Parathyroid hormone (injection): Difference between revisions
No edit summary |
No edit summary |
||
| Line 21: | Line 21: | ||
|blackBoxWarningBody=''<span style="color:#FF0000;">POTENTIAL RISK OF [[OSTEOSARCOMA]]:</span>'' | |blackBoxWarningBody=''<span style="color:#FF0000;">POTENTIAL RISK OF [[OSTEOSARCOMA]]:</span>'' | ||
* In male and female rats, [[parathyroid hormone]] caused an increase in the incidence of [[osteosarcoma]] (a malignant bone tumor) that was dependent on dose and treatment duration. A risk to humans could not be excluded. | * In male and female rats, [[parathyroid hormone]] caused an increase in the incidence of [[osteosarcoma]] (a malignant bone tumor) that was dependent on dose and treatment duration. A risk to humans could not be excluded. | ||
* Because of the potential risk of [[osteosarcoma]], prescribe | * Because of the potential risk of [[osteosarcoma]], prescribe [[Parathyroid hormone]] ([[Injection]]) only to patients who cannot be well-controlled on [[calcium]] and active forms of [[vitamin D]] and for whom the potential benefits are considered to outweigh the potential risk. | ||
* Avoid use of | * Avoid use of [[Parathyroid hormone]] ([[Injection]]) in patients who are at increased baseline risk for [[osteosarcoma]] (including those with [[Paget's disease of bone]] or unexplained elevations of [[alkaline phosphatase]], pediatric and young adult patients with open [[epiphyses]], patients with hereditary disorders predisposing to [[osteosarcoma]] or patients with a history of prior external beam or implant [[radiation therapy]] involving the skeleton). | ||
* | * [[Parathyroid hormone]] ([[Injection]]) is available only through a restricted program called the [[Parathyroid hormone]] ([[Injection]]) REMS Program. | ||
|fdaLIADAdult===== INDICATIONS AND USAGE ==== | |fdaLIADAdult===== INDICATIONS AND USAGE ==== | ||
[[Parathyroid hormone]] ([[Injection]]) is a [[parathyroid hormone]] indicated as an adjunct to [[calcium]] and [[vitamin D]] to control [[hypocalcemia]] in patients with [[hypoparathyroidism]]. | |||
===== Limitations of Use ===== | ===== Limitations of Use ===== | ||
* Because of the potential risk of [[osteosarcoma]], | * Because of the potential risk of [[osteosarcoma]], [[Parathyroid hormone]] ([[Injection]]) is recommended only for patients who cannot be well-controlled on [[calcium]] supplements and active forms of [[vitamin D]] alone. | ||
* | * [[Parathyroid hormone]] ([[Injection]]) was not studied in patients with [[hypoparathyroidism]] caused by [[calcium]]-sensing receptor mutations. | ||
* | * [[Parathyroid hormone]] ([[Injection]]) was not studied in patients with acute post-surgical [[hypoparathyroidism]]. | ||
==== DOSAGE AND ADMINISTRATION ==== | ==== DOSAGE AND ADMINISTRATION ==== | ||
* The dose of | * The dose of [[Parathyroid hormone]] ([[Injection]]) should be individualized to achieve a serum [[calcium level]] in the lower half of the normal range. | ||
* Confirm [[vitamin D]] stores are sufficient and serum [[calcium]] is above 7.5 mg/dL before starting | * Confirm [[vitamin D]] stores are sufficient and serum [[calcium]] is above 7.5 mg/dL before starting [[Parathyroid hormone]] ([[Injection]]). | ||
* The starting dose of | * The starting dose of [[Parathyroid hormone]] ([[Injection]]) is 50 mcg injected once daily in the thigh. When starting [[Parathyroid hormone]] ([[Injection]]), decrease dose of active [[vitamin D]] by 50%, if serum calcium is above 7.5 mg/dL. | ||
* Monitor serum calcium levels every 3 to 7 days after starting or adjusting | * Monitor serum calcium levels every 3 to 7 days after starting or adjusting [[Parathyroid hormone]] ([[Injection]]) dose and when adjusting either active vitamin D or calcium supplements dose while using [[Parathyroid hormone]] ([[Injection]]). | ||
==== DOSAGE FORMS AND STRENGTHS ==== | ==== DOSAGE FORMS AND STRENGTHS ==== | ||
* | * [[Parathyroid hormone]] ([[Injection]]) is supplied as a multiple-dose, dual-chamber glass cartridge containing a sterile lyophilized powder and a sterile diluent for reconstitution in four dosage strengths. | ||
* For [[injection]]: 25 mcg, 50 mcg, 75 mcg, or 100 mcg. | * For [[injection]]: 25 mcg, 50 mcg, 75 mcg, or 100 mcg. | ||
|offLabelAdultGuideSupport=There is limited information regarding ''Off-Label Guideline-Supported Use'' of Parathyroid hormone (Injection) in adult patients. | |offLabelAdultGuideSupport=There is limited information regarding ''Off-Label Guideline-Supported Use'' of Parathyroid hormone (Injection) in adult patients. | ||
| Line 45: | Line 45: | ||
* In male and female rats, parathyroid hormone caused an increase in the incidence of [[osteosarcoma]] (a malignant bone tumor). | * In male and female rats, parathyroid hormone caused an increase in the incidence of [[osteosarcoma]] (a malignant bone tumor). | ||
* The occurrence of [[osteosarcoma]] was observed to be dependent on [[parathyroid hormone]] dose and treatment duration. | * The occurrence of [[osteosarcoma]] was observed to be dependent on [[parathyroid hormone]] dose and treatment duration. | ||
* This effect was observed at parathyroid hormone exposure levels ranging from 3 to 71 times the exposure levels for humans receiving a 100 mcg dose of | * This effect was observed at parathyroid hormone exposure levels ranging from 3 to 71 times the exposure levels for humans receiving a 100 mcg dose of [[Parathyroid hormone]] ([[Injection]]). | ||
* These data could not exclude a risk to humans. | * These data could not exclude a risk to humans. | ||
* Because of a potential risk of osteosarcoma, use | * Because of a potential risk of osteosarcoma, use [[Parathyroid hormone]] ([[Injection]]) only in patients who cannot be well-controlled on calcium supplements and active forms of vitamin D alone and for whom the potential benefits are considered to outweigh this potential risk. | ||
