Necrotizing fasciitis pathophysiology
|
Necrotizing fasciitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Necrotizing fasciitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Necrotizing fasciitis pathophysiology |
|
Risk calculators and risk factors for Necrotizing fasciitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Yamuna Kondapally, M.B.B.S[2]
Overview
The pathophysiology of necrotizing fasciitis is common to all types but the speed of development and associated clinical features differs depending on the causative organisms. Following transmission, the bacteria uses the entry site to invade the fascial planes which causes the wide spread necrosis of superficial fascia, deep fascia, subcutaneous fat, nerves, arteries, and veins. Necrotizing fasciitis can be a serious complication of omphalitis in the neonate.The pathogenesis of necrotizing fasciitis is the result of bacterial and host factors. The exact pathogenesis of type 1 necrotizing fasciitis is not fully understood but polymicrobial species work together to enhance the spread of infection (Synergistic). Group A streptococcus is the most common causative agent of type 2 NF. Bacterial virulence factors, exotoxins, superantigens and host immune system plays a major role in the pathogenesis of type II NF. Recurrent NF is caused by MRSA. On gross pathology, the characteristic findings of NF include subcutaneous emphysema, skin sloughing, bulae and necrosis. Inflammatory changes are seen on microscopic histopathology.
Pathophysiology
The pathophysiology of necrotizing fasciitis is common to all types of NF but the speed of development and associated clinical features differs depending on the causative organisms.
- The transmission of pathogens occurs through the following routes:
- External trauma (e.g., laceration, abrasion, burn, insect bite)
- Direct spread from a perforated viscus (particularly colon, rectum, or anus) or another surgical procedure (e.g., vasectomy, hemorrhoidectomy)
- Urogenital organ
- Perirectal abscess
- Decubitus ulcer
- Following transmission, the bacteria uses the entry site to invade the fascial planes which causes the wide spread necrosis of superficial fascia, deep fascia, subcutaneous fat, nerves, arteries, and veins.
- Superficial skin and deeper muscles are typically spared.
- In late stages, lesions develop liquefaction necrosis at all tissue levels.
Neonate
- Necrotizing fasciitis can be a serious complication of omphalitis in the neonate.
- The omphalitis may progress resulting in purplish discoloration and periumbilical necrosis.
- The necrosis may extend to the flanks and even onto the chest wall.
Pathogenesis
The pathogenesis of necrotizing fasciitis is the result of bacterial and host factors.
Type 1 NF
- The exact pathogenesis of type 1 necrotizing fasciitis is not fully understood.
- It is thought that type 1 NF is caused by polymicrobial species that work together to enhance the spread of infection (Synergistic).
- Synergistic NF is comparatively slow process evolving over days.
- It usually develops in the area where gut flora breaches the mucosa, entering the tissue planes.
Type 2 NF
- Group A streptococcus is the most common causative agent of type 2 NF.[1]
- Type 2 NF is initially insidious in onset but progress more rapidly.
- The disease may appear spontaneously with no obvious focus. Hematogenous infection from many foci such as skin, throat, ascending vaginitis, primary peritonitis reaches the fascial layer or seeds vimentin exposed by muscle damage.
- Direct inoculation of GAS through wounds or associated surgery is less common.
