WBR0491: Difference between revisions
Jump to navigation
Jump to search
Rim Halaby (talk | contribs) No edit summary |
m (refreshing WBR questions) |
||
| (11 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
{{WBRQuestion | {{WBRQuestion | ||
|QuestionAuthor={{ | |QuestionAuthor= {{SSK}} (Reviewed by Serge Korjian and {{AJL}}) | ||
|ExamType=USMLE Step 1 | |ExamType=USMLE Step 1 | ||
|MainCategory=Immunology | |MainCategory=Immunology | ||
| Line 8: | Line 8: | ||
|MainCategory=Immunology | |MainCategory=Immunology | ||
|SubCategory=Pulmonology | |SubCategory=Pulmonology | ||
|MainCategory=Immunology | |||
|MainCategory=Immunology | |MainCategory=Immunology | ||
|MainCategory=Immunology | |MainCategory=Immunology | ||
| Line 20: | Line 21: | ||
|MainCategory=Immunology | |MainCategory=Immunology | ||
|SubCategory=Pulmonology | |SubCategory=Pulmonology | ||
|Prompt=A 7-year-old boy | |Prompt=A 7-year-old boy is brought to the emergency department for several hours of unremitting cough. The mother mentions that this is not the first occurrence, as he has been having severe coughing fits at night and following gym class for several weeks now. Physical examination reveals significant wheezing and decreased air entry bilaterally. Expression of which of the following mediators is likely to be elevated in this patient? | ||
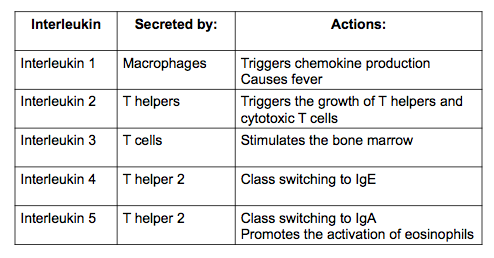
|Explanation=The | |Explanation=Asthma is an airway disease characterized by reversible bronchial obstruction with chronic underlying airway inflammation. The main pathophysiologic mechanism underlying asthma is Th2-cell mediated inflammation. In vivo, the ratio of Th2/Th1 is markedly elevated in patients with asthma. Consequently, Th2 cytokines, particularly interleukin 4, 5, and 13 are significantly increased. Interleukin-4 is a major contributor to the disease pathogenesis. It promotes class switching of immunoglobulin into [[IgE]], and stimulates the differentiation of immature T-cells into Th2 cells. | ||
[[File:Interleukin.png]] | The table below summarizes the roles of interleukins and the main cells that secrete them. | ||
<br> | |||
[[File:Interleukin.png]]<br> | |||
|AnswerA=Interleukin 1 | |AnswerA=Interleukin 1 | ||
|AnswerAExp=Interleukin 1 | |AnswerAExp=Interleukin 1 impacts the activity of [[hypothalamus]], the thermoregulatory center, which leads to a raise of a body temperature. Interleukin 1 is not involved in [[asthma]]. | ||
|AnswerB=Interleukin | |AnswerB=Interleukin 3 | ||
|AnswerBExp=Interleukin | |AnswerBExp=Interleukin 3, secreted by [[basophil]]s and activated [[T cells]], supports growth and differentiation of T cells from [[bone marrow]] in an immune response. Interleukin 3 is not involved in [[asthma]]. | ||
|AnswerC=Interleukin 4 | |||
|AnswerCExp=Interleukin 4 induces [[B-cell]] class switching to [[IgE]], and up-regulates MHC class II production. IL-4 decreases the production of Th1 cells, macrophages, IFN-gamma, and dendritic cell IL-12. | |||
| | |AnswerD=Interleukin 10 | ||
| | |AnswerDExp=Interleukin 10 is a major regulator of T<sub>reg</sub>-cell activity, and is usually decreased in patients with asthma. | ||
| | |AnswerE=Interleukin 12 | ||
| | |AnswerEExp=Interleukin 12 is important for the differentiation of helper T-cells into Th1 cells. Interleukin 12 is not elevated in [[asthma]]. | ||
|RightAnswer= | |EducationalObjectives=Asthma is a Th2-mediated disease with elevated levels of Th2 cytokines, particularly interleukin 4, 5, and 13. | ||
|WBRKeyword=Interleukin, | |References=Martinez FD, Vercelli D. Asthma. Lancet, 2013;382(9901):1360-72.<br> | ||