* To further mitigate the potential risk of [[osteosarcoma]], avoid use of | * To further mitigate the potential risk of [[osteosarcoma]], avoid use of [[Parathyroid hormone]] ([[Injection]]) in patients who are at increased risk for [[osteosarcoma]], such as patients with Paget's disease of bone or unexplained elevations of alkaline phosphatase, pediatric and young adult patients with open epiphyses, patients with hereditary disorders predisposing to osteosarcoma, or patients with a prior history of external beam or implant radiation therapy involving the skeleton. | ||
* Instruct patients to promptly report clinical symptoms (e.g., persistent localized pain) and signs (e.g., soft tissue mass tender to palpation) that could be consistent with osteosarcoma. | * Instruct patients to promptly report clinical symptoms (e.g., persistent localized pain) and signs (e.g., soft tissue mass tender to palpation) that could be consistent with osteosarcoma. | ||
* | * [[Parathyroid hormone]] ([[Injection]]) is available only through a restricted program under a REMS. | ||
==== | ==== [[Parathyroid hormone]] ([[Injection]]) REMS Program ==== | ||
* Because of the potential risk of osteosarcoma associated with | * Because of the potential risk of osteosarcoma associated with [[Parathyroid hormone]] ([[Injection]]) therapy, [[Parathyroid hormone]] ([[Injection]]) is available only through a restricted REMS program called the NATPARA REMS Program. | ||
* Under the | * Under the [[Parathyroid hormone]] ([[Injection]]) REMS Program, only certified healthcare providers can prescribe and only certified pharmacies can dispense [[Parathyroid hormone]] ([[Injection]]). | ||
==== Hypercalcemia ==== | ==== Hypercalcemia ==== | ||
* Severe hypercalcemia has been reported with | * Severe hypercalcemia has been reported with [[Parathyroid hormone]] ([[Injection]]). | ||
* In the pivotal trial, 3 patients randomized to | * In the pivotal trial, 3 patients randomized to [[Parathyroid hormone]] ([[Injection]]) required administration of IV fluids to correct [[hypercalcemia]] during treatment with [[Parathyroid hormone]] ([[Injection]]). | ||
* The risk is highest when starting or increasing the dose of | * The risk is highest when starting or increasing the dose of [[Parathyroid hormone]] ([[Injection]]), but can occur at any time. | ||
* Monitor serum calcium and patients for signs and symptoms of [[hypercalcemia]]. | * Monitor serum calcium and patients for signs and symptoms of [[hypercalcemia]]. | ||
* Treat hypercalcemia per standard practice and consider holding and/or lowering the dose of | * Treat hypercalcemia per standard practice and consider holding and/or lowering the dose of [[Parathyroid hormone]] ([[Injection]]) if severe hypercalcemia occurs. | ||
==== Hypocalcemia ==== | ==== Hypocalcemia ==== | ||
* Severe [[hypocalcemia]] has been reported with | * Severe [[hypocalcemia]] has been reported with [[Parathyroid hormone]] ([[Injection]]). | ||
* The risk is highest when | * The risk is highest when [[Parathyroid hormone]] ([[Injection]]) is withheld, missed or abruptly discontinued, but can occur at any time. | ||
* Monitor serum calcium and patients for signs and symptoms of hypocalcemia. | * Monitor serum calcium and patients for signs and symptoms of hypocalcemia. | ||
* Resume treatment with, or increase the dose of, an active form of vitamin D or calcium supplements or both if indicated in patients interrupting or discontinuing | * Resume treatment with, or increase the dose of, an active form of vitamin D or calcium supplements or both if indicated in patients interrupting or discontinuing [[Parathyroid hormone]] ([[Injection]]) to prevent severe hypocalcemia. | ||
==== Risk of [[Digoxin]] Toxicity with Concomitant Use of Digitalis Compounds ==== | ==== Risk of [[Digoxin]] Toxicity with Concomitant Use of Digitalis Compounds ==== | ||
* The inotropic effects of digoxin are affected by serum calcium levels. | * The inotropic effects of digoxin are affected by serum calcium levels. | ||
* [[Hypercalcemia]] of any cause may predispose to digoxin toxicity. | * [[Hypercalcemia]] of any cause may predispose to digoxin toxicity. | ||
* In patients using | * In patients using [[Parathyroid hormone]] ([[Injection]]) concomitantly with digitalis compounds, monitor serum calcium and digoxin levels and patients for signs and symptoms of digitalis toxicity. | ||
* Adjustment of digoxin and/or | * Adjustment of digoxin and/or [[Parathyroid hormone]] ([[Injection]]) may be needed. | ||
* No drug-drug interaction study has been conducted with digoxin and | * No drug-drug interaction study has been conducted with digoxin and [[Parathyroid hormone]] ([[Injection]]). | ||
|clinicalTrials==== Adverse Reactions in Clinical Trials for Hypoparathyroidism === | |clinicalTrials==== Adverse Reactions in Clinical Trials for Hypoparathyroidism === | ||
* Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other clinical trials and may not reflect the rates observed in clinical practice. | * Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other clinical trials and may not reflect the rates observed in clinical practice. | ||
* | * [[Parathyroid hormone]] ([[Injection]]) was studied in a placebo-controlled trial. | ||
* The data described in Table 1 below reflect exposure to | * The data described in Table 1 below reflect exposure to [[Parathyroid hormone]] ([[Injection]]) in 84 patients, including 78 exposed for 24 weeks. | ||
* The mean age of the trial population was 47 years and ranged from 19 to 74 years old. | * The mean age of the trial population was 47 years and ranged from 19 to 74 years old. | ||
* Seventy-nine percent (79%) were females. | * Seventy-nine percent (79%) were females. | ||
| Line 83: | Line 82: | ||
* The mean eGFR at baseline was 97.4 mL/min/1.73 m2 and 45%, 10% and 0% had mild, moderate and severe renal impairment, respectively, at baseline. | * The mean eGFR at baseline was 97.4 mL/min/1.73 m2 and 45%, 10% and 0% had mild, moderate and severe renal impairment, respectively, at baseline. | ||
