Breast cancer epidemiology and demographics: Difference between revisions
No edit summary |
|||
| (64 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
{{ | __NOTOC__ | ||
{{Editor | {{Breast cancer}} | ||
{{CMG}}; {{AE}}{{Soroush}}{{Rim}}'''; Assistant Editor(s)-In-Chief:''' [[User:Jack Khouri|Jack Khouri]]; {{MGS}} | |||
==Overview== | |||
The prevalence of breast cancer is approximately 124.8 per 100,000 women per year. The number of deaths was 21.9 per 100,000 women per year, based on 2010-2012 data. About 1 out of 8 women in United states will develop invasive [[breast]] cancer. Annually (i . e in 2019) around 268,600 and 62,930 new cases of invasive and non-invasive (in situ) breast cancer are expected to be diagnosed respectively. In men, life time likelihood of developing breast cancer is about 1 in 883. Annually 2,670 new cases of invasive breast cancer are expected to be diagnosed in males. Breast cancer increasing pattern of [[incidence]] rates began decreasing after year 2000 in US. | |||
==Epidemiology and demographics== | |||
*About 1 out of 8 women in United states will develop invasive [[breast]] cancer. | |||
*Annually (i . e in 2019) around 268,600 and 62,930 new cases of invasive and non-invasive (in situ) breast cancer are expected to be diagnosed respectively. | |||
*In men, life time likelihood of developing breast cancer is about 1 in 883. | |||
*Annually 2,670 new cases of invasive breast cancer are expected to be diagnosed in males. | |||
*Breast cancer increasing pattern of [[incidence]] rates began decreasing after year 2000 in US. | |||
*According to the results of the Women’s Health Initiative study ,published in 2002, reduced use of [[hormone replacement therapy]] (HRT) by US women might explain the observed decreasing pattern of incidence. | |||
*Around 42000 women in the U.S. are expected to die annually from breast cancer. | |||
*Women under 50 have experienced larger decreases. | |||
*A decreasing pattern of death rates has been observed since 1989 which might be explained by treatment advances, earlier cancer detection courtesy of [[Screening (medicine)|screening]] programs, and increased awareness.<ref name="urlCancer Statistics Review, 1975-2015 - SEER Statistics">{{cite web |url=https://seer.cancer.gov/csr/1975_2015/ |title=Cancer Statistics Review, 1975-2015 - SEER Statistics |format= |work= |accessdate=}}</ref> | |||
** | |||
** | |||
**In the subgroup of women under 45, African-American women breast incidence of breast cancer is higher compared to the white women, and they are more likely to die of breast cancer. | |||
**Asian, Hispanic, and Native-American women, have a lower risk of developing and dying from breast cancer. | |||
* | |||
===Incidence=== | |||
*[https://seer.cancer.gov/csr/1975_2015/ The following tables represent age-adjusted SEER incidence rates, 2011-2015.] | |||
=== Age-Adjusted SEER Incidence<sup>a</sup> Rates, 2011-2015 === | |||
{| class="wikitable" | |||
! colspan="1" |Age at Diagnosis | |||
! colspan="1" |All Races, Females | |||
! colspan="1" |White Females | |||
! colspan="1" |Black Females | |||
|- | |||
!All ages | |||
|31.1 | |||
|30.8 | |||
|32.1 | |||
|- | |||
!Under 65 | |||
|23.1 | |||
|22.9 | |||
|21.9 | |||
|- | |||
!65 and over | |||
|86.7 | |||
|85.3 | |||
|102.9 | |||
|- | |||
!All ages (WHO world std)<sup>b</sup> | |||
|25.3 | |||
|25.0 | |||
|25. | |||
|} | |||
=== Age-Specific SEER Incidence Rates, 2011-2015 === | |||
{| class="wikitable" | |||
! colspan="1" |Age at Diagnosis | |||
! colspan="1" |All Races, Females | |||
! colspan="1" |White Females | |||
! colspan="1" |Black Females | |||
|- | |||
!<1 | |||
| - | |||
| - | |||
| - | |||
|- | |||
!1-4 | |||
| - | |||
| - | |||
| - | |||
|- | |||
!5-9 | |||
| - | |||
| - | |||
| - | |||
