WBR0322: Difference between revisions
Jump to navigation
Jump to search
Rim Halaby (talk | contribs) (Created page with "{{WBRQuestion |QuestionAuthor={{Rim}} |ExamType=USMLE Step 1 |MainCategory=Pathophysiology |SubCategory=Hematology |MainCategory=Pathophysiology |SubCategory=Hematology |MainC...") |
m (refreshing WBR questions) |
||
| (11 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
{{WBRQuestion | {{WBRQuestion | ||
|QuestionAuthor={{ | |QuestionAuthor= {{SSK}} {{Alison}} (Reviewed by Serge Korjian) | ||
|ExamType=USMLE Step 1 | |ExamType=USMLE Step 1 | ||
|MainCategory= | |MainCategory=Immunology | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory= | |MainCategory=Immunology | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory= | |MainCategory=Immunology | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory= | |MainCategory=Immunology | ||
|MainCategory= | |MainCategory=Immunology | ||
|MainCategory=Immunology | |||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory= | |MainCategory=Immunology | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory= | |MainCategory=Immunology | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory= | |MainCategory=Immunology | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|MainCategory= | |MainCategory=Immunology | ||
|MainCategory= | |MainCategory=Immunology | ||
|SubCategory=Hematology | |SubCategory=Hematology | ||
|Prompt=A 67 year old presents to the | |Prompt=A 67-year-old man presents to the physician's office with complaints of weight loss, fever, and night sweats. Following appropriate work-up,you diagnose him with acute myelogenous leukemia (AML) and start him on scheduled chemotherapy sessions. Three weeks into the treatment, you detect that patient is profoundly thrombocytopenic and requires a platelet transfusion. During the transfusion, the patient develops fever, chills, and intense flushing, but denies any itching or shortness of breath. On physical exam, you find that the patient has a temperature of 38.5 °C (101.3 °F) , heart rate of 108 bpm, respiratory rate of 18/min, and blood pressure of 128/78 mmHg. What is the most likely cause of this patient's reaction to the platelet transfusion? | ||
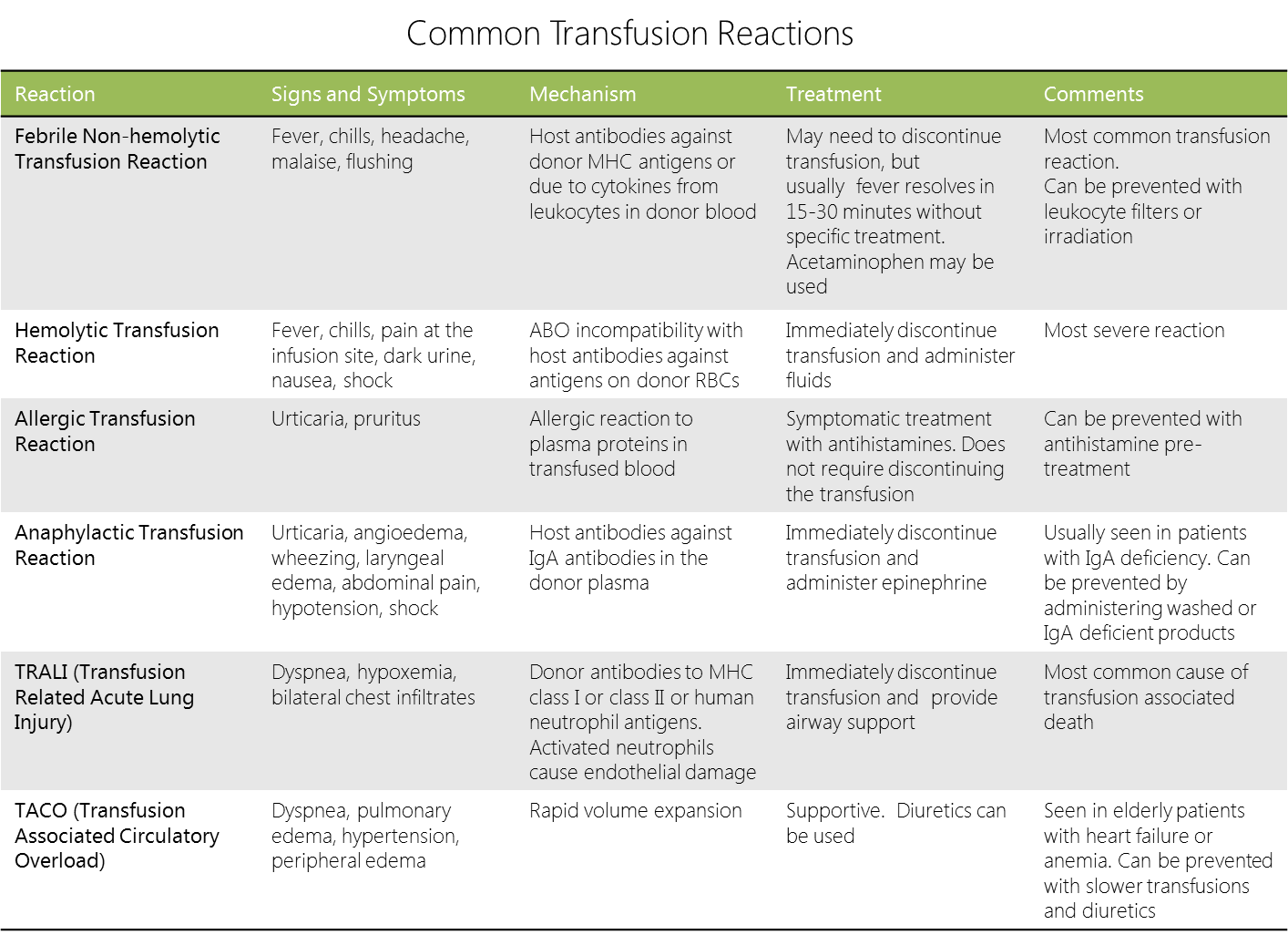
|Explanation=The | |Explanation=The patient in this scenario is most likely manifesting a [[febrile nonhemolytic transfusion reaction]] (FNHTR) most commonly occurring during platelet transfusions. The etiology of this reaction is directly related to cytokines that accumulate in the product during storage. The true mechanism of the accumulation is poorly understood although leukocyte [[apoptosis]] and monocyte activation during platelet processing may play a role. In packed red blood cells however, the role of cytokines in FNHTR is minor. The pathophysiology is believed to be mostly caused by recipient humoral and cell activity against transfused leukocytes (via non-self HLA) and subsequent febrile reaction. The treatment is still controversial, but includes fever reduction by antipyretics (such as acetaminophen). Stopping the transfusion is also generally accepted but not always necessary. | ||
[[File:Transfusion_reactions.png|1000px]] | |||
|AnswerA=Formation of IgG and IgA immune complexes that activate the complement pathway and release C3a and C5a | |AnswerA=Formation of IgG and IgA immune complexes that activate the complement pathway and release C3a and C5a | ||
