Syphilis physical examination
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Aysha Anwar, M.B.B.S[2]
|
Syphilis Microchapters | |
|
Diagnosis | |
|
Treatment | |
|
Case Studies | |
|
Syphilis physical examination On the Web | |
|
American Roentgen Ray Society Images of Syphilis physical examination | |
|
Risk calculators and risk factors for Syphilis physical examination | |
Physical Examination
The physical exmaination findings of syphilis are described according to the stage of syphilis.[1][2][3]
| Stage of syphilis | Physical Examination | Images |
|---|---|---|
| Primary syphilis |
Chancre Regional lymphadenopathy
|
|
| Secondary syphilis |
Cardinal signs
Condylomata lata
Superficial mucosal patches |
|
| Latent syphilis |
|
|
| Tertiary syphilis |
Neurosyphilis
Cardiovascular syphilis Gummatous lesions
|
Primary syphilis: Chancre
- Afebrile
- Chancre:
- Regional lymphadenopathy accompanies primary lesion.
- Onset within a week.
- Unilateral or bilateral.
- Lymph nodes are firm, painless, non-tender and non-suppurative.
- Primary chancre heals spontaneously within 4-6 weeks; however, regional lymphadenopathy may persist for longer periods.
-
Primary stage syphilis sore (chancre) on the surface of a tongue.
-
Chancres on the penile shaft due to a primary syphilitic infection
-
Primary stage syphilis sore (chancre) on glans (head) of the penis.
-
Syphilis primary chancre.
-
Syphilis primary chancre.
-
Typical presentation of secondary syphilis rash on the palms of the hands and usually also seen on soles of feet
-
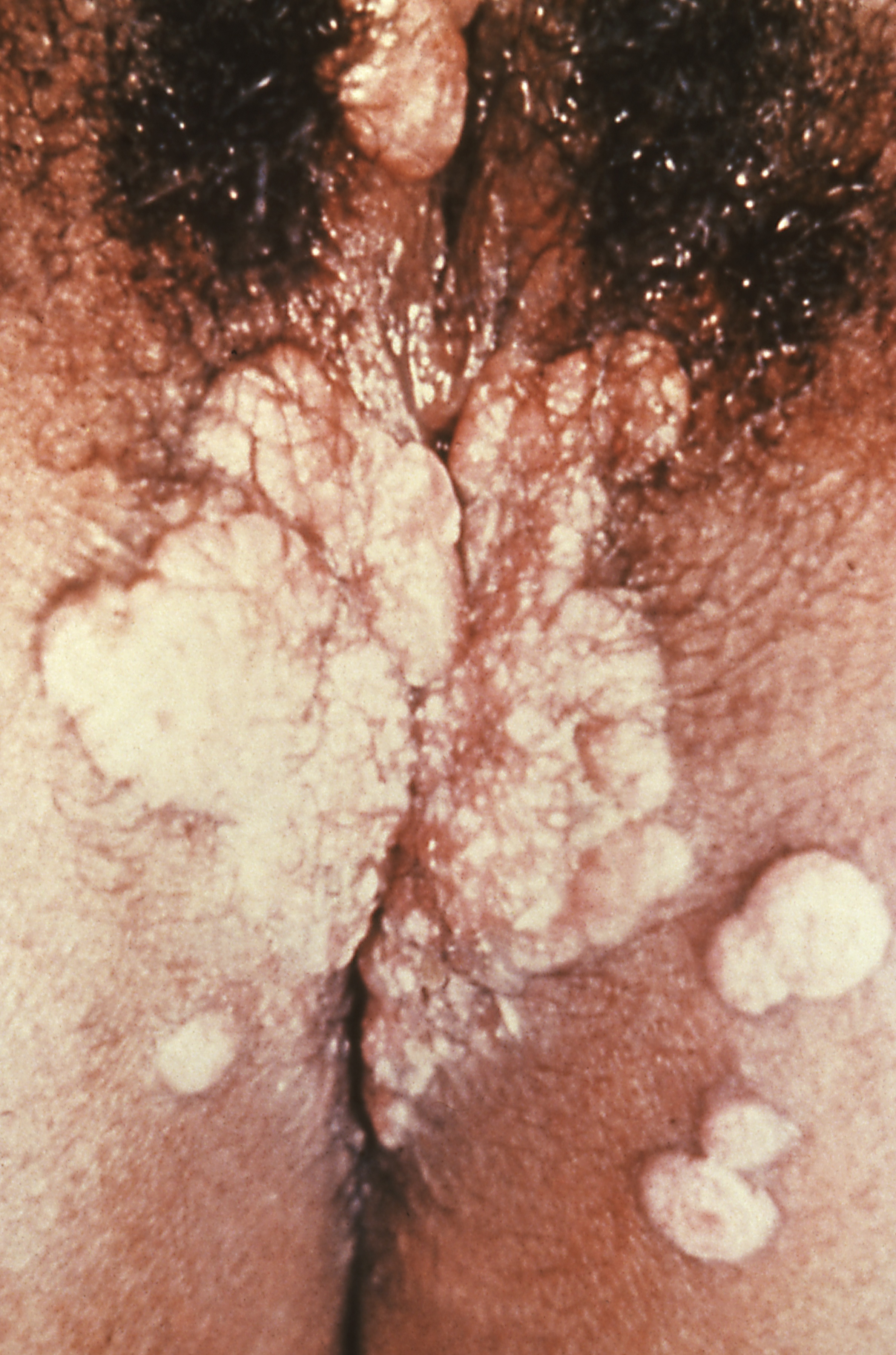
Condyoma lata (syphilis secondary)
-
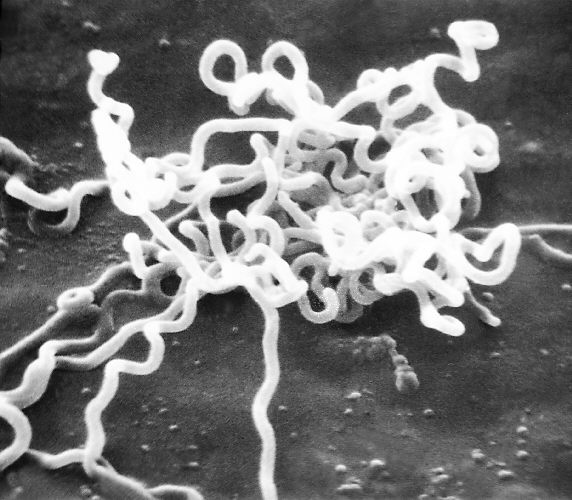
Electron micrograph of Treponema pallidum
-
Syphilis lesions on a patient's back
-
Syphilis lesions on a patient's chest
