Gout: Difference between revisions
No edit summary |
No edit summary |
||
| Line 36: | Line 36: | ||
==Diagnosis== | ==Diagnosis== | ||
[[Gout history and symptoms|History and Symptoms]] | [[Gout physical examination|Physical Examination]] | [[Gout laboratory findings|Laboratory Findings]] | [[Gout x ray|X-ray]] | [[Gout MRI|MRI]] | [[Gout history and symptoms|History and Symptoms]] | [[Gout physical examination|Physical Examination]] | [[Gout laboratory findings|Laboratory Findings]] | [[Gout x ray|X-ray]] | [[Gout MRI|MRI]] | ||
==Treatment== | ==Treatment== | ||
[[Gout medical therapy|Medical Therapy]] | [[Gout surgery|Surgery]] | |||
==Prevention== | ==Prevention== | ||
| Line 282: | Line 158: | ||
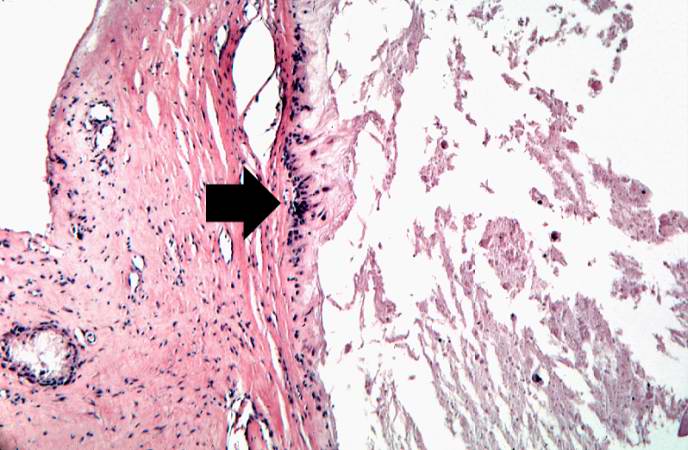
[[Image:Gout case 8.jpg|left|thumb|400px|This is a gross photograph of a tophus on the great toe of another patient with gout (arrow). The healed surgical incision and the size of this tophus indicate that this was a long-standing problem for this patient. ]] | [[Image:Gout case 8.jpg|left|thumb|400px|This is a gross photograph of a tophus on the great toe of another patient with gout (arrow). The healed surgical incision and the size of this tophus indicate that this was a long-standing problem for this patient. ]] | ||
<br clear="left"/> | <br clear="left"/> | ||
==See also== | ==See also== | ||
Revision as of 17:11, 21 August 2012
For patient information click here
| Gout | |
 | |
|---|---|
| Tophaceous Gout (Image courtesy of Charlie Goldberg, M.D.) | |
| ICD-10 | M10 |
| ICD-9 | 274.0 274.1 274.8 274.9 |
| OMIM | 138900 300323 |
| DiseasesDB | 29031 |
| MeSH | D006073 |
|
Gout Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Gout On the Web |
|
American Roentgen Ray Society Images of Gout |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Historical Perspective
Pathophysiology
Clinical Stages
1. Asymptomatic hyperuricemia
2. Acute gouty arthritis
3. Intercritical gout
4. Chronic tophaceous gout.
Diagnosis
History and Symptoms | Physical Examination | Laboratory Findings | X-ray | MRI
Treatment
Prevention
Medications
- Allopurinol and azathioprine (Imuran) used together present a risk of a potentially fatal drug interaction, a severe risk of allopurinol use which is of importance to transplant patients being treated with azathioprine for immunosuppression.[3]
- Febuxostat ((2-[3-cyano-4-isobutoxyphenyl]-4-methylthiazole-5-carboxylic acid) - a non-purine inhibitor of xanthine oxidase seems to be an alternative that is superior to allopurinol; it is currently in Phase III trials.[1]
- Probenecid, a uricosuric drug that promotes the excretion of uric acid in urine, is also commonly prescribed - often in conjunction with colchicine. The drug fenofibrate (which is used in treating hyperlipidemia) also exerts a beneficial uricosuric effect.[2]
- As arterial hypertension quite often coexists with gout, treating it with losartan, an angiotensin II receptor antagonist, might have an additional beneficial effect on uric acid plasma levels. This way losartan can offset the negative side-effect of thiazides (a group of diuretics used for high blood pressure) on uric acid metabolism in patients with gout.
