Esophageal stricture: Difference between revisions
No edit summary |
|||
| Line 15: | Line 15: | ||
'''For patient information, click [[Esophageal stricture (patient information)|here]]''' | '''For patient information, click [[Esophageal stricture (patient information)|here]]''' | ||
{{CMG}}; {{AE}}{{MA}} | {{CMG}}; {{AE}}{{MA}} [mailto:malihash@bidmc.harvard.edu] | ||
==[[Esophageal stricture overview|Overview]]== | ==[[Esophageal stricture overview|Overview]]== | ||
==[[Esophageal stricture historical perspective|Historical Perspective]]== | ==[[Esophageal stricture historical perspective|Historical Perspective]]== | ||
First intervention for esophaegal stricture was done in the 17 century by whalebone. The first bougienage was performed in 1801. In 1868, esophagoscope was developed for the first time. In 1877, first surgical [[resection]] for esophaegal [[carcinoma]] was performed by Vincenz Czerny. First stent was introduced in 1990. | |||
==[[Esophageal stricture classification|Classification]]== | ==[[Esophageal stricture classification|Classification]]== | ||
There is no established system for the classification of [[esophageal]] [[stricture]], but it may be classified into [[benign]] and [[malignant]] according to causes. | |||
==[[Esophageal stricture pathophysiology|Pathophysiology]]== | ==[[Esophageal stricture pathophysiology|Pathophysiology]]== | ||
It is thought that [[esophageal]] [[stricture]] is the result of lower pressure of [[esophageal sphincter]] in [[gastroesophageal reflux disease]], esophageal motor disorder, [[inflammation]] and [[fibrosis]] in [[neoplasia]]. The most characteristic finding in [[gross pathology]] is thickening of the lower [[esophageal]] wall in [[gastroesophageal reflux disease]], pale [[mucosa]] in [[lymphocytic]] [[esophagitis]] and [[hemorrhagic]] [[congestion]] in [[caustic]] ingestion. | |||
[[Microscopic]] [[histopathological]] characteristic findings of [[esophageal]] [[stricture]] is inntraepithelial [[lymphocytes]] and [[basal cell]] [[hyperplasia]] in [[gastroesophageal reflux disease]], [[Infiltration (medical)|infiltration]] T [[lymphocytes]] in [[squamous]] [[mucosa]] in [[lymphocytic]] [[esophagitis]] and [[eosinophilic]] [[necrosis]] in [[caustic]] ingestion | |||
==[[Esophageal stricture causes|Causes]]== | ==[[Esophageal stricture causes|Causes]]== | ||
Common causes of [[esophageal]] [[stricture]] include [[gastroesophageal reflux disease]] and [[caustic]] ingestions. | |||
==[[Esophageal stricture differential diagnosis|Differentiating Esophageal stricture from other Disorders]]== | ==[[Esophageal stricture differential diagnosis|Differentiating Esophageal stricture from other Disorders]]== | ||
Esophageal stricture must be differentiated from plummer-vinson syndrome, [[achalasia]] , [[diffuse esophageal spasm]], [[systemic sclerosis]], [[zenker's diverticulum]], [[Esophageal cancer|esophageal carcinoma]], [[stroke]], motor disorders, [[GERD]][[Esophageal web|, esophageal web]]. | |||
==[[Esophageal stricture epidemiology and demographics|Epidemiology and Demographics]]== | ==[[Esophageal stricture epidemiology and demographics|Epidemiology and Demographics]]== | ||
Most of [[esophageal]] [[strictures]] are related to [[gastroesophageal reflux disease]]. Overall incidence of [[esophageal stricture]] is approximately 11 per 100,000 individuals and the [[prevalence]] of [[esophageal]][[stricture]] is approximately 70-120 per 100,000 individuals in united states. The [[incidence]] of [[esophageal]] [[stricture]] increases with age. There is no racial predilection to [[esophageal]] [[stricture]]. The risk of [[esophageal]] [[stricture]] is higher in men under 60 yr but there is similar [[incidence]] in men and women after age 60. | |||
==[[Esophageal stricture risk factors|Risk Factors]]== | ==[[Esophageal stricture risk factors|Risk Factors]]== | ||
The most potent [[risk factor]] in the development of [[esophageal]] [[stricture]] is frequent [[acid reflux]]. Other [[risk factor]]<nowiki/>s include [[Hiatus hernia|hiatal hernia]], [[obesity]], [[smoking]], [[esophageal dysmotility]], increased [[gastric]] acidity, and heavy [[alcohol]] use. | |||
==[[Esophageal stricture natural history, complications and prognosis|Natural History, Complications, and Prognosis]]== | ==[[Esophageal stricture natural history, complications and prognosis|Natural History, Complications, and Prognosis]]== | ||