* During the trial, most patients received 100 mcg and the dose range was 50 to 100 mcg administered [[subcutaneously]] once daily in the thigh. | * During the trial, most patients received 100 mcg and the dose range was 50 to 100 mcg administered [[subcutaneously]] once daily in the thigh. | ||
* Table 1 lists common adverse reactions associated with | * Table 1 lists common adverse reactions associated with [[Parathyroid hormone]] ([[Injection]]) use in the clinical trial. | ||
* Common adverse reactions were reactions that occurred in ≥5% of subjects and occurred more commonly on | * Common adverse reactions were reactions that occurred in ≥5% of subjects and occurred more commonly on [[Parathyroid hormone]] ([[Injection]]) than on placebo. | ||
TABLE 1: | TABLE 1: | ||
==== Hypercalcemia ==== | ==== Hypercalcemia ==== | ||
* In the overall pivotal trial a greater proportion of patients on | * In the overall pivotal trial a greater proportion of patients on [[Parathyroid hormone]] ([[Injection]]) had albumin-corrected serum calcium above the normal range (8.4 to 10.6 mg/dL). | ||
* During the entire trial duration 3 patients on | * During the entire trial duration 3 patients on [[Parathyroid hormone]] ([[Injection]]) and 1 patient on placebo had a calcium level above 12 mg/dL. | ||
* Table 2 displays the number of subjects who had albumin-corrected serum calcium levels above the normal range (8.4 to 10.6 mg/dL) by study treatment period in the placebo-controlled study based on routine monitoring at each trial visit. | * Table 2 displays the number of subjects who had albumin-corrected serum calcium levels above the normal range (8.4 to 10.6 mg/dL) by study treatment period in the placebo-controlled study based on routine monitoring at each trial visit. | ||
* More patients randomized to | * More patients randomized to [[Parathyroid hormone]] ([[Injection]]) had hypercalcemia in both phases of the study (note: all trial participants underwent a 50% reduction in active vitamin D dose at randomization). | ||
Table 2 | Table 2 | ||
==== Hypocalcemia ==== | ==== Hypocalcemia ==== | ||
* Table 3 displays the number of subjects who had albumin-corrected serum calcium levels below 8.4 mg/dL by treatment period in the placebo-controlled study based on routine monitoring at each trial visit. | * Table 3 displays the number of subjects who had albumin-corrected serum calcium levels below 8.4 mg/dL by treatment period in the placebo-controlled study based on routine monitoring at each trial visit. | ||
* More patients randomized to placebo had hypocalcemia of less than 7 mg/dL in the titration phase (note: all trial participants underwent a 50% reduction in active vitamin D dose at randomization). | * More patients randomized to placebo had hypocalcemia of less than 7 mg/dL in the titration phase (note: all trial participants underwent a 50% reduction in active vitamin D dose at randomization). | ||
* More patients randomized to | * More patients randomized to [[Parathyroid hormone]] ([[Injection]]) had hypocalcemia of less than 7 mg/dL in the dose maintenance phase. | ||
Table 3: | Table 3: | ||
* The risk of hypocalcemia increases when | * The risk of hypocalcemia increases when [[Parathyroid hormone]] ([[Injection]]) is withdrawn. | ||
* At the end of the trial, | * At the end of the trial, [[Parathyroid hormone]] ([[Injection]]) and placebo were withdrawn, calcium and active vitamin D were returned to baseline doses and subjects were followed for 4 weeks. | ||
* During this withdrawal phase, more patients previously randomized to | * During this withdrawal phase, more patients previously randomized to [[Parathyroid hormone]] ([[Injection]]) experienced an albumin-corrected serum calcium value of less than 7 mg/dL (5.0% versus 17% for previous treatment with placebo and [[Parathyroid hormone]] ([[Injection]]) respectively). | ||
* Twenty subjects (24%) previously randomized to | * Twenty subjects (24%) previously randomized to [[Parathyroid hormone]] ([[Injection]]) experienced adverse reactions of hypocalcemia in the post-treatment phase compared to three subjects (8%) previously randomized to placebo. | ||
* Five subjects previously randomized to | * Five subjects previously randomized to [[Parathyroid hormone]] ([[Injection]]) with albumin-corrected serum calcium below 7 mg/dL required treatment with IV [[calcium gluconate]] to correct [[hypocalcemia]]. | ||
==== Hypercalciuria ==== | ==== Hypercalciuria ==== | ||
* Treatment with | * Treatment with [[Parathyroid hormone]] ([[Injection]]) did not lower 24-hour urinary calcium excretion in the placebo-controlled trial. | ||
* The proportion of subjects with [[hypercalciuria]] (defined as urine calcium levels of >300 mg/24 hours) was similar at baseline and trial end in the | * The proportion of subjects with [[hypercalciuria]] (defined as urine calcium levels of >300 mg/24 hours) was similar at baseline and trial end in the [[Parathyroid hormone]] ([[Injection]]) and placebo groups. | ||
* The median (IQR) 24-hour Urine Calcium at trial end was similar between NATPARA [231 (168-351) mg/24 hours], and placebo [232 (139-342) mg/24 hours]. | * The median (IQR) 24-hour Urine Calcium at trial end was similar between NATPARA [231 (168-351) mg/24 hours], and placebo [232 (139-342) mg/24 hours]. | ||
* At trial end, serum calcium values between | * At trial end, serum calcium values between [[Parathyroid hormone]] ([[Injection]]) and placebo were also similar. | ||
* Risk of hypercalciuria throughout the trial was related to serum calcium levels. | * Risk of hypercalciuria throughout the trial was related to serum calcium levels. | ||
* To minimize the risk of hypercalciuria, | * To minimize the risk of hypercalciuria, [[Parathyroid hormone]] ([[Injection]]) should be dosed to a target albumin-corrected total serum calcium within the lower half of the normal range (i.e., between 8 and 9 mg/dL). | ||
=== Immunogenicity === | === Immunogenicity === | ||
* | * [[Parathyroid hormone]] ([[Injection]]) may trigger the development of antibodies. | ||