-
Chancres on the penile shaft due to a primary syphilitic infection
-
Secondary syphilis manifested perineal condylomata lata lesions, which presented as gray, raised papules that sometimes appear on the vulva or near the anus, or in any other warm intertriginous region.
-
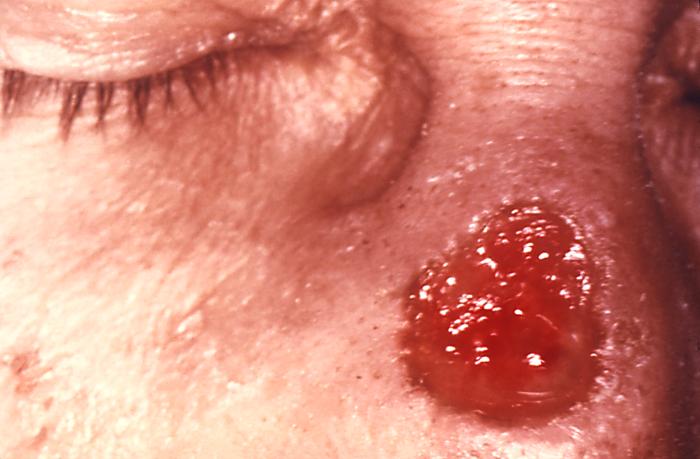
Gumma of the nose due to long standing tertiary syphilis
-
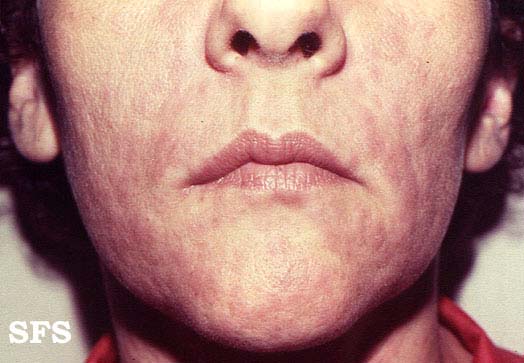
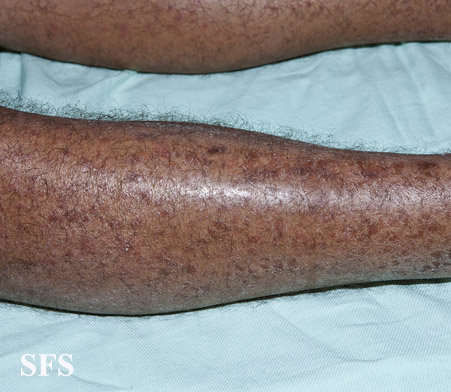
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
-
Secondary syphilis
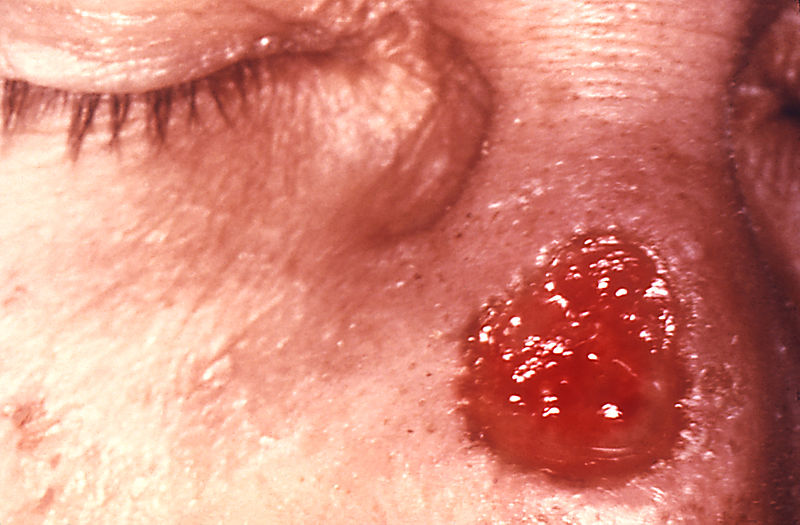
Tertiary syphilis: Gumma
- Soft, asymmetric, coalscent granulomatous lesion
- Solitary lesions less than a centimeter in diameter
- Appear almost anywhere in the body including in the skeleton
- Cutaneous gumma: indurated, nodular, papulosquamous to ulcerative lesions with peripheral hyperpigmentation
-
A gumma of nose due to a long standing tertiary syphilitic Treponema pallidum infection.
-
Tertiary syphilis
-
Tertiary syphilis
-
Tertiary syphilis
- Cardiovascular manifestation secondary to aortic dilation with resultant aortic regurgitation:
- Diastolic murmur
- De Musset's sign[5] a bobbing of the head that de Musset first noted in Parisian prostitutes
- Neurological manifestation:
- Asymptomatic meningitis
- Asymptomatic neurosyphilis usually has no signs or symptoms and is diagnosed exclusively with the presence of CSF abnormalities notably pleocytosis, elevated protein, decreased glucose or a positive VDRL test.
- Symptomatic meningitis
- Develops within 6-months to several years of primary infection
- Typical meningitis symptoms present
- Cranial nerve abnormalities may be observed
- Meningovascular syphilis
- Occurs a few months to 10 years (average, 7 years) after the primary infection
