Tibial plateau fracture classification: Difference between revisions
No edit summary |
No edit summary |
||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
There are multiple classifications available for tibial plateau fracture. The most common classification systems for tibial plateau fracture include Schatzker, Hohl and Moore, Luo's three column concept and AO classification. | There are multiple [[Classification|classifications]] available for tibial plateau fracture. The most common classification systems for tibial plateau fracture include Schatzker, Hohl and Moore, Luo's three column concept and AO [[classification]]. | ||
==Classification== | ==Classification== | ||
There are multiple classifications available for tibial plateau fracture. The most common classification systems for tibial plateau fracture include Schatzker, Hohl and Moore, Luo's three column concept and AO/OTA classification.<ref>{{cite book | last = Rockwood | first = Charles | title = Rockwood and Green's fractures in adults | publisher = Wolters Kluwer Health/Lippincott Williams & Wilkins | location = Philadelphia, PA | year = 2010 | isbn = 9781605476773 }}</ref><ref>{{cite book | last = Azar | first = Frederick | title = Campbell's operative orthopaedics | publisher = Elsevier | location = Philadelphia, PA | year = 2017 | isbn = 9780323374620 }}</ref> | There are multiple [[Classification|classifications]] available for tibial plateau fracture. The most common [[classification]] systems for tibial plateau fracture include Schatzker, Hohl and Moore, Luo's three column concept and AO/OTA [[classification]].<ref>{{cite book | last = Rockwood | first = Charles | title = Rockwood and Green's fractures in adults | publisher = Wolters Kluwer Health/Lippincott Williams & Wilkins | location = Philadelphia, PA | year = 2010 | isbn = 9781605476773 }}</ref><ref>{{cite book | last = Azar | first = Frederick | title = Campbell's operative orthopaedics | publisher = Elsevier | location = Philadelphia, PA | year = 2017 | isbn = 9780323374620 }}</ref> | ||
===Schatzker Classification=== | ===Schatzker Classification=== | ||
| Line 22: | Line 22: | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type I | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type I | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Lateral split fracture | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Lateral split [[Bone fracture|fracture]] | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" | Type II | | style="background: #4479BA; color: #FFFFFF; text-align: center;" | Type II | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Lateral Split-depressed fracture | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Lateral Split-depressed [[Bone fracture|fracture]] | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type III | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type III | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Lateral Pure depression fracture | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Lateral Pure depression [[Bone fracture|fracture]] | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type IV | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type IV | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Medial plateau fracture | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Medial plateau [[Bone fracture|fracture]] | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type V | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type V | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Bicondylar fracture | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Bicondylar [[Bone fracture|fracture]] | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type VI | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type VI | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Metaphyseal-diaphyseal | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Metaphyseal-diaphyseal [[Dissociation (chemistry)|dissociation]] | ||
|} | |} | ||
===Hohl and Moore Classification=== | ===Hohl and Moore Classification=== | ||
* Hohl and Moore classification of tibial plateau fracture is useful for fracture dislocation, fracture patterns that cannot be classified by Schatzker classification and fractures associated with knee instability.<ref>Hohl M, Moore TM. Articular fractures of the proximal tibia. In: Evarts CM, editor. Surgery of the musculoskeletal system. 2nd ed., New York: Churchill Livingstone; 1990. </ref> | * Hohl and Moore [[classification]] of tibial plateau fracture is useful for [[fracture]] [[dislocation]], [[fracture]] patterns that cannot be classified by Schatzker [[classification]] and [[fractures]] associated with [[Instability|knee instability]].<ref>Hohl M, Moore TM. Articular fractures of the proximal tibia. In: Evarts CM, editor. Surgery of the musculoskeletal system. 2nd ed., New York: Churchill Livingstone; 1990. </ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 47: | Line 47: | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type I | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type I | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Coronal split fracture | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Coronal split [[fracture]] | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type II | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type II | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Entire condylar fracture | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Entire condylar [[Bone fracture|fracture]] | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type III | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type III | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Rim avulsion fracture of lateral plateau | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Rim avulsion [[Bone fracture|fracture]] of lateral plateau | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type IV | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type IV | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Rim compression fracture | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Rim compression [[Bone fracture|fracture]] | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type V | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |Type V | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Four-part fracture | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Four-part [[Bone fracture|fracture]] | ||
