Small cell carcinoma of the lung pathophysiology: Difference between revisions
| Line 21: | Line 21: | ||
==Smoking== | ==Smoking== | ||
* It is well established the relationship between | * It is well established the relationship between smoking and lung cancer, since 1950 several studies had shown the increased risk of smoking and lung cancer. <ref>{{Cite journal | ||
| author = [[R. DOLL]] & [[A. B. HILL]] | | author = [[R. DOLL]] & [[A. B. HILL]] | ||
| title = Smoking and carcinoma of the lung; preliminary report | | title = Smoking and carcinoma of the lung; preliminary report | ||
| Line 42: | Line 42: | ||
| pmid = 22943444 | | pmid = 22943444 | ||
}}</ref> | }}</ref> | ||
* There are more than 60 carcinogens in a cigarette,<ref name="Hecht">{{cite journal | last =Hecht | first =S | title =Tobacco carcinogens, their biomarkers and tobacco-induced cancer | journal =Nature Reviews. Cancer | volume =3 | issue =10 | pages =733–744 | publisher =Nature Publishing Group | date =Oct 2003 | url =http://www.nature.com/nrc/journal/v3/n10/abs/nrc1190_fs.html;jsessionid=A78B217DFCAD36DD965F2DBA685CF121 | doi =10.1038/nrc1190 |pmid =14570033 | accessdate =2007-08-10 }}</ref> including [[radioisotopes]] from the [[radon]] decay sequence, [[nitrosamine]], and [[benzopyrene]]. Nicotine appears to depress the immune response to malignant growths in exposed tissue. | |||
* There is evidence that lung cancer in never-smokers has a better prognosis than in smokers,<ref name="Nordquist">{{cite journal | last =Nordquist | first =LT | authorlink = | coauthors =Simon GR, Cantor A et al. | title =Improved survival in never-smokers vs current smokers with primary adenocarcinoma of the lung | journal =Chest | volume =126 | issue =2 | pages =347–351| publisher = American College of Chest Physicians | date =Aug 2004 | url =http://www.chestjournal.org/cgi/content/full/126/2/347 |pmid =15302716 | accessdate =2007-08-10 }}</ref> and that patients who smoke at the time of diagnosis have shorter survival than those who have quit.<ref name="Tammemagi">{{cite journal | last =Tammemagi | first =CM | authorlink = | coauthors =Neslund-Dudas C, Simoff M, Kvale P | title =Smoking and lung cancer survival: the role of comorbidity and treatment | journal =Chest | volume =125 |issue =1 | pages =27–37 | publisher =American College of Chest Physicians | date =Jan 2004 | url =http://www.chestjournal.org/cgi/content/full/125/1/27 | pmid =14718417 | accessdate =2007-08-10 }}</ref> | |||
==Paraneoplastic Syndrome== | ==Paraneoplastic Syndrome== | ||
Revision as of 19:17, 9 June 2014
|
Small Cell Carcinoma of the Lung Microchapters |
|
Differentiating Small Cell Carcinoma of the Lung from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Small cell carcinoma of the lung pathophysiology On the Web |
|
American Roentgen Ray Society Images of Small cell carcinoma of the lung pathophysiology |
|
Small cell carcinoma of the lung pathophysiology in the news |
|
Directions to Hospitals Treating Small cell carcinoma of the lung |
|
Risk calculators and risk factors for Small cell carcinoma of the lung pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Small cell lung cancer is the most aggressive form of lung cancer. It usually starts in the breathing tubes (bronchi) in the center of the chest. Although the cancer cells are small, they grow very quickly and create large tumors. These tumors often spread rapidly (metastasize) to other parts of the body, including the brain, liver, and bone.
Molecular Abnormalities
A mutation in p53 is found in 75% to 100% of cases of small cell carcinoma. Other molecular abnormalities have been described that influence in the development of small cell carcinoma, such as chromosome 3p deletion, MYC amplification, BCL2 expression, GRP (gastrin-releasing peptide) expression , RB1 deletion (loss of RB1 protein), VEGF (vascular endothelial growth factor) expression, c-kit/SCFR (stem cell factor receptor) coexpression.[1]
Smoking
- It is well established the relationship between smoking and lung cancer, since 1950 several studies had shown the increased risk of smoking and lung cancer. [2][3]
- There are more than 60 carcinogens in a cigarette,[4] including radioisotopes from the radon decay sequence, nitrosamine, and benzopyrene. Nicotine appears to depress the immune response to malignant growths in exposed tissue.
