Meningitis pathophysiology: Difference between revisions
m (Bot: Removing from Primary care) |
|||
| (11 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Meningitis}} | {{Meningitis}} | ||
{{CMG}}; '''Associate Editor(s)-In-Chief:''' {{CZ}} | {{CMG}}; '''Associate Editor(s)-In-Chief:''' {{CZ}} | ||
==Pathophysiology== | ==Pathophysiology== | ||
The clinical picture of meningitis largely arises from the host response to the inciting organism in the CSF. | The clinical picture of meningitis largely arises from the host response to the inciting organism in the CSF. | ||
* It seems that the subcapsular components (the cell wall and lipopolysaccharide) of bacteria are more important in determining inflammation than the surface components (pili and polysaccharide capsule). | * It seems that the subcapsular components (the cell wall and [[lipopolysaccharide]]) of bacteria are more important in determining [[inflammation]] than the surface components ([[pili]] and [[polysaccharide]] capsule). | ||
* The primary site of breakdown of the blood-brain barrier is the cerebral microvascular endothelium. | * The primary site of breakdown of the [[blood-brain barrier]] is the cerebral microvascular endothelium. | ||
*:* Electron microscope (EM) studies have shown complete separation of the intercellular tight junctions | *:* [[Electron microscope]] (EM) studies have shown complete separation of the intercellular tight junctions | ||
* It appears that there is a final common pathway, mediated by TNF-alpha, IL-1 and IL-6, that results in meningeal inflammation and loss of the blood-brain barrier. | * It appears that there is a final common pathway, mediated by TNF-alpha, IL-1 and IL-6, that results in meningeal inflammation and loss of the blood-brain barrier. | ||
*:* One of the major roles of these cytokines is to facilitate the migration of neutrophils across the vascular endothelium into the CSF. | *:* One of the major roles of these [[cytokines]] is to facilitate the migration of [[neutrophils]] across the vascular [[endothelium]] into the CSF. | ||
*:* A key initial step in this process is obviously adhesion of the PMN to the endothelial surface. | *:* A key initial step in this process is obviously adhesion of the PMN to the endothelial surface. | ||
*:*:* This is mediated by the expression of specific transmembrane glycoproteins expressed on the endothelial surface that interact with specific counterparts on the neutrophils. | *:*:* This is mediated by the expression of specific transmembrane glycoproteins expressed on the endothelial surface that interact with specific counterparts on the neutrophils. | ||
*:*:* These adhesion molecules fall into three large categories: the immunoglobin superfamily (including the antigen-specific T and B cell receptors, ICAM-1 and ICAM-2), the integrin family (beta-1, beta-2, and beta-3) and the selectin family (including ELAM-1). | *:*:* These adhesion molecules fall into three large categories: the [[immunoglobin]] superfamily (including the antigen-specific T and B cell receptors, ICAM-1 and ICAM-2), the [[integrin]] family (beta-1, beta-2, and beta-3) and the selectin family (including ELAM-1). | ||