|} | |} | ||
===Luo's Three Column Classification=== | ===Luo's Three Column Classification=== | ||
* Luo's classified tibial plateau fracture based on computed tomography ‘‘three column fixation’’ concept which aided in column-specific fixation technique.<ref name="pmid20881634">{{cite journal| author=Luo CF, Sun H, Zhang B, Zeng BF| title=Three-column fixation for complex tibial plateau fractures. | journal=J Orthop Trauma | year= 2010 | volume= 24 | issue= 11 | pages= 683-92 | pmid=20881634 | doi=10.1097/BOT.0b013e3181d436f3 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20881634 }} </ref> | * Luo's [[Classification|classified]] tibial plateau fracture based on [[computed tomography]] ‘‘three column fixation’’ concept which aided in column-specific [[fixation]] technique.<ref name="pmid20881634">{{cite journal| author=Luo CF, Sun H, Zhang B, Zeng BF| title=Three-column fixation for complex tibial plateau fractures. | journal=J Orthop Trauma | year= 2010 | volume= 24 | issue= 11 | pages= 683-92 | pmid=20881634 | doi=10.1097/BOT.0b013e3181d436f3 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20881634 }} </ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 72: | Line 72: | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |1 Column fracture | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |1 Column fracture | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Lateral column fracture | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Lateral column [[Bone fracture|fracture]] | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |2 Column fracture | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |2 Column fracture | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Lateral and posterior column fracture | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Lateral and posterior column [[Bone fracture|fracture]] | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |3 Column fracture | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |3 Column fracture | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Bicondylar fracture dividing into three fragments | | style="background: #F5F5F5; padding: 5px; text-align: center;" |Bicondylar [[Bone fracture|fracture]] dividing into three fragments | ||
|} | |} | ||
===OTA System=== | ===OTA System=== | ||
*AO/ASIF classification is also a widely accepted classification.<ref>ME Muller, S Nazarian, P Koch. Classification AO des fractures. 1 Les os longs. Springler-Verlag, Berlin, 1987.</ref> | *AO/ASIF [[classification]] is also a widely accepted [[classification]].<ref>ME Muller, S Nazarian, P Koch. Classification AO des fractures. 1 Les os longs. Springler-Verlag, Berlin, 1987.</ref> | ||
*Proximal tibia is given the number 41 based on the classification. | *Proximal [[tibia]] is given the number 41 based on the classification. | ||
*It is further subdivided as: | *It is further subdivided as: | ||
| Line 90: | Line 89: | ||
|- | |- | ||
| rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |A | | rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |A | ||
| colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |Extra-articular fractures | | colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |Extra-articular [[Bone fracture|fractures]] | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |A1 | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |A1 | ||
| Line 102: | Line 101: | ||
|- | |- | ||
| rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |B | | rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |B | ||
| colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" | | colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |Partial articular [[Bone fracture|fractures]] | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |B1 | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |B1 | ||
| Line 114: | Line 113: | ||
|- | |- | ||
| rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |C | | rowspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |C | ||
| colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |Complete articular fractures | | colspan="2" style="background: #DCDCDC; padding: 5px; text-align: center;" |Complete articular [[Bone fracture|fractures]] | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |C1 | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |C1 | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Articular simple + [[metaphyseal]] simple | | style="background: #F5F5F5; padding: 5px; text-align: center;" |[[Articular]] simple + [[metaphyseal]] simple | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |C2 | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |C2 | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Articular simple, [[metaphyseal]] multifragmentary | | style="background: #F5F5F5; padding: 5px; text-align: center;" |[[Articular]] simple, [[metaphyseal]] multifragmentary | ||
|- | |- | ||
| style="background: #4479BA; color: #FFFFFF; text-align: center;" |C3 | | style="background: #4479BA; color: #FFFFFF; text-align: center;" |C3 | ||
| style="background: #F5F5F5; padding: 5px; text-align: center;" |Articular multifragmentary | | style="background: #F5F5F5; padding: 5px; text-align: center;" |[[Articular]] multifragmentary | ||
|} | |} | ||
Revision as of 21:10, 5 February 2019
|
Tibial plateau fracture Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tibial plateau fracture classification On the Web |
|
American Roentgen Ray Society Images of Tibial plateau fracture classification |
|
Risk calculators and risk factors for Tibial plateau fracture classification |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rohan A. Bhimani, M.B.B.S., D.N.B., M.Ch.[2]
Overview
There are multiple classifications available for tibial plateau fracture. The most common classification systems for tibial plateau fracture include Schatzker, Hohl and Moore, Luo's three column concept and AO classification.