- There is evidence that lung cancer in never-smokers has a better prognosis than in smokers,[5] and that patients who smoke at the time of diagnosis have shorter survival than those who have quit.[6]
Paraneoplastic Syndrome
- Small cell carcinoma is one of the most common tumors associated to a paraneoplastic syndrome. The most common endocrine condition is SIADH, where there is an excessive secretion of ADH which leads to hyponatremia. Other conditions that are related to small cell carcinoma are the secretion of ANP, where the patient has hyponatremia, natriuresis and hypotension; ectopic ACTH production, which causes Cushing syndrome; and Lambert-Eaton syndrome, where there are antibodies that are directed against the antigens of the neuromuscular junction.
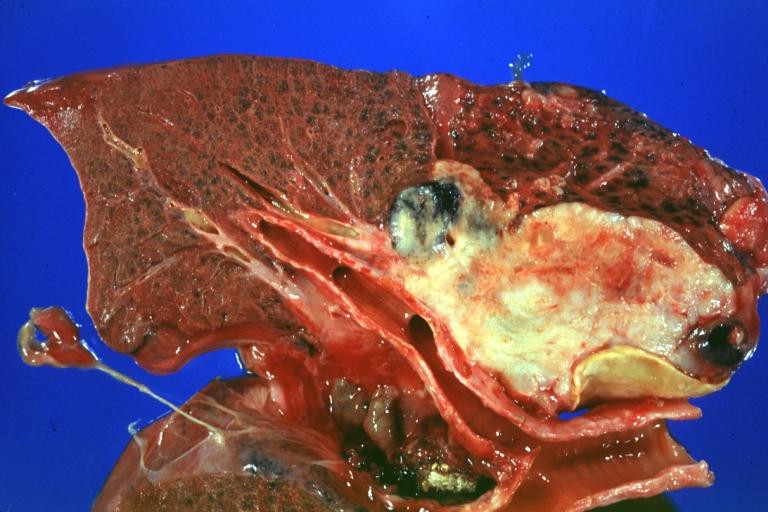
Gross Pathology
- The tumor cells are small and round, but sometimes can be ovoid or spindle shaped. They have a scant cytoplasm with a high mitotic count and a hyperchromatic nuclei. Nearly all SCLC are immunoreactive for keratin, thyroid transcription factor 1, and epithelial membrane antigen. Neuroendocrine and neural differentiation result in the expression of dopa decarboxylase, calcitonin, neuron-specific enolase, chromogranin A, CD56 (also known as nucleosomal histone kinase 1 or neural-cell adhesion molecule), gastrin-releasing peptide, and insulin-like growth factor 1. One or more markers of neuroendocrine differentiation can be found in approximately 75% of SCLC
References
- ↑ Grace K. Dy & Alex A. Adjei (2002). "Novel targets for lung cancer therapy: part I". Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 20 (12): 2881–2894. PMID 12065566. Unknown parameter
|month=ignored (help) - ↑ R. DOLL & A. B. HILL (1950). "Smoking and carcinoma of the lung; preliminary report". British medical journal. 2 (4682): 739–748. PMID 14772469. Unknown parameter
|month=ignored (help) - ↑ Peter N. Lee, Barbara A. Forey & Katharine J. Coombs (2012). "Systematic review with meta-analysis of the epidemiological evidence in the 1900s relating smoking to lung cancer". BMC cancer. 12: 385. doi:10.1186/1471-2407-12-385. PMID 22943444.
- ↑ Hecht, S (Oct 2003). "Tobacco carcinogens, their biomarkers and tobacco-induced cancer". Nature Reviews. Cancer. Nature Publishing Group. 3 (10): 733–744. doi:10.1038/nrc1190. PMID 14570033. Retrieved 2007-08-10.
- ↑ Nordquist, LT (Aug 2004). "Improved survival in never-smokers vs current smokers with primary adenocarcinoma of the lung". Chest. American College of Chest Physicians. 126 (2): 347–351. PMID 15302716. Retrieved 2007-08-10. Unknown parameter
|coauthors=ignored (help) - ↑ Tammemagi, CM (Jan 2004). "Smoking and lung cancer survival: the role of comorbidity and treatment". Chest. American College of Chest Physicians. 125 (1): 27–37. PMID 14718417. Retrieved 2007-08-10. Unknown parameter
|coauthors=ignored (help)