* In the placebo-controlled study in adults with hypoparathyroidism, the incidence of anti-PTH antibodies was 8.6% (3/35) and 5.9% (1/17) in subjects who received subcutaneous administration of 50 to 100 mcg | * In the placebo-controlled study in adults with hypoparathyroidism, the incidence of anti-PTH antibodies was 8.6% (3/35) and 5.9% (1/17) in subjects who received subcutaneous administration of 50 to 100 mcg [[Parathyroid hormone]] ([[Injection]]) or placebo once daily for 24 weeks, respectively. | ||
* Across all clinical studies in subjects with hypoparathyroidism following treatment with | * Across all clinical studies in subjects with hypoparathyroidism following treatment with [[Parathyroid hormone]] ([[Injection]]) for up to 2.6 years, the immunogenicity incidence rate was 16.1% (14/87). | ||
* These 14 subjects had low titer anti-PTH antibodies and, of these, 3 subjects subsequently became antibody negative. | * These 14 subjects had low titer anti-PTH antibodies and, of these, 3 subjects subsequently became antibody negative. | ||
* One of these subjects had antibodies with neutralizing activity; this subject maintained a clinical response with no evidence of immune-related adverse reactions. | * One of these subjects had antibodies with neutralizing activity; this subject maintained a clinical response with no evidence of immune-related adverse reactions. | ||
* Anti-PTH antibodies did not appear to affect efficacy or safety during the clinical trials but their longer-term impact is unknown. | * Anti-PTH antibodies did not appear to affect efficacy or safety during the clinical trials but their longer-term impact is unknown. | ||
* Immunogenicity assay results are highly dependent on the sensitivity and specificity of the assay and may be influenced by several factors such as: assay methodology, sample handling, timing of sample collection, concomitant medication, and underlying diseases. | * Immunogenicity assay results are highly dependent on the sensitivity and specificity of the assay and may be influenced by several factors such as: assay methodology, sample handling, timing of sample collection, concomitant medication, and underlying diseases. | ||
* For these reasons, comparison of the incidence of antibodies to | * For these reasons, comparison of the incidence of antibodies to [[Parathyroid hormone]] ([[Injection]]) with the incidence of antibodies to other products may be misleading. | ||
|drugInteractions===== Alendronate ==== | |drugInteractions===== Alendronate ==== | ||
* Co-administration of [[alendronate]] and | * Co-administration of [[alendronate]] and [[Parathyroid hormone]] ([[Injection]]) leads to reduction in the calcium-sparing effect, which can interfere with the normalization of serum calcium. | ||
* Concomitant use of | * Concomitant use of [[Parathyroid hormone]] ([[Injection]]) with alendronate is not recommended. | ||
==== Digoxin ==== | ==== Digoxin ==== | ||
* | * [[Parathyroid hormone]] ([[Injection]]) causes transient increase in calcium and therefore, concomitant use of [[Parathyroid hormone]] ([[Injection]]) and [[cardiac glycosides]] (e.g., digoxin) may predispose patients to digitalis toxicity if hypercalcemia develops. | ||
* Digoxin efficacy is reduced if hypocalcemia is present. | * Digoxin efficacy is reduced if hypocalcemia is present. | ||
* In patients using | * In patients using [[Parathyroid hormone]] ([[Injection]]) concomitantly with digoxin, carefully monitor serum calcium and digoxin levels, and patients for signs and symptoms of [[digoxin]] toxicity. | ||
* Adjustment of digoxin and/or | * Adjustment of digoxin and/or [[Parathyroid hormone]] ([[Injection]]) may be needed. | ||
* No drug-drug interaction study has been conducted with digoxin and | * No drug-drug interaction study has been conducted with digoxin and [[Parathyroid hormone]] ([[Injection]]). | ||
|useInPregnancyFDA=* Developmental effects were observed in a peri-/post-natal study in pregnant rats given subcutaneous doses of 100, 300, 1000 mcg/kg/day from organogenesis through lactation, while entire stillborn litters were observed in the 300 mcg/kg/day group (34 times the 100 mcg/day clinical dose based on AUC). | |useInPregnancyFDA=* Developmental effects were observed in a peri-/post-natal study in pregnant rats given subcutaneous doses of 100, 300, 1000 mcg/kg/day from organogenesis through lactation, while entire stillborn litters were observed in the 300 mcg/kg/day group (34 times the 100 mcg/day clinical dose based on AUC). | ||
* Increased incidence of morbidity associated with [[dehydration]], broken [[palate]] and palate injuries related to incisor misalignment and mortality were found in pups from litters given 100 mcg/kg/day (10 times the 100 mcg/day clinical dose based on AUC). | * Increased incidence of morbidity associated with [[dehydration]], broken [[palate]] and palate injuries related to incisor misalignment and mortality were found in pups from litters given 100 mcg/kg/day (10 times the 100 mcg/day clinical dose based on AUC). | ||
* Because animal reproduction studies are not always predictive of human response, | * Because animal reproduction studies are not always predictive of human response, [[Parathyroid hormone]] ([[Injection]]) should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. | ||
|useInNursing=* It is unknown whether | |useInNursing=* It is unknown whether [[Parathyroid hormone]] ([[Injection]]) is excreted in human milk. * In rats, mean parathyroid hormone concentration in milk was approximately 10 ng/mL at a dose of 1000 mcg/kg/day, 42 times lower in milk than in plasma. | ||
* For nursing mothers, consideration should be made whether discontinuing nursing or | * For nursing mothers, consideration should be made whether discontinuing nursing or [[Parathyroid hormone]] ([[Injection]]) is warranted, taking into account the importance of the drug to the mother. | ||
|useInPed=* Safety and efficacy in patients less than 18 years of age has not been established. | |useInPed=* Safety and efficacy in patients less than 18 years of age has not been established. | ||