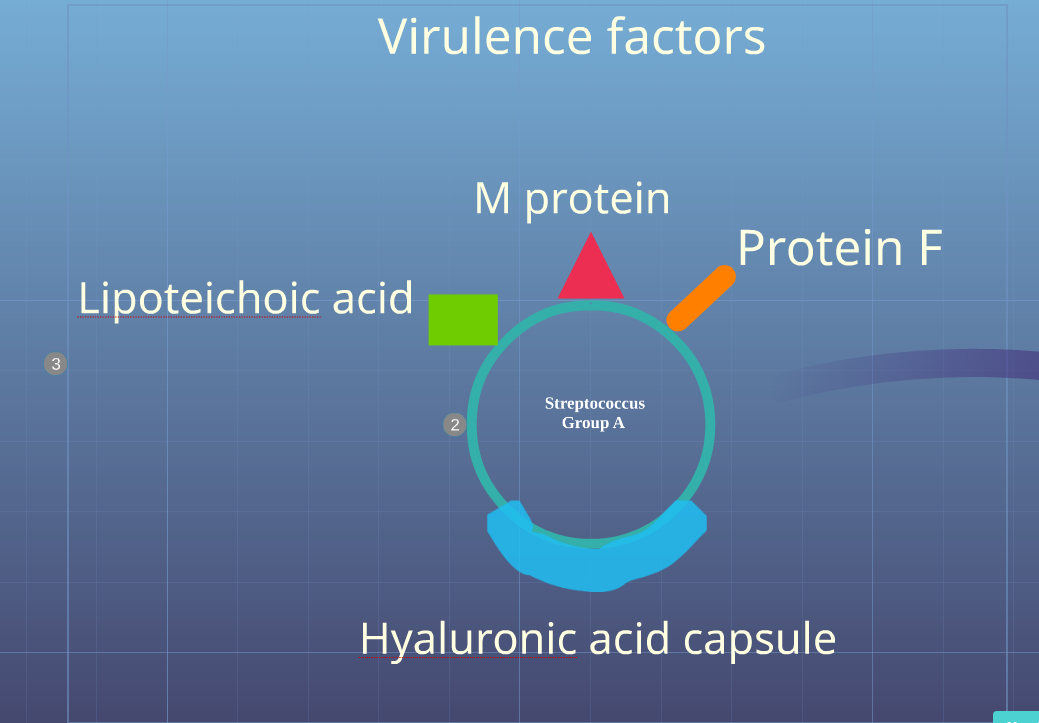
- The pathogenesis of type 2 NF is the result of the following process:
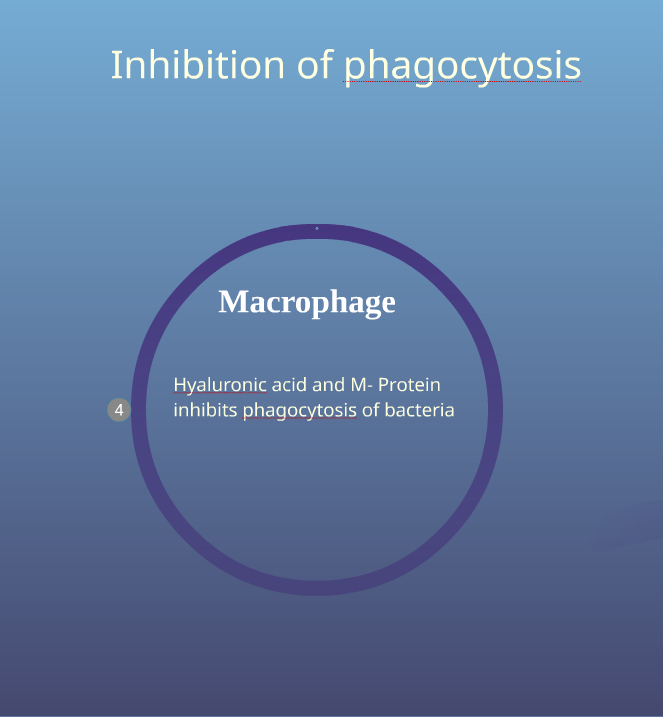
- Inhibition of phagocytosis of bacteria by hyaluronic acid capsule and M protein
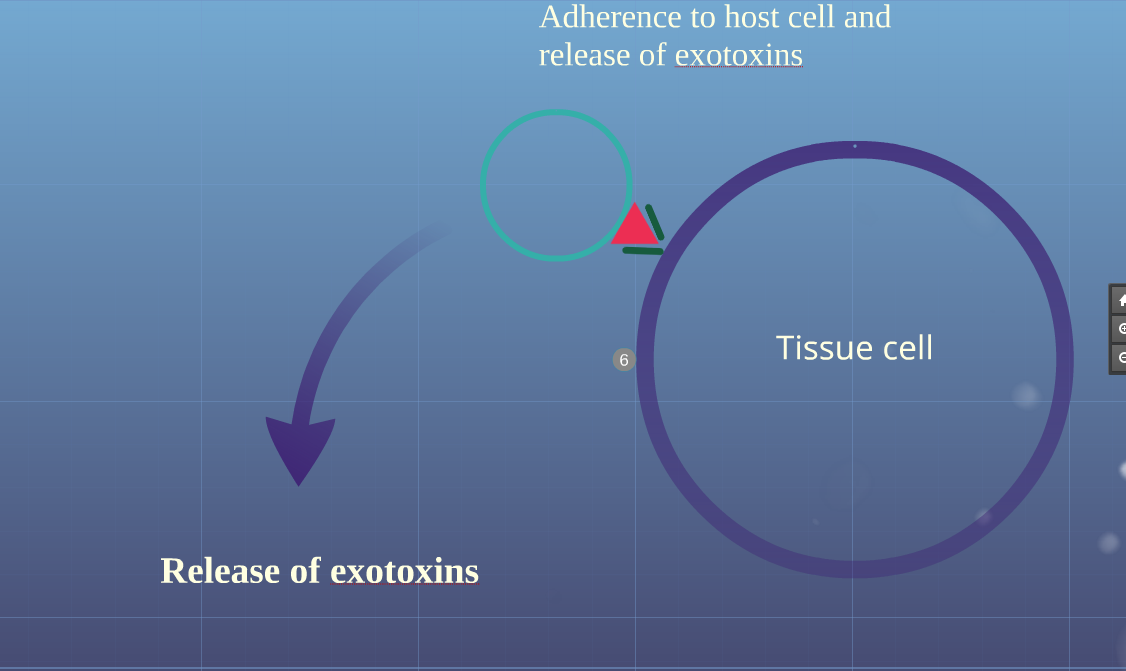
- Adherence of bacteria to host cell through adherence factors such as M protein, protein F and lipoteichoic acid
