Brucellosis pathophysiology
|
Brucellosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Brucellosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Brucellosis pathophysiology |
|
Risk calculators and risk factors for Brucellosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2] Danitza Lukac
Overview
Brucella is usually transmitted via the digestive route to the human host. Following transmission, white blood cells phagocyte the pathogen and transports it via the hematologic or lymphatic route to different organs, specially to those of the reticuloendothelial system.[1][2]
Pathophysiology
The pathophysiology of brucellosis may be described in the following steps:
Transmission:
| Humans are generally infected with brucellosis in one of three ways | |
|---|---|
Eating undercooked meat or consuming unpasteurized/raw dairy products |
The most common way to be infected is by eating or drinking unpasteurized/raw dairy products. When sheep, goats, cows, or camels are infected, their milk becomes contaminated with the bacteria.
If the milk from infected animals is not pasteurized, the infection will be transmitted to people who consume the milk and/or cheese products. |
Breathing in the bacteria that cause brucellosis (inhalation) |
Breathing in the bacteria that causes brucellosis may also lead to infection. This risk is generally greater for people in laboratories that work with the bacteria. In addition, slaughterhouse and meat-packing employees have also been known to be exposed to the bacteria and ultimately become infected. |
Bacteria entering the body through skin wounds or mucous membranes |
Bacteria can also enter wounds in the skin/mucous membranes through contact with infected animals.
This poses a problem for workers who have close contact with animals or animal excretions (newborn animals, fetuses, and excretions that may result from birth). Such workers may include:
|
| |
Incubation
Incubation period of brucellosis varies from one to four weeks. But occasionally, it may be as long as several months. [3][4]
Dissemination
Following transmission, brucellae is ingested by macrophages and polymorphonuclear cells. On ingestion, they replicate intracellularly inside the lysed cells, infecting the other cells or disseminating systemically. [5]
Seeding
- On transmission, Neutrophilic granulocytes and monocytes actively phagocytosed the bacteria, Initial attachment takes place via specific receptors, including Fc, C3, fibronectin, and mannose-binding proteins.
- Opsonized bacteria trigger an oxidative burst inside phagocytes. Unopsonized bacteria are internalized via similar receptors but at much lower efficiency. Smooth lipopolysaccharide (LPS), β-cyclic glucan, and possibly an invasion-attachment protein (IalB) are involved in this process.
- Initial intracellular replication of brucellae takes place within cells of the lymph nodes draining the point of entry. Followed by systemic hematogenous spread, resulting in chronic localizing infection at almost any site, although the reticuloendothelial system, musculoskeletal tissues, and genitourinary system are most frequently targeted.
Immune response
Brucellosis elicits both humoral and cell-mediated immune responses:[6]
Humoral immune response
Antibodies promote clearance of extracellular brucellae by bactericidal action and by facilitation of phagocytosis by polymorphonuclear and mononuclear phagocytes; however, antibodies alone cannot eradicate infection.
Cell-mediated immune response
- Tumor necrosis factor α (TNF-α) produced early in the course of infection stimulates T-cytotoxic lymphocytes and activates macrophages, which can kill intracellular brucellae
- Virulent brucella cells can suppress the TNF-α response, and control of infection in this situation depends on macrophage activation and interferon γ (IFN-γ) responses. Cytokines such as interleukin (IL) 12 promote production of IFN-γ, which drives TH1-type responses and stimulates macrophage activation. Inflammatory cytokines, including IL-4, IL-6, and IL-10, downregulate the protective response.
Pathogenesis
The pathogenesis of brucellosis involve the following:[7][8]
- Brucella, avoid triggering of innate immunity, permitting survival within monocytic cells.
- Endotoxic lipopolysaccharide LPS, plays a key role in pyrogenicity and in resistance to phagocytosis and serum killing in the nonimmune host.
- LPS plays a key role in suppressing phagosome–lysosome fusion and diverting the internalized bacteria into vacuoles located in endoplasmic reticulum, where intracellular replication takes place.
- Type IV secretion system (VirB) that regulates intracellular survival and trafficking has been identified.
- Brucellae, produce acid-stable proteins that facilitate the organisms’ survival in phagosomes and may enhance their resistance to reactive oxygen intermediates.
- A type III secretion system based on modified flagellar structures also has been inferred, although not yet confirmed.
- Virulent brucellae are resistant to defensins and produce a Cu-Zn superoxide dismutase that increases their resistance to reactive oxygen intermediates.
- A hemolysin-like protein may trigger the release of brucellae from infected cells.
Genetics
There is no known genetic association to brucellosis.
