Glomerulonephritis pathophysiology: Difference between revisions
(→Images) |
m (Bot: Removing from Primary care) |
||
| (5 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div style="-webkit-user-select: none;"> | |||
{| class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right;" | |||
|- | |||
| {{#ev:youtube|https://https://www.youtube.com/watch?v=zucxZw069kw|350}} | |||
|- | |||
|} | |||
__NOTOC__ | __NOTOC__ | ||
{{CMG}} | {{CMG}} | ||
{{Glomerulonephritis}} | {{Glomerulonephritis}} | ||
==Pathophysiology== | ==Pathophysiology== | ||
===Microscopic Pathology=== | ===Microscopic Pathology=== | ||
[http://www.peir.net Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | [http://www.peir.net Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | ||
| Line 28: | Line 33: | ||
{{#ev:youtube|eA1vYarRAWo}} | {{#ev:youtube|eA1vYarRAWo}} | ||
===Images=== | ===Images=== | ||
| Line 49: | Line 44: | ||
</gallery> | </gallery> | ||
</div> | </div> | ||
<div align="left"> | <div align="left"> | ||
| Line 57: | Line 51: | ||
</gallery> | </gallery> | ||
</div> | </div> | ||
<div align="left"> | <div align="left"> | ||
| Line 65: | Line 58: | ||
</gallery> | </gallery> | ||
</div> | </div> | ||
<div align="left"> | <div align="left"> | ||
| Line 73: | Line 65: | ||
</gallery> | </gallery> | ||
</div> | </div> | ||
<div align="left"> | <div align="left"> | ||