* Avoid use of | * Avoid use of [[Parathyroid hormone]] ([[Injection]]) in patients who are at increased baseline risk for [[osteosarcoma]] including pediatric and young adult patients with open epiphyses. | ||
|useInGeri=* Clinical studies of | |useInGeri=* Clinical studies of [[Parathyroid hormone]] ([[Injection]]) did not include sufficient numbers of subjects aged 65 and over to determine whether response in these subjects is different from younger subjects. | ||
* In general, dose selection for elderly individuals should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. | * In general, dose selection for elderly individuals should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. | ||
|useInRenalImpair=* Clinical studies of | |useInRenalImpair=* Clinical studies of [[Parathyroid hormone]] ([[Injection]]) did not include sufficient numbers of subjects with moderate and severe renal impairment to determine whether they respond differently from subjects with mild renal impairment or normal renal function. | ||
* Some of the mechanisms of action of | * Some of the mechanisms of action of [[Parathyroid hormone]] ([[Injection]]) (e.g., conversion of 25-OH vitamin D to 1,25-OH2 vitamin D) are dependent on renal function. | ||
* | * [[Parathyroid hormone]] ([[Injection]]) is eliminated by the kidney and maximum drug levels increased with renal impairment. | ||
|overdose=* Accidental overdose in studies in hypoparathyroidism occurred in 1 subject who received a 150 mcg dose and experienced mild palpitations. | |overdose=* Accidental overdose in studies in hypoparathyroidism occurred in 1 subject who received a 150 mcg dose and experienced mild palpitations. | ||
* Serum calcium 24 hours later was 10.3 mg/dL. | * Serum calcium 24 hours later was 10.3 mg/dL. | ||
* In the event of overdose, the patient should be carefully monitored for hypercalcemia by a medical professional. | * In the event of overdose, the patient should be carefully monitored for hypercalcemia by a medical professional. | ||
|mechAction=* | |mechAction=* [[Parathyroid hormone]] ([[Injection]]) is a parathyroid hormone. | ||
* Parathyroid hormone raises serum calcium by increasing renal tubular calcium reabsorption, increasing intestinal calcium absorption (i.e., by converting 25-OH vitamin D to 1,25-OH2 vitamin D) and by increasing bone turnover which releases calcium into the circulation. | * Parathyroid hormone raises serum calcium by increasing renal tubular calcium reabsorption, increasing intestinal calcium absorption (i.e., by converting 25-OH vitamin D to 1,25-OH2 vitamin D) and by increasing bone turnover which releases calcium into the circulation. | ||
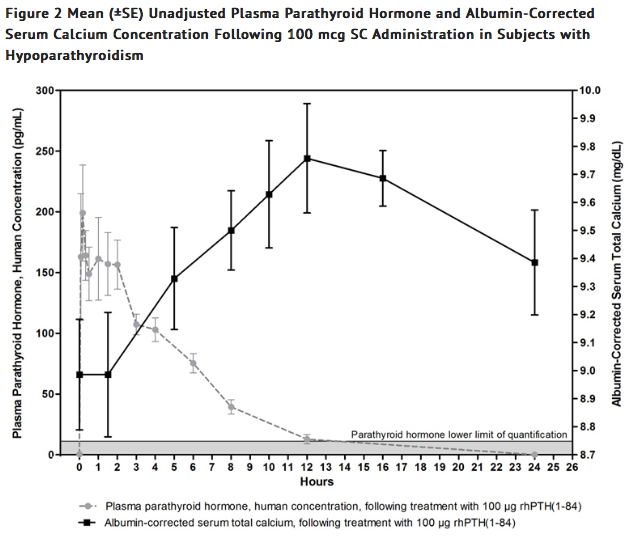
|PD=* The pharmacodynamics in subjects with hypoparathyroidism after single subcutaneous administration of 50 and 100 mcg dose of | |PD=* The pharmacodynamics in subjects with hypoparathyroidism after single subcutaneous administration of 50 and 100 mcg dose of [[Parathyroid hormone]] ([[Injection]]) in the thigh were evaluated. | ||
* Treatment with | * Treatment with [[Parathyroid hormone]] ([[Injection]]) increases serum calcium levels (Figure 2). | ||
* The increase in serum calcium levels in [[hypoparathyroidism]] subjects occurs in a dose-related manner. | * The increase in serum calcium levels in [[hypoparathyroidism]] subjects occurs in a dose-related manner. | ||
* Mean peak serum calcium levels are reached between 10 and 12 hours following a single [[subcutaneous]] injection and the increase in serum calcium above baseline is sustained for more than 24 hours after administration. | * Mean peak serum calcium levels are reached between 10 and 12 hours following a single [[subcutaneous]] injection and the increase in serum calcium above baseline is sustained for more than 24 hours after administration. | ||
* The maximum mean increases of serum calcium, which occurred at 12 hours, were approximately 0.5 mg/dL and 0.7 mg/dL from baseline with the 50 mcg and 100 mcg doses, respectively. | * The maximum mean increases of serum calcium, which occurred at 12 hours, were approximately 0.5 mg/dL and 0.7 mg/dL from baseline with the 50 mcg and 100 mcg doses, respectively. | ||
* The mean calcium intake for the 50 and 100 mcg doses was 1700 mg. | * The mean calcium intake for the 50 and 100 mcg doses was 1700 mg. | ||
|PK=* Following single [[subcutaneous]] injections of | |PK=* Following single [[subcutaneous]] injections of [[Parathyroid hormone]] ([[Injection]]) at 50 mcg and 100 mcg in subjects with [[hypoparathyroidism]], peak plasma concentrations (mean Tmax) of [[Parathyroid hormone]] ([[Injection]]) occurs within 5 to 30 minutes and a second usually smaller peak at 1 to 2 hours. | ||
* The plasma AUC increased in a dose-proportional manner from 50 mcg to 100 mcg. | * The plasma AUC increased in a dose-proportional manner from 50 mcg to 100 mcg. | ||
* The apparent terminal half-life (t1/2) was 3.02 and 2.83 hours for the 50 and 100 mcg dose, respectively. | * The apparent terminal half-life (t1/2) was 3.02 and 2.83 hours for the 50 and 100 mcg dose, respectively. | ||
* Mean unadjusted concentration-time profiles of parathyroid hormone in plasma following SC administration of 100 mcg of | * Mean unadjusted concentration-time profiles of parathyroid hormone in plasma following SC administration of 100 mcg of [[Parathyroid hormone]] ([[Injection]]) are presented in Figure 2. | ||
* One 100 mcg dose of | * One 100 mcg dose of [[Parathyroid hormone]] ([[Injection]]) provides a 24-hour calcemic response in [[hypoparathyroidism]] subjects. | ||
[[File:Parathyroid.png|thumb|center]] | [[File:Parathyroid.png|thumb|center]] | ||
|alcohol=Alcohol-Parathyroid hormone (Injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |alcohol=Alcohol-Parathyroid hormone (Injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | ||
}} | }} | ||
Revision as of 18:30, 27 February 2017
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Shivani Chaparala M.B.B.S [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING
See full prescribing information for complete Boxed Warning.