- It is suspected that in many cases gout may be secondary to untreated sleep apnea, when oxygen-starved cells break down and release purines as a by-product. Treatment for apnea can be effective in lessening incidence of acute gout attacks.[3]
- A study in 2004 suggests that animal flesh sources of purine, such as beef and seafood, greatly increase the risk of developing gout. However, high-purine vegetable sources did not. Dairy products such as milk and cheese significantly reduced the chances of gout. The study followed over 40000 men over a period of 12 years, in which 1300 cases of gout were reported.[4]
- PEG-uricase, a polyethylene glycol ("PEG") conjugate of recombinant porcine uricase (urate oxidase), which breaks down the uric acid deposits is being studied in Phase III clinical trials for the treatment of severe, treatment-refractory gout in the United States in 2006.Pipeline
- Sodium bicarbonate (baking soda) is an old remedy,[5] thought to work by raising blood pH (lowering blood acidity). However, the added sodium may be inappropriate for some people.
- Research from the University of British Columbia suggests long-term coffee consumption is associated with a lower risk of gout.[6] [7]
Diet
See Saag and Choi, 2006, an open-access review article, for detailed references and further information.[8]
The serum level of uric acid is the primary risk factor for gout. The serum level is the result of both intake (diet) and output (excretion).
Reduce intake of purines
The solubility threshold for uric acid is approximately 6.7 mg/dl; above this threshold crystals may form. Healthy subjects in the Normative Aging Study who had serum levels of uric acid over 9.0 mg/dl suffered a 22% incidence of gout over six years, compared to less than one percent for those with 7.0-8.9 mg/dl. The average uric acid level in men is 5.0 mg/dl, and substitution of a purine-free formula diet reduces this to 3.0 mg/dl. A purine-restricted diet lowers the level nearly as much (1-2 mg/dl).
A diet low in purines reduces the serum level of uric acid. Notable sources of dietary purines include:
- beer (high in guanosine
Protein is a crude proxy for purines; a more precise proxy is muscle. Apart from the notable dietary purines above, the main source of dietary purines is DNA and RNA, via their bases adenine and guanine. All sources of dietary protein supply some purines, but some sources provide far more purines than others. Meat (particularly dark meat) and seafood are high in purine because muscle cells are packed with mitochondria, which have their own DNA and RNA. In a large prospective study, high consumption of meat and seafood were found associated with an elevated risk of gout onset (41% and 50%, respectively). High consumption of dairy products, high in protein but very low in DNA and RNA, was associated with a 44% decrease in the incidence of gout. Consumption of the more purine-rich vegetables or a high protein diet per se had no significant correlation.
Consumption of beer is associated with a 49% increase in relative risk per daily 12-oz serving. By contrast, consumption of spirits was associated with only a 15% increase in relative risk, and no association at all was found with consumption of wine.
Some medical drugs are purine-based. Notable among these are the purine-analog antimetabolite drugs, sometimes used as chemotherapy agents.
Increase output of uric acid
Ingestion of 500 mg of Vitamin C per day has been shown to bring about a 0.5 mg/dl decrease in serum uric acid through increased excretion. Some Gout sufferers have recently found that taking up to 1,000 mg of Vitamin C, combined with a small dosage (approx. 10-15 mg./day) of Lithium have had very beneficial effects on their uric acid levels.
Vitamin C, taken in high doses, can help decrease blood uric acid levels, but should not be taken without a doctor's supervision. Note that there is a small subset of people with gout who will actually get worse with high levels of vitamin C. Also, a single high dose can free up too much uric acid and cause kidney stones. (University of Maryland Medical Center for Integrative Medicine).
Other approaches
Additional dietary recommendations can be made which reduce gout indirectly, by reducing gout risk factors such as obesity, hypertension, cardiovascular disease, diabetes, and metabolic syndrome.
The following suggestions do not meet with universal approval among medical practitioners.
Low purine diet:
- To lower uric acid:
- cherries were reported to reduce uric acid in a small study.[9][10]
- celery extracts (celery or celery seed either in capsule form or as a tea) is believed by many to reduce uric acid levels (although these are also diuretics). Celery extracts have been reported to act synergistically with anti-inflammatory drugs.[11]
- Cheese has been recommended as a low-purine food,[12] and dairy products have been found to reduce the risk of gout.