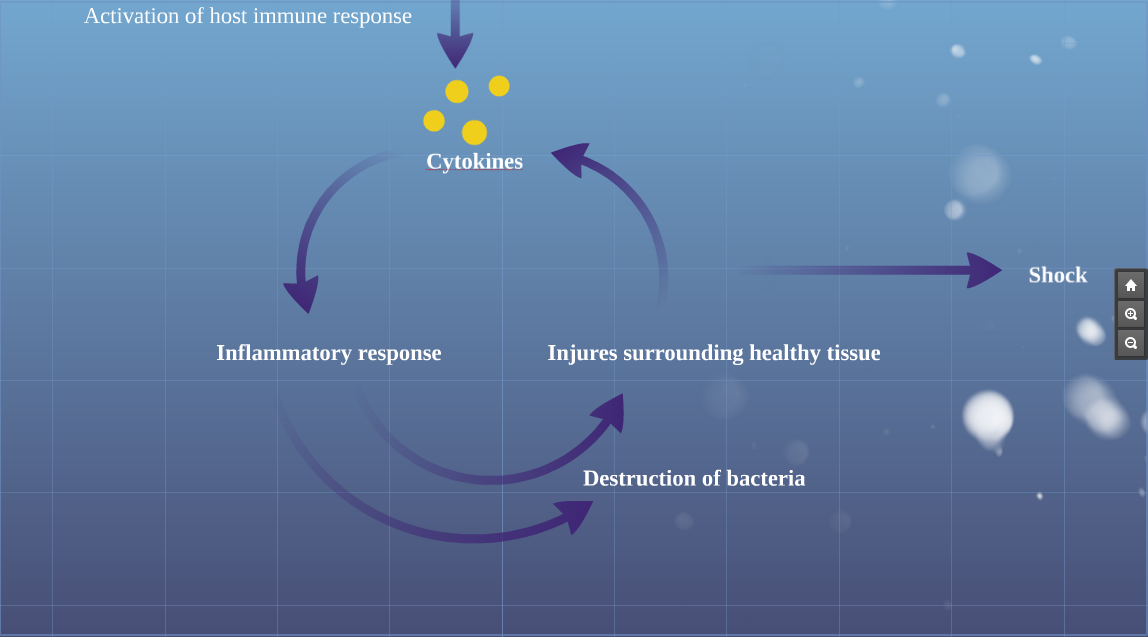
- Release of exotoxins (streptococcal pyogenic exotoxins and superantigens) into blood produce massive proliferation of T cells and cascading release of cytokines activating inflammatory process
- Activation of inflammatory process which begins to kill bacteria.