|AnswerAExp=Anaphylactic reaction, usually in patients with IgA deficiency, is caused by formation of immune complexes that activate anaphylaxins, such as C3a and C5a. Patients typically present with features of anaphylaxis, such as hypotension and shock. | |AnswerAExp=Anaphylactic reaction, usually occurring in patients with IgA deficiency, is caused by formation of immune complexes that activate anaphylaxins, such as C3a and C5a. Patients typically present with features characteristic of anaphylaxis, such as hypotension and shock. | ||
|AnswerB=Reaction by cytokines | |AnswerB=Reaction caused primarily by the accumulation of cytokines in the platelet products during storage | ||
|AnswerBExp= | |AnswerBExp=See explanation. | ||
|AnswerC=Hypersensitivity reaction against foreign antigens on donor red blood cells | |AnswerC=Hypersensitivity reaction against foreign antigens on donor red blood cells | ||
|AnswerCExp=Acute and delayed hemolytic transfusion reactions | |AnswerCExp=Acute and delayed hemolytic transfusion reactions, resulting from hypersensitivity reactions against foreign antigens on donor red blood cells, manifest in jaundice, flank pain, and hemoglobinuria. | ||
|AnswerD=Production of IgE by plasma cells following antigen exposure | |AnswerD=Production of IgE by plasma cells following antigen exposure | ||
|AnswerDExp= | |AnswerDExp=Following antigen exposure, allergic reaction may result from IgE production by plasma cells. The allergic reaction typically manifest with urticaria, pruritis, and wheezing. | ||
|AnswerE=Non-immune circulatory overload due to incoming transfused blood | |AnswerE=Non-immune circulatory overload due to rapidly incoming transfused blood | ||
|AnswerEExp=Transfusion-associated circulatory overload (TACO) | |AnswerEExp=Transfusion-associated circulatory overload (TACO) results from the rapid transfusion of blood products. TACO is a non-immune condition, which typically causes high blood pressure, peripheral edema, dyspnea, and orthopnea. | ||
|EducationalObjectives=[[Febrile nonhemolytic transfusion reaction|Febrile nonhemolytic transfusion reaction (FNHTR)]], most frequently occurs following platelet transfusions, are due to cytokine accumulation in the platelet products during storage. In RBC transfusions, the reaction occurs due to an immune process against donor HLA antigens. | |||
|References=Tenorio GC, Gupte SC, Munker R. Transfusion medicine and immunohematology. in Modern Hematology - Biology and Clinical Management, 2nd ed. 2007. pp:401-432.<br> | |||
Heddle NM. Pathophysiology of febrile nonhemolytic transfusion reactions. Curr Opin Hematol. 1999; 6(6):420-6. | |||
|RightAnswer=B | |RightAnswer=B | ||
|WBRKeyword= | |WBRKeyword=Transfusion, Transfusion reactions, FNHTR, Febrile nonhemolytic transfusion reaction, Platelets, Platelet transfusion, Hypersensitivity reactions, | ||
|Approved= | |Approved=Yes | ||
}} | }} | ||
Latest revision as of 00:11, 28 October 2020
| Author | [[PageAuthor::Serge Korjian M.D. (Reviewed by Alison Leibowitz) (Reviewed by Serge Korjian)]] |
|---|---|
| Exam Type | ExamType::USMLE Step 1 |
| Main Category | MainCategory::Immunology |
| Sub Category | SubCategory::Hematology |