- Food to avoid:
- foods high in purines
- limit food high in protein such as meat, fish, poultry, or tofu to 8 ounces (226 grams) a day. Avoid entirely during a flare up. Tofu has been proposed as a safe source of protein for gout patients due to its small and transient effect on plasma urate levels.[13]
- sweetbreads, kidneys, liver, brains, or other offal meats.[14][15]
- sardines and anchovies [16]
- seafood [17]
- alcohol.[18] Some claim that this applies especially to beer, on the basis that brewer's yeasts are very rich in purine. Since most modern commercial beer contains only trace amounts of yeast, this claim requires further substantiation. Formerly, port wine was sweetened with litharge, causing lead poisoning, of which gout is a complication. Ironically, red wines, particularly those produced by traditional methods,[19] contain procyanidins released from grape seeds during wine making, which have been reported to lower serum uric acid levels by an indirect mechanism.[20] However, withdrawal of urate-lowering therapy is associated with recurrence of acute gouty arthritis.[21]
- meat extracts, consommés, and gravies[22]
- foods high in purines
- To avoid dehydration:
- Drink plenty of liquids, especially water, to dilute and assist excretion of urates;
- Avoid diuretic foods or medicines like aspirin(aspirin should be avoided from those suffering from gout, unless specified by a trained physician), vitamin C, tea and alcohol. The role of diuretics in triggering gout has been disputed.[23]
- Moderate intake of purine-rich vegetables is not associated with increased gout.[4]
Case Examples
Case #1
Clinical Summary
This patient was diagnosed with gout approximately 20 years ago. At that time, he noted the gradual onset of pain in the left knee, followed by swelling, redness and heat, all of which persisted for approximately one month. Shortly thereafter, he had periodic episodes of hot, painful, swollen joints involving the left knee, left ankle, and both first metatarsophalangeal joints. At this time the patient was hospitalized for evaluation of these arthritides. Serum uric acid values on three separate occasions were 8.0, 9.3, and 8.7 mg/dl. In addition to the presence of the painful swollen joints, a gouty tophus was present on the left arm. The patient was readmitted to the hospital from time to time because of acute exacerbations of gouty arthritis. On the most recent hospital admission, a 3-cm tophus was found over the right elbow, as well as several smaller tophi over the right hand.
Autopsy Findings
The specimen consisted of an elliptically shaped, mottled, yellow-white irregular hard mass, measuring 8.0 x 5.0 x 2.0 cm. in diameter.
Histopathological Findings







See also
- Pseudogout is a very similar disease, but caused by deposition of calcium pyrophosphate, not uric acid.
References
- ↑ Becker M, Schumacher H, Wortmann R, MacDonald P, Eustace D, Palo W, Streit J, Joseph-Ridge N (2005). "Febuxostat compared with allopurinol in patients with hyperuricemia and gout". N Engl J Med. 353 (23): 2450&ndash, 61. PMID 16339094.
- ↑ Bardin T (2003). "Fenofibrate and losartan". Ann Rheum Dis. 62 (6): 497&ndash, 8. PMID 12759281.
- ↑ Abrams B (2005). "Gout is an indicator of sleep apnea". Sleep. 28 (2): 275. PMID 16171252.
- ↑ 4.0 4.1 Choi H, Atkinson K, Karlson E, Willett W, Curhan G (2004). "Purine-rich foods, dairy and protein intake, and the risk of gout in men" (PDF). N Engl J Med. 350 (11): 1093&ndash, 103. PMID 15014182.
- ↑ The British Pharmaceutical Codex. Published by direction of the Council of the Pharmaceutical Society of Great Britain, 1911. Sodium
- ↑ Hyon K. Choi, Walter Willett, Gary Curhan (2007). "Coffee consumption and risk of incident gout in men: A prospective study". Arthritis & Rheumatism. 56 (6): 2049&ndash, 2055. PMID 17530645.
- ↑ Choi HK, Curhan G. (2007). "Coffee, tea, and caffeine consumption and serum uric acid level: The third national health and nutrition examination survey". Arthritis & Rheumatism. 57 (5): 816&ndash, 821. PMID 17530681.
- ↑ Saag KG, Choi H (2006). "Epidemiology, risk factors, and lifestyle modifications for gout". Arthritis Res. Ther. 8 Suppl 1: S2. doi:10.1186/ar1907. PMID 16820041.
- ↑ Jacob RA, Spinozzi GM, Simon VA; et al. (2003). "Consumption of cherries lowers plasma urate in healthy women". J. Nutr. 133 (6): 1826–9. PMID 12771324.
- ↑ BLAU LW (1950). "Cherry diet control for gout and arthritis". Tex. Rep. Biol. Med. 8 (3): 309–11. PMID 14776685.
- ↑ Whitehouse MW, Butters DE (2003). "Combination anti-inflammatory therapy: synergism in rats of NSAIDs/corticosteroids with some herbal/animal products". Inflammopharmacology. 11 (4): 453–64. doi:10.1163/156856003322699636. PMID 15035799.