|- | |||
!10-14 | |||
| - | |||
| - | |||
| - | |||
|- | |||
!15-19 | |||
| - | |||
| - | |||
| - | |||
|- | |||
!20-24 | |||
|0.2 | |||
|0.2 | |||
| - | |||
|- | |||
!25-29 | |||
|0.7 | |||
|0.6 | |||
|0.8 | |||
|- | |||
!30-34 | |||
|2.7 | |||
|2.4 | |||
|3.1 | |||
|- | |||
!35-39 | |||
|9.6 | |||
|9.7 | |||
|8.6 | |||
|- | |||
!40-44 | |||
|40.7 | |||
|40.5 | |||
|34.5 | |||
|- | |||
!45-49 | |||
|62.5 | |||
|62.9 | |||
|49.4 | |||
|- | |||
!50-54 | |||
|70.5 | |||
|70.6 | |||
|62.9 | |||
|- | |||
!55-59 | |||
|73.1 | |||
|71.4 | |||
|79.2 | |||
|- | |||
!60-64 | |||
|86.6 | |||
|84.0 | |||
|101.7 | |||
|- | |||
!65-69 | |||
|108.4 | |||
|105.9 | |||
|122.0 | |||
|- | |||
!70-74 | |||
|103.4 | |||
|101.1 | |||
|123.2 | |||
|- | |||
!75-79 | |||
|88.0 | |||
|87.0 | |||
|112.8 | |||
|- | |||
!80-84 | |||
|64.3 | |||
|64.2 | |||
|74.9 | |||
|- | |||
!85+ | |||
|28.4 | |||
|28.2 | |||
|34.4 | |||
|} | |||
'''Footnotes:''' ''<sup>a</sup> SEER 18 areas. Rates are per 100,000 and are age-adjusted to the 2000 US Std Population (19 age groups - Census P25-1130), unless noted.'' | |||
''<sup>b</sup> Rates are per 100,000 and are age-adjusted to the world (WHO 2000-2025) standard million.'' | |||
''- Statistic not shown. Rate based on less than 16 cases for the time interval.'' | |||
*Estimated new breast cancer cases in 2018 was 266,120 which made 15% of all new caner cases. | |||
*The incidence of breast cancer varies greatly around the world: it is lowest in less-developed countries and greatest in the more-developed countries. | |||
*In the twelve world regions, the annual age-standardized [[incidence rate]]s per 100,000 women are as follows: | |||
::* in Eastern Asia,18; | |||
::* South Central Asia, 22; | |||
::* Sub-Saharan Africa, 22; | |||
::* South-Eastern Asia, 26; | |||
::*North Africa and Western Asia, 28; | |||
::*South and Central America, 42; | |||
::*Eastern Europe, 49; | |||
::* Southern Europe, 56; | |||
::*Northern Europe, 73; | |||
::*Oceania, 74; | |||
::*Western Europe, 78; | |||
::*and in North America, 90.<ref>[http://www.scribd.com/doc/2350813/World-Cancer-Report-2003-Stuart-e-Kleihues-WHO-e-IARC Stewart B. W. and Kleihues P. (Eds): World Cancer Report. IARCPress. Lyon 2003] {{wayback|url=http://www.scribd.com/doc/2350813/World-Cancer-Report-2003-Stuart-e-Kleihues-WHO-e-IARC |date=20081020000016 |df=y }}</ref> | |||
== | ===Prevalence=== | ||
*In 2019, around 3.1 million women are living with breast cancer in the United States. | |||
*Approximately 12.3 percent of women will be diagnosed with female breast cancer at some point during their lifetime. | |||
* Worldwide, [[breast cancer]] is the most common invasive cancer in women. (The most common form of cancer is non-invasive [[Skin neoplasm|non-melanoma skin cancer]]; non-invasive cancers are generally easily cured, cause very few deaths, and are routinely excluded from cancer statistics.) Breast cancer comprises 22.9% of invasive cancers in women and 16% of all female cancers.<ref>{{Cite web|url=http://www.who.int/cancer/detection/breastcancer/en/index1.html|title=Breast cancer: prevention and control |work=World Health Organization |accessdate=}}</ref> | |||
* In the United States, breast cancer is the third most common cause of cancer death (after lung cancer and colon cancer). In 2007, breast cancer caused approximately 40,910 deaths (7% of cancer deaths; almost 2% of all deaths) in the U.S.<ref name="acs cancer facts 2007">{{cite web |author=[[American Cancer Society]] |year=2007 |title=Cancer Facts & Figures 2007 |url=http://www.cancer.org/downloads/STT/CAFF2007PWSecured.pdf |accessdate=2007-04-26}}</ref> | |||