Classification
There are multiple classifications available for tibial plateau fracture. The most common classification systems for tibial plateau fracture include Schatzker, Hohl and Moore, Luo's three column concept and AO/OTA classification.[1][2]
Schatzker Classification
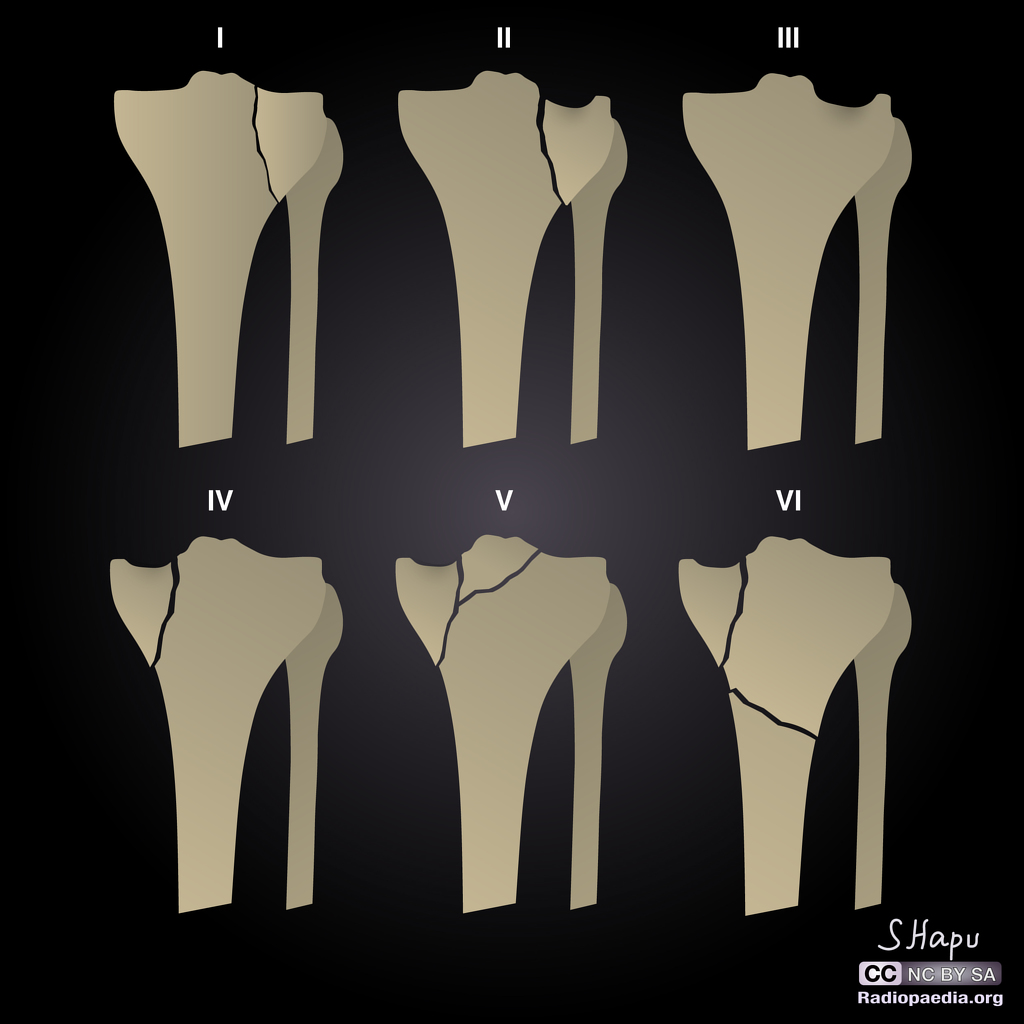 |
- Schatzker classification is the most commonly used classification for tibial plateau fracture.[3]
| Schatzker Classification | |
|---|---|
| Type I | Lateral split fracture |
| Type II | Lateral Split-depressed fracture |
| Type III | Lateral Pure depression fracture |
| Type IV | Medial plateau fracture |
| Type V | Bicondylar fracture |
| Type VI | Metaphyseal-diaphyseal dissociation |
Hohl and Moore Classification
- Hohl and Moore classification of tibial plateau fracture is useful for fracture dislocation, fracture patterns that cannot be classified by Schatzker classification and fractures associated with knee instability.[4]
| Hohl and Moore Classification | |
|---|---|
| Type I | Coronal split fracture |
| Type II | Entire condylar fracture |
| Type III | Rim avulsion fracture of lateral plateau |
| Type IV | Rim compression fracture |
| Type V | Four-part fracture |
Luo's Three Column Classification
- Luo's classified tibial plateau fracture based on computed tomography ‘‘three column fixation’’ concept which aided in column-specific fixation technique.[5]
| Luo's Three Column Classification | |
|---|---|
| Zero-column fracture | Pure articular depression |
| 1 Column fracture | Lateral column fracture |
| 2 Column fracture | Lateral and posterior column fracture |
