Zygomycosis case study one
|
Zygomycosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Zygomycosis case study one On the Web |
|
American Roentgen Ray Society Images of Zygomycosis case study one |
|
Risk calculators and risk factors for Zygomycosis case study one |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Case Studies
Clinical Summary
A 63-year-old white male was in his usual state of good health until eight weeks before his death when he developed sudden onset of shortness of breath. A thoracotomy was performed for plication of ruptured emphysematous blebs.
Following improvement and discharge from the hospital he developed weakness, lethargy, and a left lower lobe lung infiltrate. The patient's condition soon deteriorated further, with almost every organ system having failed. The patient developed DIC and peripheral embolic phenomena, including gangrene of his extremities and face.
A single antemortem blood culture grew Staphylococcus aureus.
Postmortem Findings
Autopsy revealed severe emphysema, severe widespread abscessiform and necrotizing pneumonia, and bacterial endocarditis (Staphylococcus aureus) of the pulmonic valve. The right internal carotid artery was occluded by a thrombus and there were areas of necrosis (due to CVAs) in the brain.
-
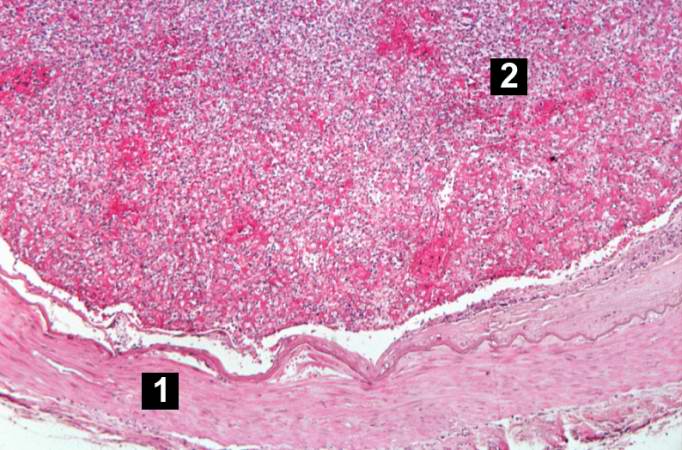
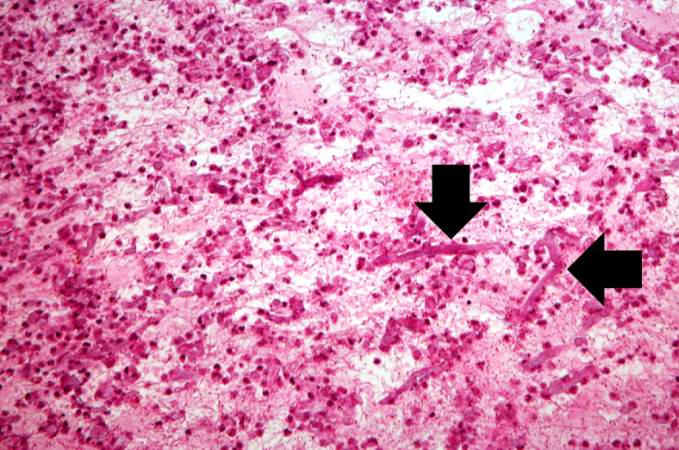
This is a low-power photomicrograph of a section of carotid artery containing a mural thrombus.
-
This is a higher-power photomicrograph of the wall of the carotid artery (1) and the thrombus (2).
-
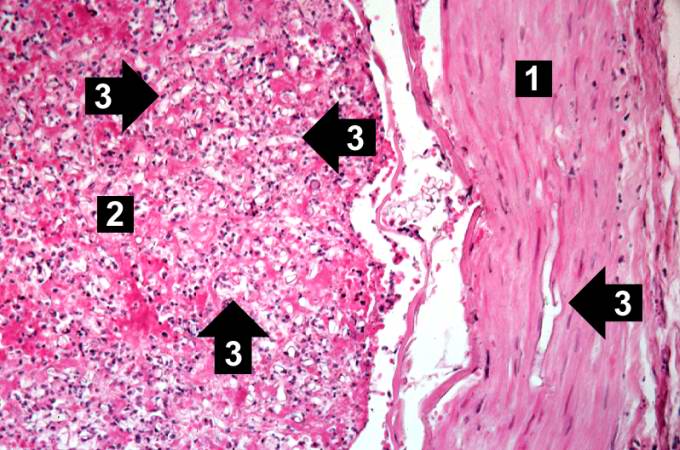
This is an even higher-power photomicrograph of the wall of the carotid artery (1) and the thrombus (2). Within the wall of the artery and in the thrombus there are multiple variably shaped clear areas (3). At this magnification and with this stain, it is impossible to determine what these clear spaces represent.