* Among women in the U.S., breast cancer is the most common cancer and the second- most common cause of cancer death (after lung cancer). Women in the U.S. have a 1 in 8 lifetime chance of developing invasive breast cancer and a 1 in 33 chance of breast cancer causing their death.<ref name="acs bc key stats">{{cite web |author=[[American Cancer Society]] |month=September 18, |year=2006 |title=What Are the Key Statistics for Breast Cancer? |url=http://www.cancer.org/docroot/CRI/content/CRI_2_4_1X_What_are_the_key_statistics_for_breast_cancer_5.asp |accessdate=2007-04-26}}</ref> A U.S. study conducted in 2005 by the Society for Women's Health Research indicated that breast cancer remains the most feared disease,<ref>{{cite press release |title=Women's Fear of Heart Disease Has Almost Doubled in Three Years, But Breast Cancer Remains Most Feared Disease | publisher=Society for Women's Health Research | date=2005-07-07 | url=http://www.womenshealthresearch.org/site/News2?page=NewsArticle&id=5459&news_iv_ctrl=0&abbr=press_ |accessdate=2007-10-15 }} | |||
</ref> even though [[heart disease]] is a much more common cause of death among women.<ref>{{cite web |url=http://www.nhlbi.nih.gov/health/hearttruth/press/infograph_dressgraph.pdf |title=Leading Causes of Death for American Women 2004 |accessdate=2007-10-15 |format=PDF |work=National Heart Lung and Blood Institute }}</ref> | |||
The | * Since the 1970s, The number of cases has significantly increased, a phenomenon partly blamed on modern lifestyles in the Western world.<ref name="indy">{{cite news | ||
| last = Laurance | |||
| first = Jeremy | |||
| title = Breast cancer cases rise 80% since Seventies | |||
| work = [[The Independent]] | |||
| date = 2006-09-29 | |||
| url = http://news.independent.co.uk/uk/health_medical/article1771835.ece | |||
| accessdate = 2006-10-09 }}</ref><ref>{{cite web | |||
| title = Breast Cancer: Statistics on Incidence, Survival, and Screening | |||
| work = [http://imaginis.com Imaginis Corporation] | |||
| date = 2006 | |||
| url = http://imaginis.com/breasthealth/statistics.asp | |||
| accessdate = 2006-10-09 }}</ref> | |||
* According to the results of the Women’s Health Initiative study ,published in 2002, reduced use of hormone replacement therapy (HRT) by US women might explain the observed decreasing pattern of incidence. | |||
* Because the breast is composed of identical tissues in males and females, breast cancer also occurs in males, although it is less common.<ref name="Dave">{{cite web | |||
| title = Male Breast Cancer Treatment - National Cancer Institute | |||
| work = [http://www.cancer.gov/ National Cancer Institute] | |||
| date = 2006 | |||
| url = http://www.cancer.gov/cancertopics/pdq/treatment/malebreast/healthprofessional | |||
| accessdate = 2006-10-16 }}</ref> | |||
: | |||
=== | ===Case Fatality Rate=== | ||
*Estimated death due to breast cancer in 2018 was 40,920 which made 6.7% of all caner induced death. | |||
*The number of deaths was 21.9 per 100,000 women per year, based on 2010-2012 data. | |||
*A decreasing pattern of death rates has been observed since 1989 which might be explained by treatment advances, earlier cancer detection courtesy of screening programs, and increased awareness. | |||
[[image:Bcid.png|thumb|center|700px|Breast cancer incidence and death rates (1992-2015). [https://seer.cancer.gov/statfacts/html/breast.html Courtesy of SEER data base website. https://seer.cancer.gov/statfacts/html/breast.html]]] | |||
===Age=== | |||
====Invasive Breast Cancer==== | |||
* While the overall age-adjusted [[incidence]] of invasive breast cancer among males and females in the United States between 2007 and 2011 is 67.1 per 100,000, the age-adjusted [[incidence]] of invasive breast cancer by age category is:<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | |||