*:* The interaction of beta-2 integrin (CD18) and ICAM-1 is largely responsible for PMN diapedesis. | *:* The interaction of beta-2 integrin (CD18) and ICAM-1 is largely responsible for PMN diapedesis. | ||
* Additionally, patients get cerebral edema that is mediated by an increase in capillary permeability, the inflammatory response from the neutrophils, and CSF outflow resistance. | * Additionally, patients get [[cerebral edema]] that is mediated by an increase in capillary permeability, the inflammatory response from the neutrophils, and CSF outflow resistance. | ||
* The above pathophysiologic processes are not only important in producing the symptoms associated with meningitis, but the understanding of the underlying disease process is necessary to guide therapy | * The above pathophysiologic processes are not only important in producing the symptoms associated with meningitis, but the understanding of the underlying disease process is necessary to guide therapy. | ||
==Mechanism== | ===Mechanism=== | ||
* In order to gain access to the CNS, the pathogen needs to colonize mucosal epithelium, invade and survive in the intravascular space, cross the blood-brain barrier and survive in the CSF. | * In order to gain access to the CNS, the pathogen needs to colonize mucosal epithelium, invade and survive in the intravascular space, cross the blood-brain barrier and survive in the CSF. | ||
* Colonization of the nasopharynx is usually asymptomatic, and during peak seasons, approximately 20% of the population are colonized with N. meningitidis. | * Colonization of the nasopharynx is usually asymptomatic, and during peak seasons, approximately 20% of the population are colonized with N. meningitidis. | ||
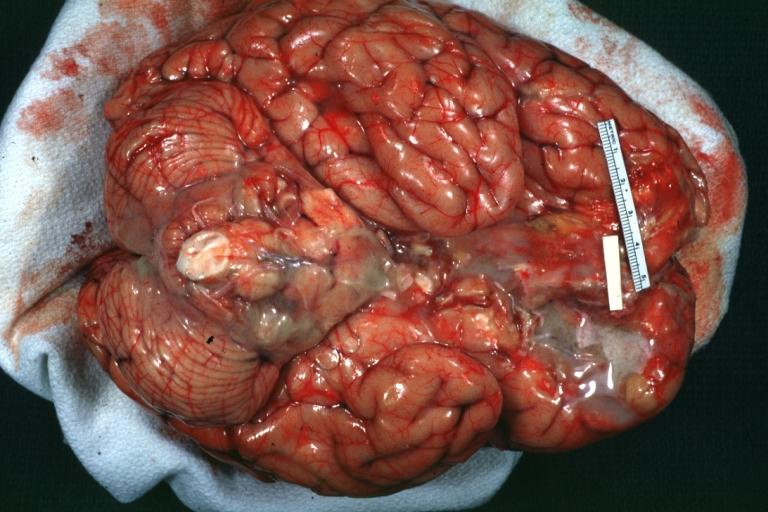
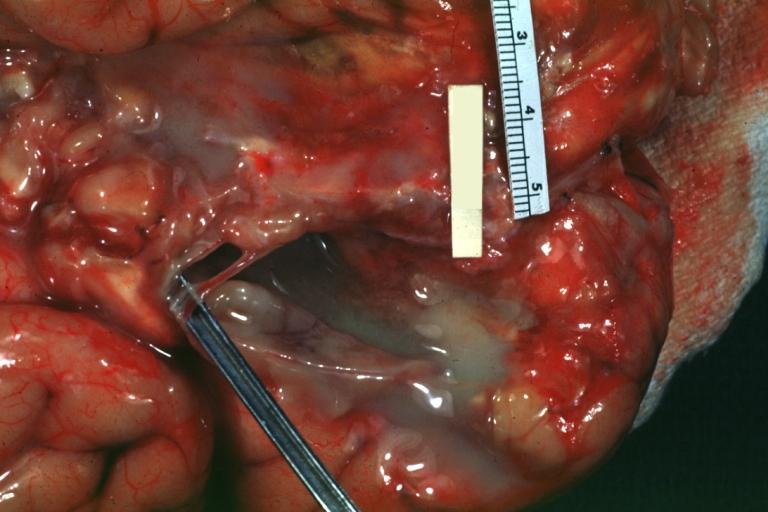
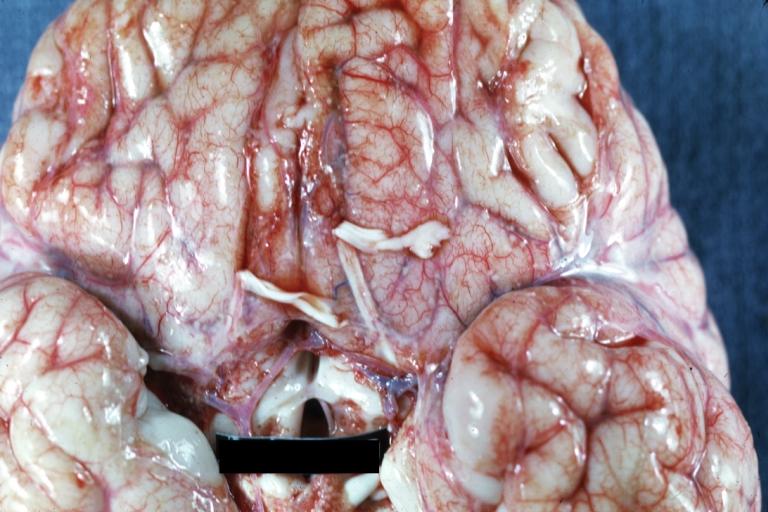
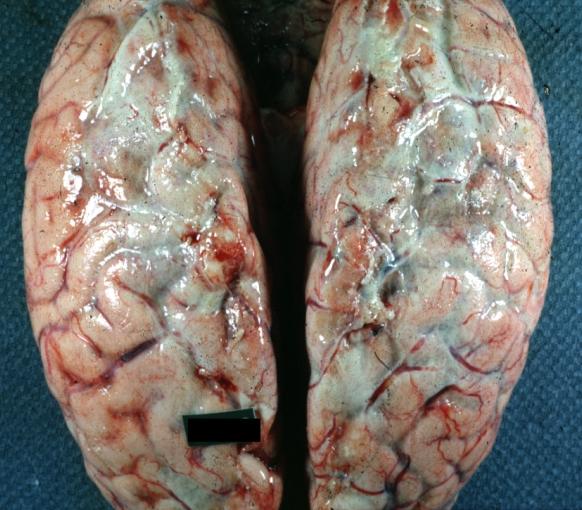
== | ===Gross Pathology=== | ||
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. [http://www.peir.net © PEIR, University of Alabama at Birmingham, Department of Pathology] | Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. [http://www.peir.net © PEIR, University of Alabama at Birmingham, Department of Pathology] | ||
| Line 76: | Line 75: | ||
</div> | </div> | ||
== | ===Microscopic Pathology=== | ||
{{#ev:youtube|L9jpjxTSLws}} | {{#ev:youtube|L9jpjxTSLws}} | ||
==References== | ==References== | ||
{{ | {{Reflist|2}} | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[Category:Needs overview]] | |||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Neurology]] | [[Category:Neurology]] | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Diseases involving the fasciae]] | |||
[[Category:Inflammations]] | |||
[[Category:Neurological disorders]] | |||
Latest revision as of 22:42, 29 July 2020
|
Meningitis Main Page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Pathophysiology
The clinical picture of meningitis largely arises from the host response to the inciting organism in the CSF.