| Prompt | [[Prompt::A 67-year-old man presents to the physician's office with complaints of weight loss, fever, and night sweats. Following appropriate work-up,you diagnose him with acute myelogenous leukemia (AML) and start him on scheduled chemotherapy sessions. Three weeks into the treatment, you detect that patient is profoundly thrombocytopenic and requires a platelet transfusion. During the transfusion, the patient develops fever, chills, and intense flushing, but denies any itching or shortness of breath. On physical exam, you find that the patient has a temperature of 38.5 °C (101.3 °F) , heart rate of 108 bpm, respiratory rate of 18/min, and blood pressure of 128/78 mmHg. What is the most likely cause of this patient's reaction to the platelet transfusion?]] |
| Answer A | AnswerA::Formation of IgG and IgA immune complexes that activate the complement pathway and release C3a and C5a |
| Answer A Explanation | [[AnswerAExp::Anaphylactic reaction, usually occurring in patients with IgA deficiency, is caused by formation of immune complexes that activate anaphylaxins, such as C3a and C5a. Patients typically present with features characteristic of anaphylaxis, such as hypotension and shock.]] |
| Answer B | AnswerB::Reaction caused primarily by the accumulation of cytokines in the platelet products during storage |
| Answer B Explanation | AnswerBExp::See explanation. |
| Answer C | AnswerC::Hypersensitivity reaction against foreign antigens on donor red blood cells |
| Answer C Explanation | AnswerCExp::Acute and delayed hemolytic transfusion reactions, resulting from hypersensitivity reactions against foreign antigens on donor red blood cells, manifest in jaundice, flank pain, and hemoglobinuria. |
| Answer D | AnswerD::Production of IgE by plasma cells following antigen exposure |
| Answer D Explanation | AnswerDExp::Following antigen exposure, allergic reaction may result from IgE production by plasma cells. The allergic reaction typically manifest with urticaria, pruritis, and wheezing. |
| Answer E | AnswerE::Non-immune circulatory overload due to rapidly incoming transfused blood |
| Answer E Explanation | AnswerEExp::Transfusion-associated circulatory overload (TACO) results from the rapid transfusion of blood products. TACO is a non-immune condition, which typically causes high blood pressure, peripheral edema, dyspnea, and orthopnea. |
| Right Answer | RightAnswer::B |
| Explanation | [[Explanation::The patient in this scenario is most likely manifesting a febrile nonhemolytic transfusion reaction (FNHTR) most commonly occurring during platelet transfusions. The etiology of this reaction is directly related to cytokines that accumulate in the product during storage. The true mechanism of the accumulation is poorly understood although leukocyte apoptosis and monocyte activation during platelet processing may play a role. In packed red blood cells however, the role of cytokines in FNHTR is minor. The pathophysiology is believed to be mostly caused by recipient humoral and cell activity against transfused leukocytes (via non-self HLA) and subsequent febrile reaction. The treatment is still controversial, but includes fever reduction by antipyretics (such as acetaminophen). Stopping the transfusion is also generally accepted but not always necessary.
|
| Approved | Approved::Yes |
| Keyword | WBRKeyword::Transfusion, WBRKeyword::Transfusion reactions, WBRKeyword::FNHTR, WBRKeyword::Febrile nonhemolytic transfusion reaction, WBRKeyword::Platelets, WBRKeyword::Platelet transfusion, WBRKeyword::Hypersensitivity reactions |
| Linked Question | Linked:: |
| Order in Linked Questions | LinkedOrder:: |