POTENTIAL RISK OF OSTEOSARCOMA:
|
Overview
Parathyroid hormone (injection) is a parathyroid hormone that is FDA approved for the treatment of hypocalcemia in patients with hypoparathyroidism, as an adjunct to calcium and vitamin D.. There is a Black Box Warning for this drug as shown here. Common adverse reactions include * Paresthesia
- Hypocalcemia
- Headache
- Hypercalcemia
- Nausea
- Hypoaesthesia
- Diarrhea
- Vomiting
- Arthralgia
- Hypercalciuria and
- Pain in extremity..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
INDICATIONS AND USAGE
Parathyroid hormone (Injection) is a parathyroid hormone indicated as an adjunct to calcium and vitamin D to control hypocalcemia in patients with hypoparathyroidism.
Limitations of Use
- Because of the potential risk of osteosarcoma, Parathyroid hormone (Injection) is recommended only for patients who cannot be well-controlled on calcium supplements and active forms of vitamin D alone.
- Parathyroid hormone (Injection) was not studied in patients with hypoparathyroidism caused by calcium-sensing receptor mutations.
- Parathyroid hormone (Injection) was not studied in patients with acute post-surgical hypoparathyroidism.
DOSAGE AND ADMINISTRATION
- The dose of Parathyroid hormone (Injection) should be individualized to achieve a serum calcium level in the lower half of the normal range.
- Confirm vitamin D stores are sufficient and serum calcium is above 7.5 mg/dL before starting Parathyroid hormone (Injection).
- The starting dose of Parathyroid hormone (Injection) is 50 mcg injected once daily in the thigh. When starting Parathyroid hormone (Injection), decrease dose of active vitamin D by 50%, if serum calcium is above 7.5 mg/dL.
- Monitor serum calcium levels every 3 to 7 days after starting or adjusting Parathyroid hormone (Injection) dose and when adjusting either active vitamin D or calcium supplements dose while using Parathyroid hormone (Injection).
DOSAGE FORMS AND STRENGTHS
- Parathyroid hormone (Injection) is supplied as a multiple-dose, dual-chamber glass cartridge containing a sterile lyophilized powder and a sterile diluent for reconstitution in four dosage strengths.
- For injection: 25 mcg, 50 mcg, 75 mcg, or 100 mcg.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Parathyroid hormone (Injection) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Parathyroid hormone (Injection) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Parathyroid hormone (injection) FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Parathyroid hormone (Injection) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Parathyroid hormone (Injection) in pediatric patients.
Contraindications
There is limited information regarding Parathyroid hormone (injection) Contraindications in the drug label.
Warnings
|
WARNING
See full prescribing information for complete Boxed Warning.
POTENTIAL RISK OF OSTEOSARCOMA:
|
Potential Risk of Osteosarcoma
- In male and female rats, parathyroid hormone caused an increase in the incidence of osteosarcoma (a malignant bone tumor).
- The occurrence of osteosarcoma was observed to be dependent on parathyroid hormone dose and treatment duration.
- This effect was observed at parathyroid hormone exposure levels ranging from 3 to 71 times the exposure levels for humans receiving a 100 mcg dose of Parathyroid hormone (Injection).
- These data could not exclude a risk to humans.
- Because of a potential risk of osteosarcoma, use Parathyroid hormone (Injection) only in patients who cannot be well-controlled on calcium supplements and active forms of vitamin D alone and for whom the potential benefits are considered to outweigh this potential risk.
- To further mitigate the potential risk of osteosarcoma, avoid use of Parathyroid hormone (Injection) in patients who are at increased risk for osteosarcoma, such as patients with Paget's disease of bone or unexplained elevations of alkaline phosphatase, pediatric and young adult patients with open epiphyses, patients with hereditary disorders predisposing to osteosarcoma, or patients with a prior history of external beam or implant radiation therapy involving the skeleton.
- Instruct patients to promptly report clinical symptoms (e.g., persistent localized pain) and signs (e.g., soft tissue mass tender to palpation) that could be consistent with osteosarcoma.
- Parathyroid hormone (Injection) is available only through a restricted program under a REMS.
Parathyroid hormone (Injection) REMS Program
- Because of the potential risk of osteosarcoma associated with Parathyroid hormone (Injection) therapy, Parathyroid hormone (Injection) is available only through a restricted REMS program called the NATPARA REMS Program.
- Under the Parathyroid hormone (Injection) REMS Program, only certified healthcare providers can prescribe and only certified pharmacies can dispense Parathyroid hormone (Injection).
Hypercalcemia
- Severe hypercalcemia has been reported with Parathyroid hormone (Injection).
- In the pivotal trial, 3 patients randomized to Parathyroid hormone (Injection) required administration of IV fluids to correct hypercalcemia during treatment with Parathyroid hormone (Injection).
- The risk is highest when starting or increasing the dose of Parathyroid hormone (Injection), but can occur at any time.
- Monitor serum calcium and patients for signs and symptoms of hypercalcemia.
- Treat hypercalcemia per standard practice and consider holding and/or lowering the dose of Parathyroid hormone (Injection) if severe hypercalcemia occurs.
Hypocalcemia
- Severe hypocalcemia has been reported with Parathyroid hormone (Injection).
- The risk is highest when Parathyroid hormone (Injection) is withheld, missed or abruptly discontinued, but can occur at any time.
- Monitor serum calcium and patients for signs and symptoms of hypocalcemia.
- Resume treatment with, or increase the dose of, an active form of vitamin D or calcium supplements or both if indicated in patients interrupting or discontinuing Parathyroid hormone (Injection) to prevent severe hypocalcemia.
Risk of Digoxin Toxicity with Concomitant Use of Digitalis Compounds
- The inotropic effects of digoxin are affected by serum calcium levels.
- Hypercalcemia of any cause may predispose to digoxin toxicity.
- In patients using Parathyroid hormone (Injection) concomitantly with digitalis compounds, monitor serum calcium and digoxin levels and patients for signs and symptoms of digitalis toxicity.
- Adjustment of digoxin and/or Parathyroid hormone (Injection) may be needed.
- No drug-drug interaction study has been conducted with digoxin and Parathyroid hormone (Injection).
Adverse Reactions
Clinical Trials Experience
Adverse Reactions in Clinical Trials for Hypoparathyroidism
- Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other clinical trials and may not reflect the rates observed in clinical practice.
- Parathyroid hormone (Injection) was studied in a placebo-controlled trial.
- The data described in Table 1 below reflect exposure to Parathyroid hormone (Injection) in 84 patients, including 78 exposed for 24 weeks.