- It seems that the subcapsular components (the cell wall and lipopolysaccharide) of bacteria are more important in determining inflammation than the surface components (pili and polysaccharide capsule).
- The primary site of breakdown of the blood-brain barrier is the cerebral microvascular endothelium.
- Electron microscope (EM) studies have shown complete separation of the intercellular tight junctions
- It appears that there is a final common pathway, mediated by TNF-alpha, IL-1 and IL-6, that results in meningeal inflammation and loss of the blood-brain barrier.
- One of the major roles of these cytokines is to facilitate the migration of neutrophils across the vascular endothelium into the CSF.
- A key initial step in this process is obviously adhesion of the PMN to the endothelial surface.
- This is mediated by the expression of specific transmembrane glycoproteins expressed on the endothelial surface that interact with specific counterparts on the neutrophils.
- These adhesion molecules fall into three large categories: the immunoglobin superfamily (including the antigen-specific T and B cell receptors, ICAM-1 and ICAM-2), the integrin family (beta-1, beta-2, and beta-3) and the selectin family (including ELAM-1).
- The interaction of beta-2 integrin (CD18) and ICAM-1 is largely responsible for PMN diapedesis.
- Additionally, patients get cerebral edema that is mediated by an increase in capillary permeability, the inflammatory response from the neutrophils, and CSF outflow resistance.
- The above pathophysiologic processes are not only important in producing the symptoms associated with meningitis, but the understanding of the underlying disease process is necessary to guide therapy.
Mechanism
- In order to gain access to the CNS, the pathogen needs to colonize mucosal epithelium, invade and survive in the intravascular space, cross the blood-brain barrier and survive in the CSF.