| 3 Column fracture | Bicondylar fracture dividing into three fragments |
OTA System
- AO/ASIF classification is also a widely accepted classification.[6]
- Proximal tibia is given the number 41 based on the classification.
- It is further subdivided as:
| OTA System | ||
|---|---|---|
| A | Extra-articular fractures | |
| A1 | Avulsion | |
| A2 | Metaphyseal simple | |
| A3 | Metaphyseal multifragmentary | |
| B | Partial articular fractures | |
| B1 | Pure split | |
| B2 | Pure depression | |
| B3 | Split depression | |
| C | Complete articular fractures | |
| C1 | Articular simple + metaphyseal simple | |
| C2 | Articular simple, metaphyseal multifragmentary | |
| C3 | Articular multifragmentary | |
References
- ↑ Rockwood, Charles (2010). Rockwood and Green's fractures in adults. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins. ISBN 9781605476773.
- ↑ Azar, Frederick (2017). Campbell's operative orthopaedics. Philadelphia, PA: Elsevier. ISBN 9780323374620.
- ↑ Schatzker J, McBroom R, Bruce D (1979). "The tibial plateau fracture. The Toronto experience 1968--1975". Clin Orthop Relat Res (138): 94–104. PMID 445923.
- ↑ Hohl M, Moore TM. Articular fractures of the proximal tibia. In: Evarts CM, editor. Surgery of the musculoskeletal system. 2nd ed., New York: Churchill Livingstone; 1990.
- ↑ Luo CF, Sun H, Zhang B, Zeng BF (2010). "Three-column fixation for complex tibial plateau fractures". J Orthop Trauma. 24 (11): 683–92. doi:10.1097/BOT.0b013e3181d436f3. PMID 20881634.
- ↑ ME Muller, S Nazarian, P Koch. Classification AO des fractures. 1 Les os longs. Springler-Verlag, Berlin, 1987.