchliffe RF, Briggs C, Macdougall IC, Littlewood T, Cavill I; et al. (2013). "Guideline for the laboratory diagnosis of functional iron deficiency". Br J Haematol. 161 (5): 639–48. doi:10.1111/bjh.12311. PMID 23573815.
- ↑ Simpson E, Mull JD, Longley E, East J (2000). "Pica during pregnancy in low-income women born in Mexico". West J Med. 173 (1): 20–4, discussion 25. PMC 1070964. PMID 10903283.
- ↑ Rector WG (1989). "Pica: its frequency and significance in patients with iron-deficiency anemia due to chronic gastrointestinal blood loss". J Gen Intern Med. 4 (6): 512–3. PMID 2585159.
- ↑ Reynolds RD, Binder HJ, Miller MB, Chang WW, Horan S (1968). "Pagophagia and iron deficiency anemia". Ann Intern Med. 69 (3): 435–40. PMID 5244572.
- ↑ Trost LB, Bergfeld WF, Calogeras E (2006). "The diagnosis and treatment of iron deficiency and its potential relationship to hair loss". J Am Acad Dermatol. 54 (5): 824–44. doi:10.1016/j.jaad.2005.11.1104. PMID 16635664.