- The mean age of the trial population was 47 years and ranged from 19 to 74 years old.
- Seventy-nine percent (79%) were females.
- Ninety-six percent (96%) were Caucasian, 0.8% were Black, and 1.6% were Asian.
- Patients had had hypoparathyroidism for on average 15 years and hypoparathyroidism was caused by post-surgical complications in 71% of cases, idiopathic hypoparathyroidism in 25% of cases, DiGeorge Syndrome in 3% of cases, and auto-immune hypoparathyroidism in 1% of cases.
- Prior to trial enrollment, participants were receiving a median (interquartile range) daily oral calcium dose of 2000 (1250, 3000) mg and a median daily oral active vitamin D dose equivalent to 0.75 (0.5, 1) mcg of calcitriol.
- The mean eGFR at baseline was 97.4 mL/min/1.73 m2 and 45%, 10% and 0% had mild, moderate and severe renal impairment, respectively, at baseline.
- During the trial, most patients received 100 mcg and the dose range was 50 to 100 mcg administered subcutaneously once daily in the thigh.
- Table 1 lists common adverse reactions associated with Parathyroid hormone (Injection) use in the clinical trial.
- Common adverse reactions were reactions that occurred in ≥5% of subjects and occurred more commonly on Parathyroid hormone (Injection) than on placebo.
TABLE 1:
Hypercalcemia
- In the overall pivotal trial a greater proportion of patients on Parathyroid hormone (Injection) had albumin-corrected serum calcium above the normal range (8.4 to 10.6 mg/dL).
- During the entire trial duration 3 patients on Parathyroid hormone (Injection) and 1 patient on placebo had a calcium level above 12 mg/dL.
- Table 2 displays the number of subjects who had albumin-corrected serum calcium levels above the normal range (8.4 to 10.6 mg/dL) by study treatment period in the placebo-controlled study based on routine monitoring at each trial visit.
- More patients randomized to Parathyroid hormone (Injection) had hypercalcemia in both phases of the study (note: all trial participants underwent a 50% reduction in active vitamin D dose at randomization).
Table 2
Hypocalcemia
- Table 3 displays the number of subjects who had albumin-corrected serum calcium levels below 8.4 mg/dL by treatment period in the placebo-controlled study based on routine monitoring at each trial visit.
- More patients randomized to placebo had hypocalcemia of less than 7 mg/dL in the titration phase (note: all trial participants underwent a 50% reduction in active vitamin D dose at randomization).
- More patients randomized to Parathyroid hormone (Injection) had hypocalcemia of less than 7 mg/dL in the dose maintenance phase.
Table 3:
- The risk of hypocalcemia increases when Parathyroid hormone (Injection) is withdrawn.
- At the end of the trial, Parathyroid hormone (Injection) and placebo were withdrawn, calcium and active vitamin D were returned to baseline doses and subjects were followed for 4 weeks.
- During this withdrawal phase, more patients previously randomized to Parathyroid hormone (Injection) experienced an albumin-corrected serum calcium value of less than 7 mg/dL (5.0% versus 17% for previous treatment with placebo and Parathyroid hormone (Injection) respectively).
- Twenty subjects (24%) previously randomized to Parathyroid hormone (Injection) experienced adverse reactions of hypocalcemia in the post-treatment phase compared to three subjects (8%) previously randomized to placebo.
- Five subjects previously randomized to Parathyroid hormone (Injection) with albumin-corrected serum calcium below 7 mg/dL required treatment with IV calcium gluconate to correct hypocalcemia.
Hypercalciuria
- Treatment with Parathyroid hormone (Injection) did not lower 24-hour urinary calcium excretion in the placebo-controlled trial.
- The proportion of subjects with hypercalciuria (defined as urine calcium levels of >300 mg/24 hours) was similar at baseline and trial end in the Parathyroid hormone (Injection) and placebo groups.
- The median (IQR) 24-hour Urine Calcium at trial end was similar between NATPARA [231 (168-351) mg/24 hours], and placebo [232 (139-342) mg/24 hours].
- At trial end, serum calcium values between Parathyroid hormone (Injection) and placebo were also similar.
- Risk of hypercalciuria throughout the trial was related to serum calcium levels.
- To minimize the risk of hypercalciuria, Parathyroid hormone (Injection) should be dosed to a target albumin-corrected total serum calcium within the lower half of the normal range (i.e., between 8 and 9 mg/dL).
Immunogenicity
- Parathyroid hormone (Injection) may trigger the development of antibodies.
- In the placebo-controlled study in adults with hypoparathyroidism, the incidence of anti-PTH antibodies was 8.6% (3/35) and 5.9% (1/17) in subjects who received subcutaneous administration of 50 to 100 mcg Parathyroid hormone (Injection) or placebo once daily for 24 weeks, respectively.
- Across all clinical studies in subjects with hypoparathyroidism following treatment with Parathyroid hormone (Injection) for up to 2.6 years, the immunogenicity incidence rate was 16.1% (14/87).
- These 14 subjects had low titer anti-PTH antibodies and, of these, 3 subjects subsequently became antibody negative.
- One of these subjects had antibodies with neutralizing activity; this subject maintained a clinical response with no evidence of immune-related adverse reactions.
- Anti-PTH antibodies did not appear to affect efficacy or safety during the clinical trials but their longer-term impact is unknown.
- Immunogenicity assay results are highly dependent on the sensitivity and specificity of the assay and may be influenced by several factors such as: assay methodology, sample handling, timing of sample collection, concomitant medication, and underlying diseases.
- For these reasons, comparison of the incidence of antibodies to Parathyroid hormone (Injection) with the incidence of antibodies to other products may be misleading.
Postmarketing Experience
There is limited information regarding Parathyroid hormone (injection) Postmarketing Experience in the drug label.
Drug Interactions
Alendronate
- Co-administration of alendronate and Parathyroid hormone (Injection) leads to reduction in the calcium-sparing effect, which can interfere with the normalization of serum calcium.
- Concomitant use of Parathyroid hormone (Injection) with alendronate is not recommended.
Digoxin
- Parathyroid hormone (Injection) causes transient increase in calcium and therefore, concomitant use of Parathyroid hormone (Injection) and cardiac glycosides (e.g., digoxin) may predispose patients to digitalis toxicity if hypercalcemia develops.