| Line 89: | Line 80: | ||
==References== | ==References== | ||
{{ | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Disease]] | [[Category:Disease]] | ||
| Line 95: | Line 88: | ||
[[Category:Inflammations]] | [[Category:Inflammations]] | ||
[[Category:Kidney diseases]] | [[Category:Kidney diseases]] | ||
[[Category:Needs overview]] | |||
Latest revision as of 21:53, 29 July 2020
| https://https://www.youtube.com/watch?v=zucxZw069kw%7C350}} |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
|
Glomerulonephritis Main page |
|
|---|
Pathophysiology
Microscopic Pathology
-
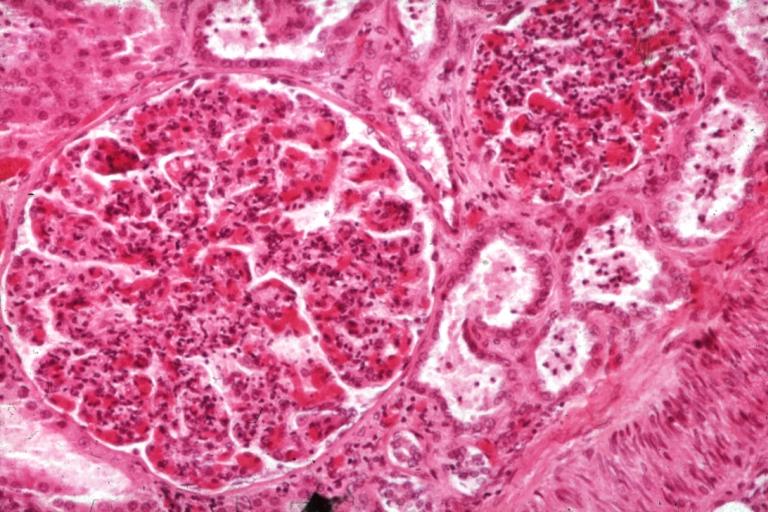
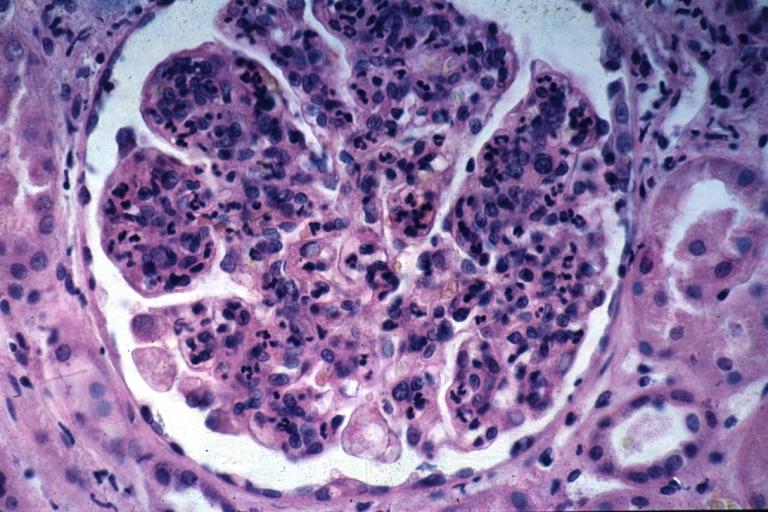
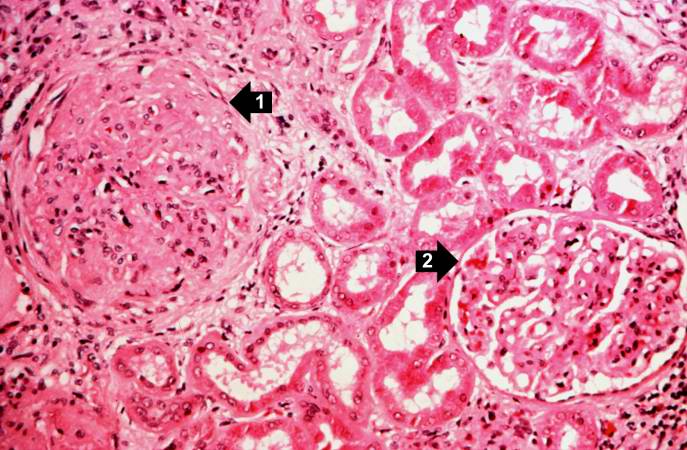
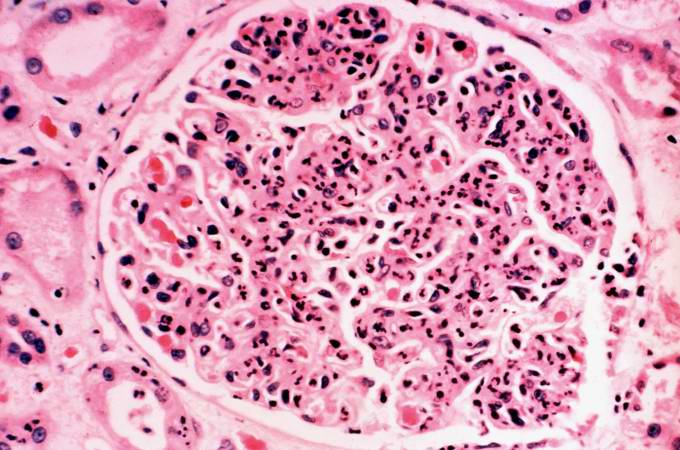
Glomerulonephritis: Micro H&E med mag; an excellent example of AGN with many neutrophils
-
Acute Glomerulonephritis: Micro H&E high mag; an excellent example of acute exudative glomerulonephritis.
Glomerulonephritis Videos
Rapidly progressive glomerulonephritis
{{#ev:youtube|CqSyj4cVZPE}}
Chronic glomerulonephritis
{{#ev:youtube|eA1vYarRAWo}}
Images
-
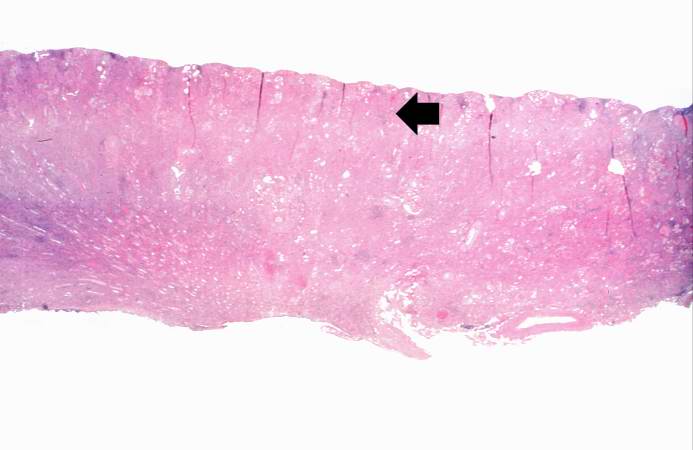
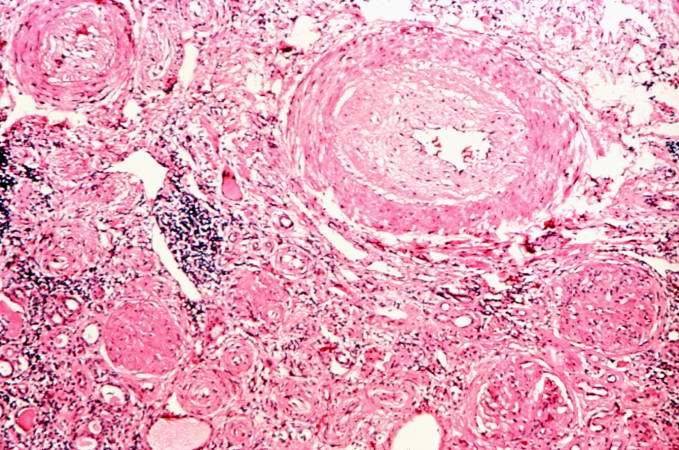
This is a low-power photomicrograph of a saggital section of end stage chronic glomerulonephritis (GN). Note the marked thinning of the cortex (arrow).