- ↑ Harris MD, Siegel LB, Alloway JA (1999). "Gout and hyperuricemia". American family physician. 59 (4): 925–34. PMID 10068714.
- ↑ Yamakita J, Yamamoto T, Moriwaki Y, Takahashi S, Tsutsumi Z, Higashino K (1998). "Effect of Tofu (bean curd) ingestion and on uric acid metabolism in healthy and gouty subjects". Adv. Exp. Med. Biol. 431: 839–42. PMID 9598181.
- ↑ Robinson CH (1954). "The low purine diet". Am. J. Clin. Nutr. 2 (4): 276–7. PMID 13188851.
- ↑ Chou P, Soong LN, Lin HY (1993). "Community-based epidemiological study on hyperuricemia in Pu-Li, Taiwan". J. Formos. Med. Assoc. 92 (7): 597–602. PMID 7904493.
- ↑ Robinson CH (1954). "The low purine diet". Am. J. Clin. Nutr. 2 (4): 276–7. PMID 13188851.
- ↑ Choi HK, Atkinson K, Karlson EW, Willett W, Curhan G (2004). "Purine-rich foods, dairy and protein intake, and the risk of gout in men". N. Engl. J. Med. 350 (11): 1093–103. doi:10.1056/NEJMoa035700. PMID 15014182.
- ↑ Choi HK, Atkinson K, Karlson EW, Willett W, Curhan G (2004). "Alcohol intake and risk of incident gout in men: a prospective study". Lancet. 363 (9417): 1277–81. doi:10.1016/S0140-6736(04)16000-5. PMID 15094272.
- ↑ Corder R, Mullen W, Khan NQ; et al. (2006). "Oenology: red wine procyanidins and vascular health". Nature. 444 (7119): 566. doi:10.1038/444566a. PMID 17136085.
- ↑ Wang Y, Zhu JX, Kong LD, Yang C, Cheng CH, Zhang X (2004). "Administration of procyanidins from grape seeds reduces serum uric acid levels and decreases hepatic xanthine dehydrogenase/oxidase activities in oxonate-treated mice". Basic Clin. Pharmacol. Toxicol. 94 (5): 232–7. doi:10.1111/j.1742-7843.2004.pto940506.x. PMID 15125693.
- ↑ Perez-Ruiz F, Atxotegi J, Hernando I, Calabozo M, Nolla JM (2006). "Using serum urate levels to determine the period free of gouty symptoms after withdrawal of long-term urate-lowering therapy: a prospective study". Arthritis Rheum. 55 (5): 786–90. doi:10.1002/art.22232. PMID 17013833.
- ↑ Robinson CH (1954). "The low purine diet". Am. J. Clin. Nutr. 2 (4): 276–7. PMID 13188851.
- ↑ Janssens HJ, van de Lisdonk EH, Janssen M, van den Hoogen HJ, Verbeek AL (2006). "Gout, not induced by diuretics? A case-control study from primary care". Ann. Rheum. Dis. 65 (8): 1080–3. doi:10.1136/ard.2005.040360. PMID 16291814.
Additional References
- Katzung, Bertram G. Basic and Clinical Pharmacology, 10th edition. New York: McGraw Hill Medical, 2007. pp. 242
External links
- "American College of Rheumatology". March 23, 2007. Retrieved 2007-03-23. Text " American College of Rheumatology " ignored (help)- (ACR Fact Sheet on Gout)
- "Answers and Questions on Gout". U.S. National Institutes of Health—National Institute of Arthritis and Musculoskeletal and Skin Diseases. September 28th, 2007. Retrieved 2007-08-28. Check date values in:
|date=(help) - "Diet and gout". A-Z Health Guide. webMD.com. July 01, 2004. Retrieved 2006-09-18. Check date values in:
|date=(help) - "Coffee Consumption and Reduced Gout Risk". Drinking coffee reduces risk of gout in middle age men. U.S. National Institutes of Health. Retrieved 2007-05-25.
- "Purine content in food". British Dalmatian Club. Retrieved 2006-09-18.
- Gout in Depth - How Stuff Works
Template:Diseases of the musculoskeletal system and connective tissue
ar:نقرس bg:Подагра cs:Dna da:Gigt de:Gicht eo:Podagro fa:نقرس io:Kiragro id:Gout it:Gotta he:שיגדון lb:Giicht ms:Gout nl:Jicht no:Urinsyregikt sk:Dna sr:Гихт fi:Kihti sv:Gikt te:గౌటు