** Under 65 years: 41.9 per 100,000 | |||
** 65 and over: 241.6 per 100,000 | |||
* Among females, only, the overall age-adjusted [[incidence]] of invasive breast cancer in the United States between 2007 and 2011 is 124.5 per 100,000, whereas the age-adjusted [[incidence]] of invasive breast cancer by age category is:<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | |||
** Under 65 years: 81.7 per 100,000 | |||
** 65 and over: 420.3 per 100,000 | |||
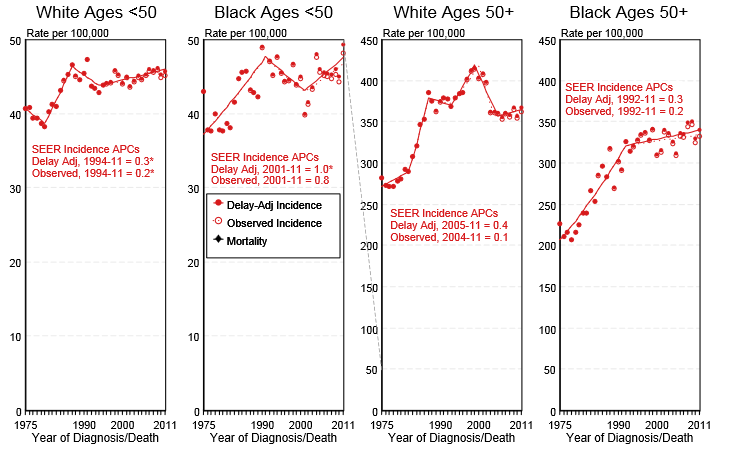
* Shown below is an image depicting the incidence of breast cancer by age and race in the United States between 1975 and 2011.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | |||
[[Image:Incidence of breast cancer by age and race.PNG|Incidence of breast cancer by age and race]] | |||
====In-Situ Breast Cancer==== | |||
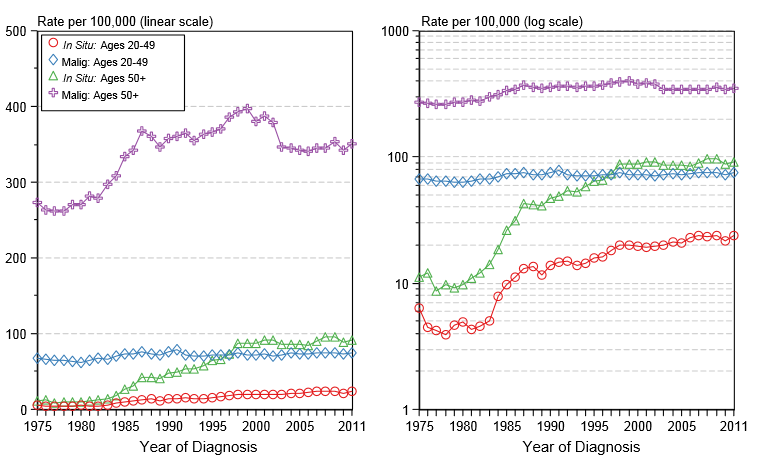
* Among females only, the overall age-adjusted [[incidence]] of in-situ breast cancer in the United States between 2007 and 2011 is 31.7 per 100,000, whereas the age-adjusted [[incidence]] of invasive breast cancer by age category is:<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | |||
** Under 65 years: 23.6 per 100,000 | |||
** 65 and over: 87.7 per 100,000 | |||
* Shown below is an image depicting the [[incidence]] of in-situ versus invasive breast cancer in females in the United States between 1975 and 2011. | |||
[[Image:Incidence of in-situ vs invasive breast cancer by age.PNG|Incidence of in-situ versus invasive breast cancer by age]] | |||
=== | ===Gender=== | ||
* In the United States, the age-adjusted [[prevalence]] of invasive breast cancer by gender in 2011 is:<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | |||
** In males: 8.3 per 100,000 | |||
** In females: 1222.3 per 100,000 | |||
===Sex=== | |||
Men have a lower risk of developing breast cancer (approximately 1.08 per 100,000 men per year), however, this risk appears to be rising.<ref name="Giordano">{{cite journal | last = Giordano | first = Sharon H | authorlink = | coauthors = Cohen DS, Buzdar AU, Perkins G, Hortobagyi GN | title = Breast carcinoma in men | journal = Cancer | volume = 101 | issue = 1 | pages = 51-57 | publisher =American Cancer Society | date = May 2004 | url= http://www3.interscience.wiley.com/cgi-bin/fulltext/108565241/HTMLSTART | doi = | id = | accessdate = }}</ref> | |||
===Race=== | |||
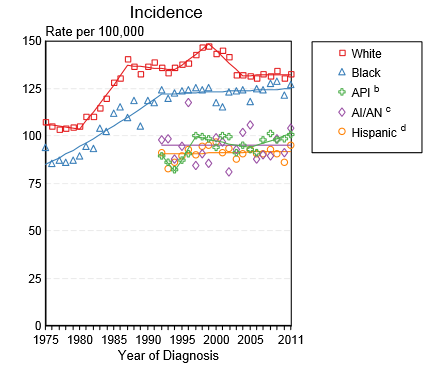
According to the American Cancer Society, between the years of 2008 and 2012, breast cancer incidence rates '''increased''' among black women and Asian/Pacific Islanders. Conversely, incidence rates remained stable amongst white women, Hispanic and American Indian/Alaska Natives, for the same years. | |||
White women have traditionally had the '''highest''' incident rate for breast cancer. However, in '''2012''', the incidence rates for white women and black women converged.<ref name="pmid26513636">DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A (2016) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=26513636 Breast cancer statistics, 2015: Convergence of incidence rates between black and white women.] ''CA Cancer J Clin'' 66 (1):31-42. [http://dx.doi.org/10.3322/caac.21320 DOI:10.3322/caac.21320] PMID: [https://pubmed.gov/26513636 26513636]</ref> | |||
In the 2013 statistics, the incidence rate remains quite close. White women have an incidence rate of '''124.4''' per 100,000 and black women, just a little less at '''122.9''' per 100,000. | |||
Although incidence rates are similar now among black and white women, there remain differences based on [[Ageing|age]] and stage at diagnosis. | |||
Although | |||
[[Image:Breast cancer Incidence by race.png|thumb|center|500px|Breast Cancer incidence rates by race and age group, Courtesy of SEER database]] | |||