-
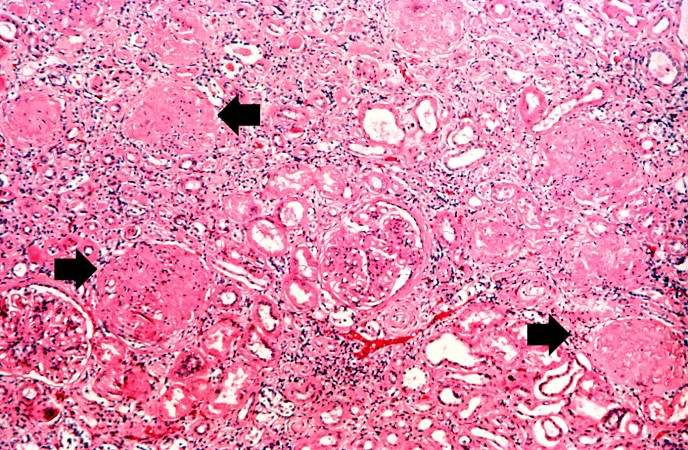
This is a higher-power photomicrograph of hyalinized glomeruli (arrows) and glomeruli with thick basement membranes.
-
This is a higher-power photomicrograph of hyalinized glomeruli (1) and glomeruli with thickened basement membranes (2).
-
This is a photomicrograph of interstitial and vascular lesions in end stage renal disease.
-
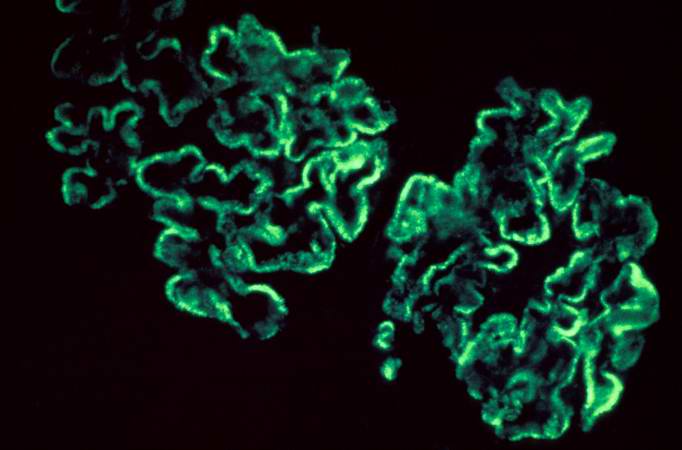
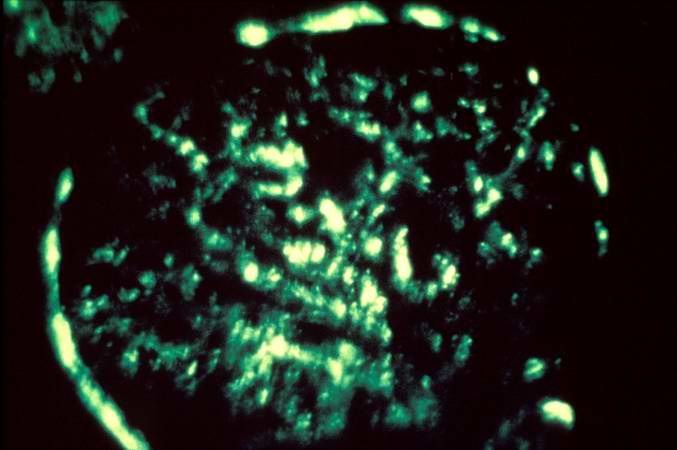
This is an immunofluorescent photomicrograph of granular membranous immunofluorescence (immune complex disease). The antibody used for these studies was specific for IgG.