- Associated with prodromal symptoms lasting weeks to months before focal deficits are identifiable
- Focal deficits initially are intermittent or progress slowly over a few days
- Clinical present with CNS vascular insufficiency or stroke involving the middle cerebral artery
- Parenchymatous neurosyphilis
- Develops 15-20 years after primary infection
- Clinical presents as general paresis or tabes dorsalis with resultant ataxia
- Argyll Robertson pupil: small irregular pupil
Ophthalmic Examination
- Slit-lamp examination and ophthalmic examination may be helpful to differentiate between acquired and congenital syphilis.
- Presence of interstitial keratitis is suggestive of congenital syphilis with latent infection of unknown duration.
Clinical pearl: Syphilis detecting Handshake
{{#ev:youtube|SAedwyzTMWA}}
References
- ↑ Singh AE, Romanowski B (1999). "Syphilis: review with emphasis on clinical, epidemiologic, and some biologic features". Clin Microbiol Rev. 12 (2): 187–209. PMC 88914. PMID 10194456.
- ↑ Carlson JA, Dabiri G, Cribier B, Sell S (2011). "The immunopathobiology of syphilis: the manifestations and course of syphilis are determined by the level of delayed-type hypersensitivity". Am J Dermatopathol. 33 (5): 433–60. doi:10.1097/DAD.0b013e3181e8b587. PMC 3690623. PMID 21694502.
- ↑ Wöhrl S, Geusau A (2007). "Clinical update: syphilis in adults". Lancet. 369 (9577): 1912–4. doi:10.1016/S0140-6736(07)60895-2. PMID 17560432.
- ↑ Sapira JD (1981 Apr). ""Quincke, de Musset, Duroziez, and Hill: some aortic regurgitations"". South Med J. 74 (4): 459–67. Check date values in:
|date=(help) - ↑ Sapira JD (1981 Apr). ""Quincke, de Musset, Duroziez, and Hill: some aortic regurgitations"". South Med J. 74 (4): 459–67. Check date values in:
|date=(help)