|Approved= | Akdis M, Burgler S, Crameri R, Eiwegger T, Fujita H, Gomez E, Klunker S, Meyer N, O'Mahony L, Palomares O, Rhyner C, Ouaked N, Schaffartzik A, Van De Veen W, Zeller S, Zimmermann M, Akdis CA. Interleukins, from 1 to 37, and interferon-γ: receptors, functions, and roles in diseases. J Allergy Clin Immunol. 2011 Mar;127(3):701-21.e1-70.<br> | ||
First Aid 2014 page 205 | |||
|RightAnswer=C | |||
|WBRKeyword=Interleukins, Interleukin, Asthma, Immunoglobulin, IgE, Atopy, IL-4, IL-5, IL-13 | |||
|Approved=Yes | |||
}} | }} | ||
Latest revision as of 00:45, 28 October 2020
| Author | [[PageAuthor::Serge Korjian M.D. (Reviewed by Serge Korjian and Alison Leibowitz [1])]] |
|---|---|
| Exam Type | ExamType::USMLE Step 1 |
| Main Category | MainCategory::Immunology |
| Sub Category | SubCategory::Pulmonology |
| Prompt | [[Prompt::A 7-year-old boy is brought to the emergency department for several hours of unremitting cough. The mother mentions that this is not the first occurrence, as he has been having severe coughing fits at night and following gym class for several weeks now. Physical examination reveals significant wheezing and decreased air entry bilaterally. Expression of which of the following mediators is likely to be elevated in this patient?]] |
| Answer A | AnswerA::Interleukin 1 |
| Answer A Explanation | [[AnswerAExp::Interleukin 1 impacts the activity of hypothalamus, the thermoregulatory center, which leads to a raise of a body temperature. Interleukin 1 is not involved in asthma.]] |
| Answer B | AnswerB::Interleukin 3 |
| Answer B Explanation | [[AnswerBExp::Interleukin 3, secreted by basophils and activated T cells, supports growth and differentiation of T cells from bone marrow in an immune response. Interleukin 3 is not involved in asthma.]] |
| Answer C | AnswerC::Interleukin 4 |
| Answer C Explanation | [[AnswerCExp::Interleukin 4 induces B-cell class switching to IgE, and up-regulates MHC class II production. IL-4 decreases the production of Th1 cells, macrophages, IFN-gamma, and dendritic cell IL-12.]] |
| Answer D | AnswerD::Interleukin 10 |
| Answer D Explanation | [[AnswerDExp::Interleukin 10 is a major regulator of Treg-cell activity, and is usually decreased in patients with asthma.]] |
| Answer E | AnswerE::Interleukin 12 |
| Answer E Explanation | [[AnswerEExp::Interleukin 12 is important for the differentiation of helper T-cells into Th1 cells. Interleukin 12 is not elevated in asthma.]] |
| Right Answer | RightAnswer::C |
| Explanation | [[Explanation::Asthma is an airway disease characterized by reversible bronchial obstruction with chronic underlying airway inflammation. The main pathophysiologic mechanism underlying asthma is Th2-cell mediated inflammation. In vivo, the ratio of Th2/Th1 is markedly elevated in patients with asthma. Consequently, Th2 cytokines, particularly interleukin 4, 5, and 13 are significantly increased. Interleukin-4 is a major contributor to the disease pathogenesis. It promotes class switching of immunoglobulin into IgE, and stimulates the differentiation of immature T-cells into Th2 cells.
The table below summarizes the roles of interleukins and the main cells that secrete them.
|
| Approved | Approved::Yes |
| Keyword | WBRKeyword::Interleukins, WBRKeyword::Interleukin, WBRKeyword::Asthma, WBRKeyword::Immunoglobulin, WBRKeyword::IgE, WBRKeyword::Atopy, WBRKeyword::IL-4, WBRKeyword::IL-5, WBRKeyword::IL-13 |
| Linked Question | Linked:: |
| Order in Linked Questions | LinkedOrder:: |