* Shown below is a table depicting the age-adjusted [[prevalence]] of invasive breast cancer by race in females and males in 2011 in the United States.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | |||
=== | {| style="cellpadding=0; cellspacing= 0; width: 600px;" | ||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" | || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''All Races''' || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''White''' || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Black''' || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Asian/Pacific Islander''' || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Hispanic''' | |||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Age-adjusted prevalence'''|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |666.3 per 100,000 || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |700.1 per 100,000|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |592.9 per 100,000|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |510.9 per 100,000 || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |460.5 per 100,000 | |||
|} | |||
* Shown below is a table depicting the age-adjusted [[prevalence]] of invasive breast cancer by race in females in in 2011 in the United States.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | |||
==== | {| style="cellpadding=0; cellspacing= 0; width: 600px;" | ||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" | || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''All Races''' || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''White''' || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Black''' || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Asian/Pacific Islander''' || style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Hispanic''' | |||
|- | |||
| style="padding: 0 5px; font-size: 100%; background: #4682B4; color: #FFFFFF; width: 10%" align="center" |'''Age-adjusted prevalence'''|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |1222.3 per 100,000 || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |1300.2 per 100,000|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |1026.1 per 100,000|| style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |916 per 100,000 || style="font-size: 100; padding: 0 5px; background: #B8B8B8" align="left" |835.9 per 100,000 | |||
|} | |||
* Shown below is an image depicting the [[incidence]] of breast cancer by race in the United States between 1975 and 2011.<ref name="SEER">Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.</ref> | |||
[[Image:Incidence of breast cancer per race.PNG|The incidence of breast cancer by race in the United States between 1975 and 2011]] | |||
<small> API: Asian/Pacific Islander; AI/AN: American Indian/ Alaska Native</small> | |||
== | ===Developing Countries=== | ||
*Breast cancer is a major public health issue in less developed countries, such as those in South America. | |||
*Breast cancer is the leading cause of cancer-related deaths in women in countries such as Uruguay, Argentina, and Brazil. | |||
*For example, the expected numbers of new cases and deaths due to breast cancer in South America for the year 2001 were approximately 70,000 and 30,000, respectively.<ref>(Schwartzmann, 2001, p 118)</ref> | |||
*Unfortunately, due to lack of funding and resources, treatment is not always available to those suffering with breast cancer. | |||
==References== | |||
{{reflist|2}} | |||
[[Category:Disease]] | |||
[[Category: | |||
[[Category:Types of cancer]] | [[Category:Types of cancer]] | ||
[[Category:Breast]] | [[Category:Breast]] | ||
[[Category:Oncology]] | |||
[[Category:Hereditary cancers]] | [[Category:Hereditary cancers]] | ||
[[Category:Mature chapter]] | |||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | |||
[[Category:Medicine]] | |||