-
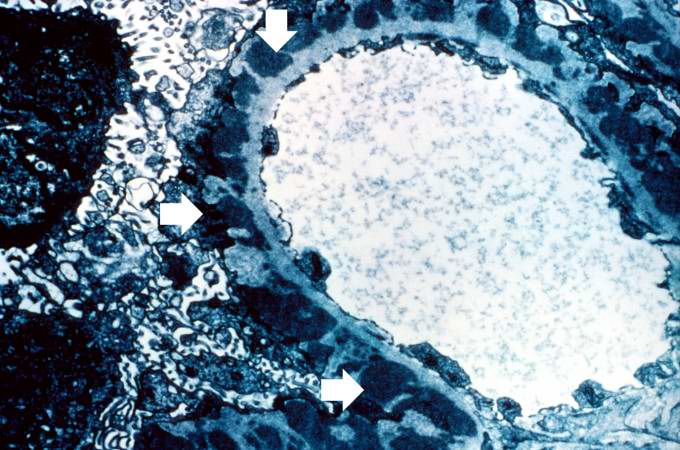
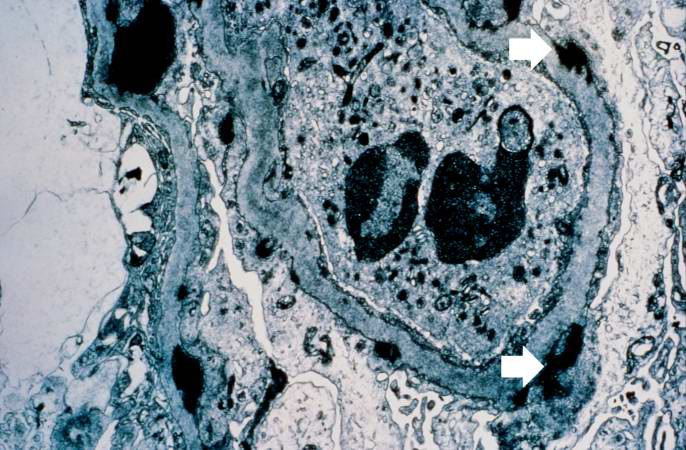
This is an electron micrograph of subepithelial granular electron dense deposits (arrows) which correspond to the granular immunofluorescence seen in the previous image.
-
This is a photomicrograph of a glomerulus from another case with acute poststreptococcal glomerulonephritis. In this case the immune complex glomerular disease is ongoing with necrosis and accumulation of neutrophils in the glomerulus.
-
This immunofluorescent photomicrograph of a glomerulus from a case of acute poststreptococcal glomerulonephritis shows a granular immunofluorescence pattern consistent with immune complex disease. The primary antibody used for this staining was specific for IgG; however antibodies for complement would show a similar pattern.
-
This electron micrograph demonstrates scattered subepithelial dense deposits (arrows) and a polymorphonuclear leukocyte in the lumen.
-
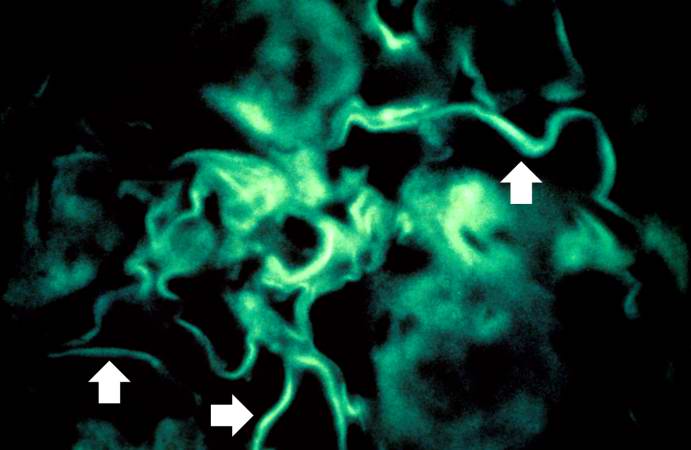
For comparison this is an immunofluorescent photomicrograph of a glomerulus from a patient with Goodpasture's syndrome. The linear (arrows) immunofluorescence is characteristic of Goodpasture's syndrome.