- Digoxin efficacy is reduced if hypocalcemia is present.
- In patients using Parathyroid hormone (Injection) concomitantly with digoxin, carefully monitor serum calcium and digoxin levels, and patients for signs and symptoms of digoxin toxicity.
- Adjustment of digoxin and/or Parathyroid hormone (Injection) may be needed.
- No drug-drug interaction study has been conducted with digoxin and Parathyroid hormone (Injection).
Use in Specific Populations
Pregnancy
- Developmental effects were observed in a peri-/post-natal study in pregnant rats given subcutaneous doses of 100, 300, 1000 mcg/kg/day from organogenesis through lactation, while entire stillborn litters were observed in the 300 mcg/kg/day group (34 times the 100 mcg/day clinical dose based on AUC).
- Increased incidence of morbidity associated with dehydration, broken palate and palate injuries related to incisor misalignment and mortality were found in pups from litters given 100 mcg/kg/day (10 times the 100 mcg/day clinical dose based on AUC).
- Because animal reproduction studies are not always predictive of human response, Parathyroid hormone (Injection) should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Parathyroid hormone (injection) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Parathyroid hormone (injection) during labor and delivery.
Nursing Mothers
- It is unknown whether Parathyroid hormone (Injection) is excreted in human milk. * In rats, mean parathyroid hormone concentration in milk was approximately 10 ng/mL at a dose of 1000 mcg/kg/day, 42 times lower in milk than in plasma.
- For nursing mothers, consideration should be made whether discontinuing nursing or Parathyroid hormone (Injection) is warranted, taking into account the importance of the drug to the mother.
Pediatric Use
- Safety and efficacy in patients less than 18 years of age has not been established.
- Avoid use of Parathyroid hormone (Injection) in patients who are at increased baseline risk for osteosarcoma including pediatric and young adult patients with open epiphyses.
Geriatic Use
- Clinical studies of Parathyroid hormone (Injection) did not include sufficient numbers of subjects aged 65 and over to determine whether response in these subjects is different from younger subjects.
- In general, dose selection for elderly individuals should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Gender
There is no FDA guidance on the use of Parathyroid hormone (injection) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Parathyroid hormone (injection) with respect to specific racial populations.
Renal Impairment
- Clinical studies of Parathyroid hormone (Injection) did not include sufficient numbers of subjects with moderate and severe renal impairment to determine whether they respond differently from subjects with mild renal impairment or normal renal function.
- Some of the mechanisms of action of Parathyroid hormone (Injection) (e.g., conversion of 25-OH vitamin D to 1,25-OH2 vitamin D) are dependent on renal function.
- Parathyroid hormone (Injection) is eliminated by the kidney and maximum drug levels increased with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Parathyroid hormone (injection) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Parathyroid hormone (injection) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Parathyroid hormone (injection) in patients who are immunocompromised.
Administration and Monitoring
Administration
There is limited information regarding Parathyroid hormone (injection) Administration in the drug label.
Monitoring
There is limited information regarding Parathyroid hormone (injection) Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Parathyroid hormone (injection) and IV administrations.
Overdosage
- Accidental overdose in studies in hypoparathyroidism occurred in 1 subject who received a 150 mcg dose and experienced mild palpitations.
- Serum calcium 24 hours later was 10.3 mg/dL.
- In the event of overdose, the patient should be carefully monitored for hypercalcemia by a medical professional.
Pharmacology
There is limited information regarding Parathyroid hormone (injection) Pharmacology in the drug label.
Mechanism of Action
- Parathyroid hormone (Injection) is a parathyroid hormone.
- Parathyroid hormone raises serum calcium by increasing renal tubular calcium reabsorption, increasing intestinal calcium absorption (i.e., by converting 25-OH vitamin D to 1,25-OH2 vitamin D) and by increasing bone turnover which releases calcium into the circulation.
Structure
There is limited information regarding Parathyroid hormone (injection) Structure in the drug label.
Pharmacodynamics
- The pharmacodynamics in subjects with hypoparathyroidism after single subcutaneous administration of 50 and 100 mcg dose of Parathyroid hormone (Injection) in the thigh were evaluated.
- Treatment with Parathyroid hormone (Injection) increases serum calcium levels (Figure 2).
- The increase in serum calcium levels in hypoparathyroidism subjects occurs in a dose-related manner.
- Mean peak serum calcium levels are reached between 10 and 12 hours following a single subcutaneous injection and the increase in serum calcium above baseline is sustained for more than 24 hours after administration.
- The maximum mean increases of serum calcium, which occurred at 12 hours, were approximately 0.5 mg/dL and 0.7 mg/dL from baseline with the 50 mcg and 100 mcg doses, respectively.
- The mean calcium intake for the 50 and 100 mcg doses was 1700 mg.
Pharmacokinetics
- Following single subcutaneous injections of Parathyroid hormone (Injection) at 50 mcg and 100 mcg in subjects with hypoparathyroidism, peak plasma concentrations (mean Tmax) of Parathyroid hormone (Injection) occurs within 5 to 30 minutes and a second usually smaller peak at 1 to 2 hours.
- The plasma AUC increased in a dose-proportional manner from 50 mcg to 100 mcg.
- The apparent terminal half-life (t1/2) was 3.02 and 2.83 hours for the 50 and 100 mcg dose, respectively.
- Mean unadjusted concentration-time profiles of parathyroid hormone in plasma following SC administration of 100 mcg of Parathyroid hormone (Injection) are presented in Figure 2.
- One 100 mcg dose of Parathyroid hormone (Injection) provides a 24-hour calcemic response in hypoparathyroidism subjects.
Nonclinical Toxicology
There is limited information regarding Parathyroid hormone (injection) Nonclinical Toxicology in the drug label.
Clinical Studies
There is limited information regarding Parathyroid hormone (injection) Clinical Studies in the drug label.
How Supplied
There is limited information regarding Parathyroid hormone (injection) How Supplied in the drug label.
Storage
There is limited information regarding Parathyroid hormone (injection) Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Parathyroid hormone (injection) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Parathyroid hormone (injection) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Parathyroid hormone (injection) Patient Counseling Information in the drug label.
Precautions with Alcohol
Alcohol-Parathyroid hormone (Injection) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Parathyroid hormone (injection) Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Parathyroid hormone (injection) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.