[[Category:Gynecology]] | |||
[[Category:Surgery]] | |||
Latest revision as of 22:49, 1 May 2019
|
Breast Cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Breast cancer epidemiology and demographics On the Web |
|
American Roentgen Ray Society Images of Breast cancer epidemiology and demographics |
|
Risk calculators and risk factors for Breast cancer epidemiology and demographics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Soroush Seifirad, M.D.[2]Rim Halaby, M.D. [3]; Assistant Editor(s)-In-Chief: Jack Khouri; Mirdula Sharma, MBBS [4]
Overview
The prevalence of breast cancer is approximately 124.8 per 100,000 women per year. The number of deaths was 21.9 per 100,000 women per year, based on 2010-2012 data. About 1 out of 8 women in United states will develop invasive breast cancer. Annually (i . e in 2019) around 268,600 and 62,930 new cases of invasive and non-invasive (in situ) breast cancer are expected to be diagnosed respectively. In men, life time likelihood of developing breast cancer is about 1 in 883. Annually 2,670 new cases of invasive breast cancer are expected to be diagnosed in males. Breast cancer increasing pattern of incidence rates began decreasing after year 2000 in US.
Epidemiology and demographics
- About 1 out of 8 women in United states will develop invasive breast cancer.
- Annually (i . e in 2019) around 268,600 and 62,930 new cases of invasive and non-invasive (in situ) breast cancer are expected to be diagnosed respectively.
- In men, life time likelihood of developing breast cancer is about 1 in 883.
- Annually 2,670 new cases of invasive breast cancer are expected to be diagnosed in males.
- Breast cancer increasing pattern of incidence rates began decreasing after year 2000 in US.
- According to the results of the Women’s Health Initiative study ,published in 2002, reduced use of hormone replacement therapy (HRT) by US women might explain the observed decreasing pattern of incidence.
- Around 42000 women in the U.S. are expected to die annually from breast cancer.
- Women under 50 have experienced larger decreases.
- A decreasing pattern of death rates has been observed since 1989 which might be explained by treatment advances, earlier cancer detection courtesy of screening programs, and increased awareness.[1]
- In the subgroup of women under 45, African-American women breast incidence of breast cancer is higher compared to the white women, and they are more likely to die of breast cancer.
- Asian, Hispanic, and Native-American women, have a lower risk of developing and dying from breast cancer.
Incidence
Age-Adjusted SEER Incidencea Rates, 2011-2015
| Age at Diagnosis | All Races, Females | White Females | Black Females |
|---|---|---|---|
| All ages | 31.1 | 30.8 | 32.1 |
| Under 65 | 23.1 | 22.9 | 21.9 |
| 65 and over | 86.7 | 85.3 | 102.9 |
| All ages (WHO world std)b | 25.3 | 25.0 | 25. |
Age-Specific SEER Incidence Rates, 2011-2015
| Age at Diagnosis | All Races, Females | White Females | Black Females |
|---|---|---|---|
| <1 | - | - | - |
| 1-4 | - | - | - |
| 5-9 | - | - | - |
| 10-14 | - | - | - |
| 15-19 | - | - | - |
| 20-24 | 0.2 | 0.2 | - |
| 25-29 | 0.7 | 0.6 | 0.8 |
| 30-34 | 2.7 | 2.4 | 3.1 |
| 35-39 | 9.6 | 9.7 | 8.6 |
| 40-44 | 40.7 | 40.5 | 34.5 |
| 45-49 | 62.5 | 62.9 | 49.4 |
| 50-54 | 70.5 | 70.6 | 62.9 |
| 55-59 | 73.1 | 71.4 | 79.2 |
| 60-64 | 86.6 | 84.0 | 101.7 |
| 65-69 | 108.4 | 105.9 | 122.0 |
| 70-74 | 103.4 | 101.1 | 123.2 |
| 75-79 | 88.0 | 87.0 | 112.8 |
| 80-84 | 64.3 | 64.2 | 74.9 |
| 85+ | 28.4 | 28.2 | 34.4 |
Footnotes: a SEER 18 areas. Rates are per 100,000 and are age-adjusted to the 2000 US Std Population (19 age groups - Census P25-1130), unless noted.
b Rates are per 100,000 and are age-adjusted to the world (WHO 2000-2025) standard million.