Associated conditions
Gross pathology
Microscopic Pathology
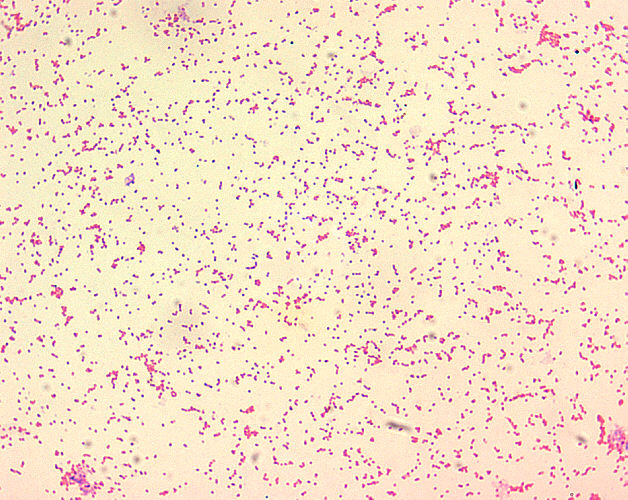
- Brucella spp. are poorly staining, small gram-negative coccobacilli (0.5-0.7 x 0.6-1.5 µm).
- Brucella spp. are seen mostly as single cells and appearing like “fine sand”.[9]
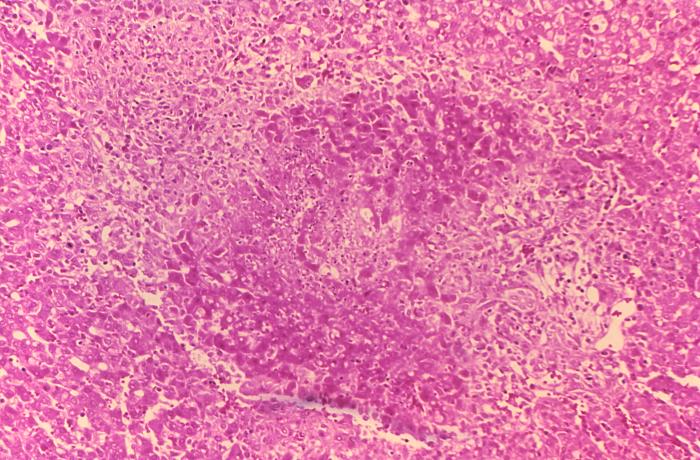
- On microscopic histopathological analysis of the liver, common findings are:
- Granulomas with centrilobular necrosis or focal necrosis and parenchyma destruction.[10]
-
Brucella spp. are poorly staining, small gram-negative coccobacilli (0.5-0.7 x 0.6-1.5 µm), and are seen mostly as single cells and appearing like “fine sand”.
-
Histopathology of guinea pig liver in experimental Brucella suis infection. Granuloma with necrosis.
Reference
- ↑ Corbel MJ (1997). "Brucellosis: an overview". Emerg Infect Dis. 3 (2): 213–21. doi:10.3201/eid0302.970219. PMC 2627605. PMID 9204307.
- ↑ Brucelosis. Wikipedia. https://es.wikipedia.org/wiki/Brucelosis. Accessed on February 2, 2016
- ↑ Mantur BG, Amarnath SK, Shinde RS. Review of clinical and laboratory features of human brucellosis. Indian J Med Microbiol 2007; 25:188.
- ↑ Fiori PL, Mastrandrea S, Rappelli P, Cappuccinelli P. Brucella abortus infection acquired in microbiology laboratories. J Clin Microbiol 2000; 38:2005.
- ↑ Barquero-Calvo E, Chaves-Olarte E, Weiss DS, et al. Brucella abortus uses a stealthy strategy to avoid activation of the innate immune system during the onset of infection. PLoS One 2007; 2:e631.
- ↑ Khan M, Harms JS, Marim FM, Armon L, Hall CL, Liu YP; et al. (2016). "The Bacterial Second Messenger Cyclic di-GMP Regulates Brucella Pathogenesis and Leads to Altered Host Immune Response". Infect Immun. 84 (12): 3458–3470. doi:10.1128/IAI.00531-16. PMC 5116723. PMID 27672085.
- ↑ Barquero-Calvo E, Chaves-Olarte E, Weiss DS, et al. Brucella abortus uses a stealthy strategy to avoid activation of the innate immune system during the onset of infection. PLoS One 2007; 2:e631.
- ↑ Gorvel JP, Moreno E. Brucella intracellular life: from invasion to intracellular replication. Vet Microbiol 2002; 90:281.
- ↑ Brucellosis. Wikipedia. https://en.wikipedia.org/wiki/Brucellosis. Accessed on January 29, 2016
- ↑ Hunt A, Bothwell P. Histological findings in human brucellosis. J Clin Pathol. 1967; 20: 267-272