- Colonization of the nasopharynx is usually asymptomatic, and during peak seasons, approximately 20% of the population are colonized with N. meningitidis.
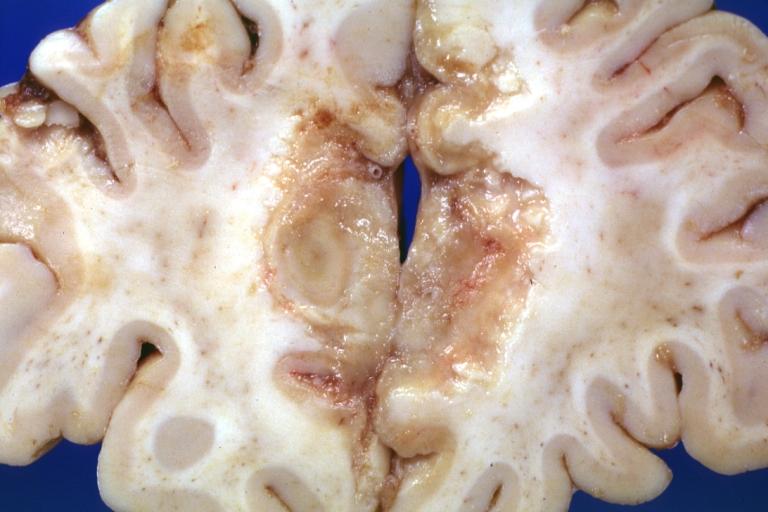
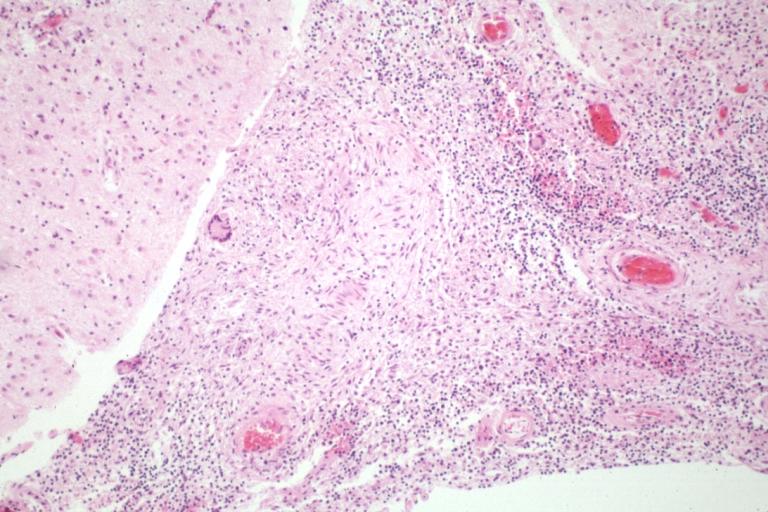
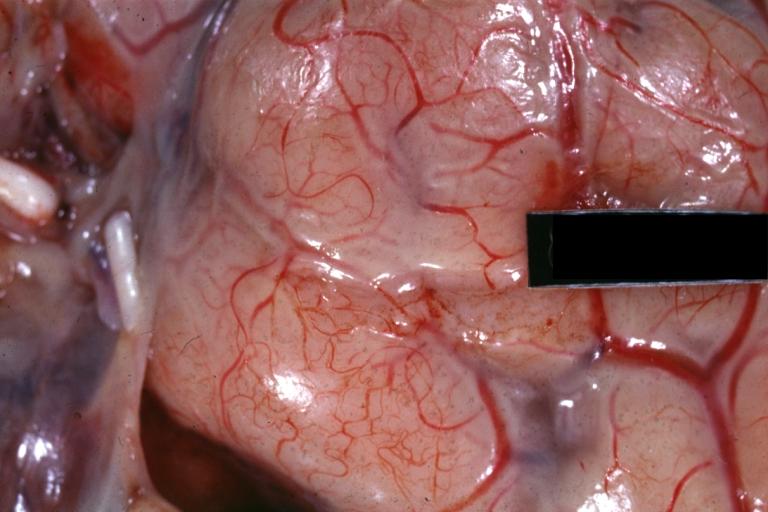
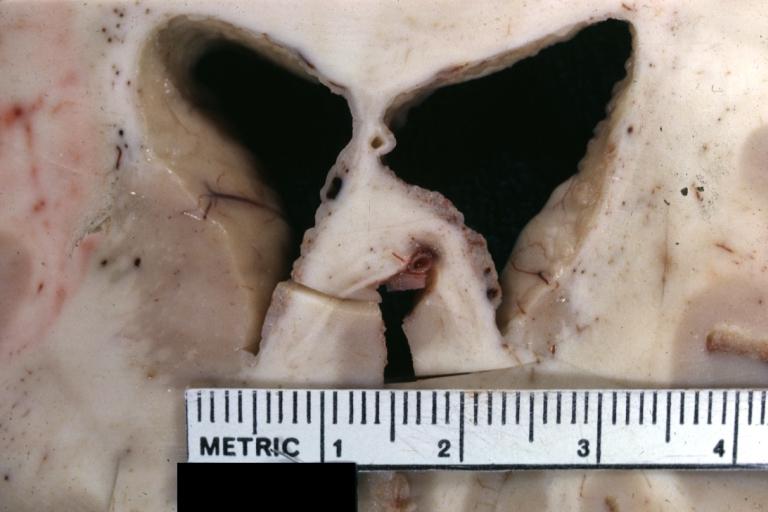
Gross Pathology
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Meningitis: Gross, purulent leptomeningitis due to pneumococcus infection, an excellent example.
-
Bacterial Meningitis: Gross, basilar view
-
Bacterial Meningitis: Gross close-up
-
Meningitis: Gross base of frontal lobes well shown meningitis burn case with Pseudomonas sepsis
-
Meningitis: Gross natural color excellent demonstration of greenish pus in subarachnoid space
-
Tuberculous Meningitis: Gross fixed tissue close-up of large areas of necrosis in frontal parasagittal cortex secondary to tuberculous vasculitis. An excellent example
-
Tuberculous Meningitis: Micro low mag H&E. An excellent example with giant cells.
-
Purulent Meningitis: Gross natural color excellent photo lateral aspect of brain with easily seen purulent exudate due to Pneumococcus infection.
-
Purulent Meningitis: Gross natural color close-up view outstanding example of purulent exudate adjacent to blood vessels
-
Purulent Meningitis: Gross natural color Staphylococcal meningitis.
-
Ependymitis Granular Neoplastic: Gross fixed tissue close-up view and a spectacular one of this lesion case also has carcinomatous meningitis primary is lung oat cell.
-
Purulent Meningitis: Gross natural color brain in situ with removed calvarium very good illustration of exudate in meninges over convexities pneumococcus.
Microscopic Pathology
{{#ev:youtube|L9jpjxTSLws}}