- Statistic not shown. Rate based on less than 16 cases for the time interval.
- Estimated new breast cancer cases in 2018 was 266,120 which made 15% of all new caner cases.
- The incidence of breast cancer varies greatly around the world: it is lowest in less-developed countries and greatest in the more-developed countries.
- In the twelve world regions, the annual age-standardized incidence rates per 100,000 women are as follows:
- in Eastern Asia,18;
- South Central Asia, 22;
- Sub-Saharan Africa, 22;
- South-Eastern Asia, 26;
- North Africa and Western Asia, 28;
- South and Central America, 42;
- Eastern Europe, 49;
- Southern Europe, 56;
- Northern Europe, 73;
- Oceania, 74;
- Western Europe, 78;
- and in North America, 90.[2]
Prevalence
- In 2019, around 3.1 million women are living with breast cancer in the United States.
- Approximately 12.3 percent of women will be diagnosed with female breast cancer at some point during their lifetime.
- Worldwide, breast cancer is the most common invasive cancer in women. (The most common form of cancer is non-invasive non-melanoma skin cancer; non-invasive cancers are generally easily cured, cause very few deaths, and are routinely excluded from cancer statistics.) Breast cancer comprises 22.9% of invasive cancers in women and 16% of all female cancers.[3]
- In the United States, breast cancer is the third most common cause of cancer death (after lung cancer and colon cancer). In 2007, breast cancer caused approximately 40,910 deaths (7% of cancer deaths; almost 2% of all deaths) in the U.S.[4]
- Among women in the U.S., breast cancer is the most common cancer and the second- most common cause of cancer death (after lung cancer). Women in the U.S. have a 1 in 8 lifetime chance of developing invasive breast cancer and a 1 in 33 chance of breast cancer causing their death.[5] A U.S. study conducted in 2005 by the Society for Women's Health Research indicated that breast cancer remains the most feared disease,[6] even though heart disease is a much more common cause of death among women.[7]
- Since the 1970s, The number of cases has significantly increased, a phenomenon partly blamed on modern lifestyles in the Western world.[8][9]
- According to the results of the Women’s Health Initiative study ,published in 2002, reduced use of hormone replacement therapy (HRT) by US women might explain the observed decreasing pattern of incidence.
- Because the breast is composed of identical tissues in males and females, breast cancer also occurs in males, although it is less common.[10]
Case Fatality Rate
- Estimated death due to breast cancer in 2018 was 40,920 which made 6.7% of all caner induced death.
- The number of deaths was 21.9 per 100,000 women per year, based on 2010-2012 data.
- A decreasing pattern of death rates has been observed since 1989 which might be explained by treatment advances, earlier cancer detection courtesy of screening programs, and increased awareness.

Age
Invasive Breast Cancer
- While the overall age-adjusted incidence of invasive breast cancer among males and females in the United States between 2007 and 2011 is 67.1 per 100,000, the age-adjusted incidence of invasive breast cancer by age category is:[11]
- Under 65 years: 41.9 per 100,000
- 65 and over: 241.6 per 100,000
- Among females, only, the overall age-adjusted incidence of invasive breast cancer in the United States between 2007 and 2011 is 124.5 per 100,000, whereas the age-adjusted incidence of invasive breast cancer by age category is:[11]
- Under 65 years: 81.7 per 100,000
- 65 and over: 420.3 per 100,000
- Shown below is an image depicting the incidence of breast cancer by age and race in the United States between 1975 and 2011.[11]
In-Situ Breast Cancer
- Among females only, the overall age-adjusted incidence of in-situ breast cancer in the United States between 2007 and 2011 is 31.7 per 100,000, whereas the age-adjusted incidence of invasive breast cancer by age category is:[11]
- Under 65 years: 23.6 per 100,000
- 65 and over: 87.7 per 100,000
- Shown below is an image depicting the incidence of in-situ versus invasive breast cancer in females in the United States between 1975 and 2011.