If left untreated, patients with [[esophageal]] [[stricture]] may progress to develop [[pulmonary aspiration]], [[weight loss]], and [[dehydration]]. Common [[complication]]<nowiki/>s of [[esophageal]] [[stricture]] include [[perforation]], [[bleeding]], [[pneumonia]], [[bacteremia]]. [[Prognosis]] is generally good but recurrence of symptoms after [[dilation]] are prevalent and usually recurrent [[dilation]] is necessary. | |||
==Diagnosis== | ==Diagnosis== | ||
| Line 48: | Line 58: | ||
* [[Esophageal cancer]] | * [[Esophageal cancer]] | ||
* [[Esophagitis]] | * [[Esophagitis]] | ||
[[Category:Gastroenterology]] | [[Category:Gastroenterology]] | ||
Revision as of 15:26, 22 November 2017
| Esophageal stricture | |
 | |
|---|---|
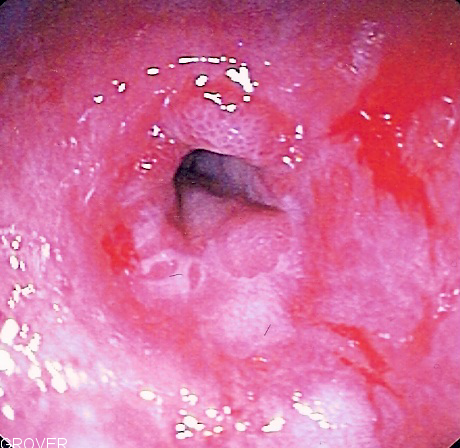
| Endoscopic image of a benign peptic stricture | |
| ICD-9 | 530.3 |
| DiseasesDB | 31502 |
| MedlinePlus | 000207 |
|
Esophageal stricture Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Esophageal stricture On the Web |
|
American Roentgen Ray Society Images of Esophageal stricture |
For patient information, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mahda Alihashemi M.D. [2] [3]
Overview
Historical Perspective
First intervention for esophaegal stricture was done in the 17 century by whalebone. The first bougienage was performed in 1801. In 1868, esophagoscope was developed for the first time. In 1877, first surgical resection for esophaegal carcinoma was performed by Vincenz Czerny. First stent was introduced in 1990.
Classification
There is no established system for the classification of esophageal stricture, but it may be classified into benign and malignant according to causes.
Pathophysiology
It is thought that esophageal stricture is the result of lower pressure of esophageal sphincter in gastroesophageal reflux disease, esophageal motor disorder, inflammation and fibrosis in neoplasia. The most characteristic finding in gross pathology is thickening of the lower esophageal wall in gastroesophageal reflux disease, pale mucosa in lymphocytic esophagitis and hemorrhagic congestion in caustic ingestion.
Microscopic histopathological characteristic findings of esophageal stricture is inntraepithelial lymphocytes and basal cell hyperplasia in gastroesophageal reflux disease, infiltration T lymphocytes in squamous mucosa in lymphocytic esophagitis and eosinophilic necrosis in caustic ingestion
Causes
Common causes of esophageal stricture include gastroesophageal reflux disease and caustic ingestions.
Differentiating Esophageal stricture from other Disorders
Esophageal stricture must be differentiated from plummer-vinson syndrome, achalasia , diffuse esophageal spasm, systemic sclerosis, zenker's diverticulum, esophageal carcinoma, stroke, motor disorders, GERD, esophageal web.
Epidemiology and Demographics
Most of esophageal strictures are related to gastroesophageal reflux disease. Overall incidence of esophageal stricture is approximately 11 per 100,000 individuals and the prevalence of esophagealstricture is approximately 70-120 per 100,000 individuals in united states. The incidence of esophageal stricture increases with age. There is no racial predilection to esophageal stricture. The risk of esophageal stricture is higher in men under 60 yr but there is similar incidence in men and women after age 60.
Risk Factors
The most potent risk factor in the development of esophageal stricture is frequent acid reflux. Other risk factors include hiatal hernia, obesity, smoking, esophageal dysmotility, increased gastric acidity, and heavy alcohol use.
Natural History, Complications, and Prognosis
If left untreated, patients with esophageal stricture may progress to develop pulmonary aspiration, weight loss, and dehydration. Common complications of esophageal stricture include perforation, bleeding, pneumonia, bacteremia. Prognosis is generally good but recurrence of symptoms after dilation are prevalent and usually recurrent dilation is necessary.
Diagnosis
Diagnostic Study of Choice | History and Symptoms | Physical Examination | Laboratory Findings | Electrocardiogram | X Rays | CT | MRI | Echocardiography or Ultrasound | Other Imaging Findings | Other Diagnostic Studies
Treatment
Medical Therapy | Surgical | Primary Prevention | Secondary Prevention | Cost-Effectiveness of Therapy | Future or Investigational Therapies