-
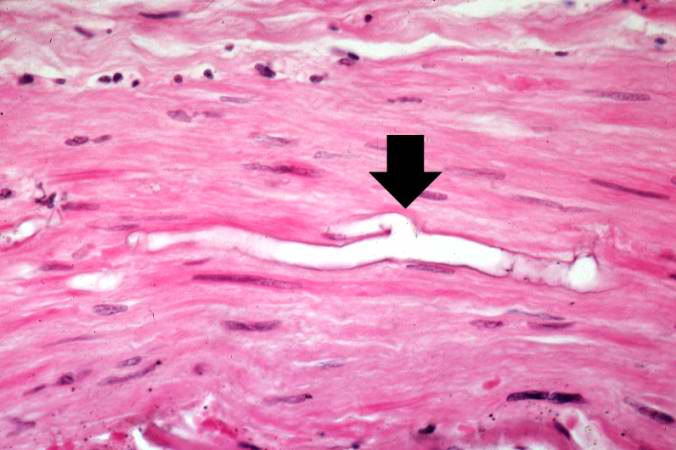
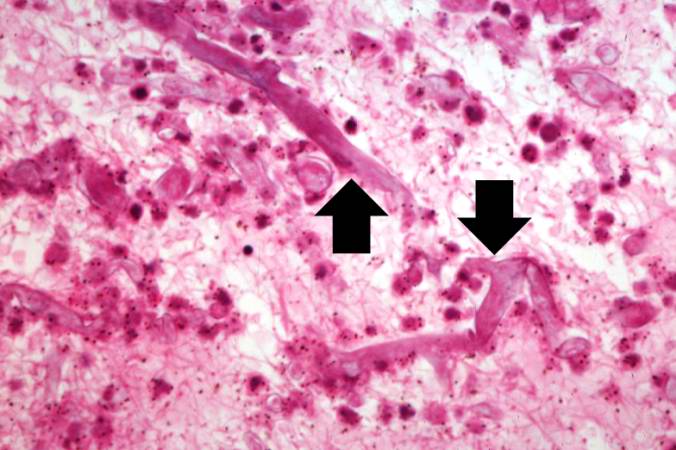
This is a higher-power photomicrograph of just the wall of the carotid artery. Note the ribbon-like clear structure with roughly parallel walls (non-septate hyphae) and right-angle branching (arrow). This is the Mucor organism.
-
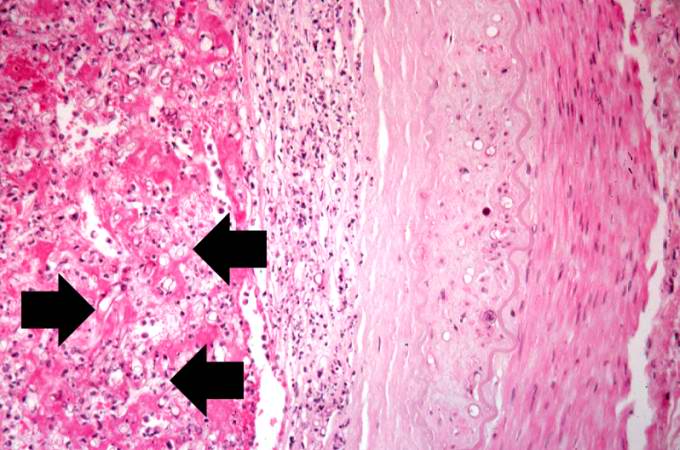
This is another high-power photomicrograph of the wall of the artery and the thrombus. Within the thrombus there are multiple variably-shaped clear areas that represent longitudinal sections and cross sections of the Mucor organisms (arrows).
-
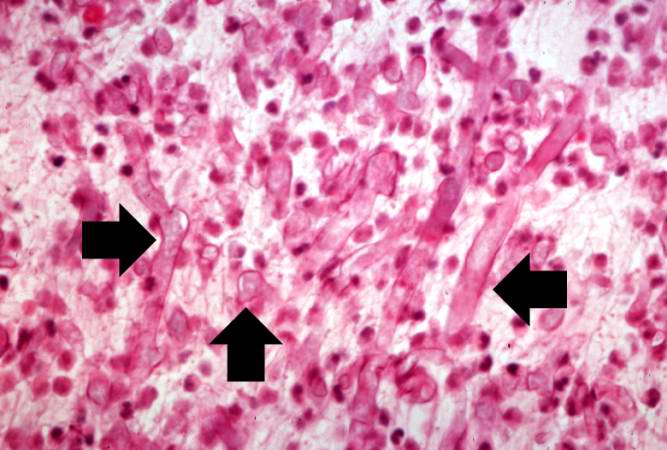
This medium-power photomicrograph shows the thrombus stained to outline the Mucor organisms (arrows). Note again the ribbon-like morphology and the wide-angle branching.
-
This is an even higher-power photomicrograph of the thrombus stained to outline the Mucor organisms (arrows).
-
This is another high-power photomicrograph of the thrombus stained to outline the Mucor organisms (arrows).