Gender
- In the United States, the age-adjusted prevalence of invasive breast cancer by gender in 2011 is:[11]
- In males: 8.3 per 100,000
- In females: 1222.3 per 100,000
Sex
Men have a lower risk of developing breast cancer (approximately 1.08 per 100,000 men per year), however, this risk appears to be rising.[12]
Race
According to the American Cancer Society, between the years of 2008 and 2012, breast cancer incidence rates increased among black women and Asian/Pacific Islanders. Conversely, incidence rates remained stable amongst white women, Hispanic and American Indian/Alaska Natives, for the same years.
White women have traditionally had the highest incident rate for breast cancer. However, in 2012, the incidence rates for white women and black women converged.[13]
In the 2013 statistics, the incidence rate remains quite close. White women have an incidence rate of 124.4 per 100,000 and black women, just a little less at 122.9 per 100,000.
Although incidence rates are similar now among black and white women, there remain differences based on age and stage at diagnosis.

- Shown below is a table depicting the age-adjusted prevalence of invasive breast cancer by race in females and males in 2011 in the United States.[11]
| All Races | White | Black | Asian/Pacific Islander | Hispanic | |
| Age-adjusted prevalence | 666.3 per 100,000 | 700.1 per 100,000 | 592.9 per 100,000 | 510.9 per 100,000 | 460.5 per 100,000 |
- Shown below is a table depicting the age-adjusted prevalence of invasive breast cancer by race in females in in 2011 in the United States.[11]
| All Races | White | Black | Asian/Pacific Islander | Hispanic | |
| Age-adjusted prevalence | 1222.3 per 100,000 | 1300.2 per 100,000 | 1026.1 per 100,000 | 916 per 100,000 | 835.9 per 100,000 |
- Shown below is an image depicting the incidence of breast cancer by race in the United States between 1975 and 2011.[11]
API: Asian/Pacific Islander; AI/AN: American Indian/ Alaska Native
Developing Countries
- Breast cancer is a major public health issue in less developed countries, such as those in South America.
- Breast cancer is the leading cause of cancer-related deaths in women in countries such as Uruguay, Argentina, and Brazil.
- For example, the expected numbers of new cases and deaths due to breast cancer in South America for the year 2001 were approximately 70,000 and 30,000, respectively.[14]
- Unfortunately, due to lack of funding and resources, treatment is not always available to those suffering with breast cancer.
References
- ↑ "Cancer Statistics Review, 1975-2015 - SEER Statistics".
- ↑ Stewart B. W. and Kleihues P. (Eds): World Cancer Report. IARCPress. Lyon 2003 Template:Wayback
- ↑ "Breast cancer: prevention and control". World Health Organization.
- ↑ American Cancer Society (2007). "Cancer Facts & Figures 2007" (PDF). Retrieved 2007-04-26.
- ↑ American Cancer Society (2006). "What Are the Key Statistics for Breast Cancer?". Retrieved 2007-04-26. Unknown parameter
|month=ignored (help) - ↑ "Women's Fear of Heart Disease Has Almost Doubled in Three Years, But Breast Cancer Remains Most Feared Disease" (Press release). Society for Women's Health Research. 2005-07-07. Retrieved 2007-10-15.
- ↑ "Leading Causes of Death for American Women 2004" (PDF). National Heart Lung and Blood Institute. Retrieved 2007-10-15.
- ↑ Laurance, Jeremy (2006-09-29). "Breast cancer cases rise 80% since Seventies". The Independent. Retrieved 2006-10-09.
- ↑ "Breast Cancer: Statistics on Incidence, Survival, and Screening". Imaginis Corporation. 2006. Retrieved 2006-10-09. External link in
|work=(help) - ↑ "Male Breast Cancer Treatment - National Cancer Institute". National Cancer Institute. 2006. Retrieved 2006-10-16. External link in
|work=(help) - ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 11.7 Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.
- ↑ Giordano, Sharon H (May 2004). "Breast carcinoma in men". Cancer. American Cancer Society. 101 (1): 51–57. Unknown parameter
|coauthors=ignored (help) - ↑ DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A (2016) Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA Cancer J Clin 66 (1):31-42. DOI:10.3322/caac.21320 PMID: 26513636
- ↑ (Schwartzmann, 2001, p 118)