- The streptococci release massive amounts of enzymes, hemolysins, DNAase, proteases and collagenases which destroy the normal skin and surrounding tissue with progressive coagulative necrosis.
- The inflamed cells release more cytokines that stimulate more inflammatory cells
- The massive release of cytokines result in systemic inflammatory response syndrome resulting in shock, organ failure, depression of myocardial function and immune suppression
- Stimulation of T-cells by superantigens causes activation of complement pathway, the bradykinin-kallikrein system, and the coagulation cascade, worsening small vessel thrombosis and tissue ischemia. Tissue ischemia impedes oxidative destruction of bacteria by polymorphonuclear cells and prevents adequate delivery of antibiotics.
- The blood flow to local tissue is compromised due to thrombosis of large number of dermal capillaries by the local hypercoaguable state, platelet-neutrophil plugging of vessels and increased interstitial pressure.
- Nerves supplying the necrotizing areas of skin die, the central areas become anaesthetic and peripheral areas remain tender.
- In later stages, infection from deeper layers ascends, producing oedema of epidermal and dermal layers (peau d'orange) and a woody firmness of the tissues
- The fascial and nerve destruction results in sensory and motor deficits, which causes progression of hemorrhagic bullae to cutaneous gangrene.
-
Virulence Factors of Group A Streptococcus
-
Inhibition of phagocytosis
-
Adherance to host cell and release of exotoxins
-
Activation of host immune response
Recurrent necrotizing fasciitis
Recurrent NF is seen in following conditions:
- Methicillin resistant staphylococcus aureus MRSA
- Complement C4 deficiency
Gross pathology
On gross pathology the characteristic findings of necrotizing fasciitis include:[2]
- Subcutaneous emphysema
- Edema
- Erythema
- Bulae
- Skin sloughing
- Dull grey discoloration
Microscopic histopathological analysis
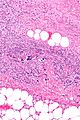
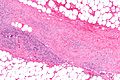
On microscopic histopathological analysis, the characteristic findings of necrotizing fasciitis are[2]
- Early stages
- Obliterative vasculitis with microangiopathic thrombosis
- Acute inflammation of subcutaneous tissue
- Superficial hyaline necrosis along with edema and inflammation of the dermis and subcutaneous fat
- Dense neutrophil-predominant inflammatory infiltrate
- Late stages
- Noninflammatory intravascular coagulation and hemorrhage
- Myonecrosis
References
- ↑ Leitch HA, Palepu A, Fernandes CM (2000). "Necrotizing fasciitis secondary to group A streptococcus. Morbidity and mortality still high". Can Fam Physician. 46: 1460–6. PMC 2144855. PMID 10925760.
- ↑ 2.0 2.1 2.2 2.3 Librae pathology(2015) https://librepathology.org/wiki/Necrotizing_fasciitis Accessed on September 2,2016
![Beginning of necrotizing fasciitis[2]](/images/a/a5/Beginning_of_Necrotizing_Fasciitis_01.jpg)
![Necrotizing fasciitis of left leg[2]](/images/0/0a/800px-Necrotizing_fasciitis_left_leg.JPEG)