Posterior myocardial infarction
|
ST Elevation Myocardial Infarction Microchapters |
|
Differentiating ST elevation myocardial infarction from other Diseases |
|
Diagnosis |
|
Treatment |
|
|
Case Studies |
|
Posterior myocardial infarction On the Web |
|
Directions to Hospitals Treating ST elevation myocardial infarction |
|
Risk calculators and risk factors for Posterior myocardial infarction |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: posterior MI, true posterior MI
Overview
A posterior myocardial infarction (MI) is a heart attack or cessation of blood flow to the heart muscle that involves the backside or posterior side of the heart. Rather than causing the traditional ST segment elevation characteristic of the electrocardiogram of many heart attacks (a "STEMI"), because the heart attack is on the opposite side of the heart, the ST segments are depressed in the anterior precordial leads rather than elevated.
Pathophysiology
A posterior MI is due to occlusion of the left circumflex artery.
EKG Findings
EKG findings in the precordial leads V1-V3:
- ST segment depression[1]
- Tall R waves (equivalent of Q wave)
- Upright T waves
EKG Examples
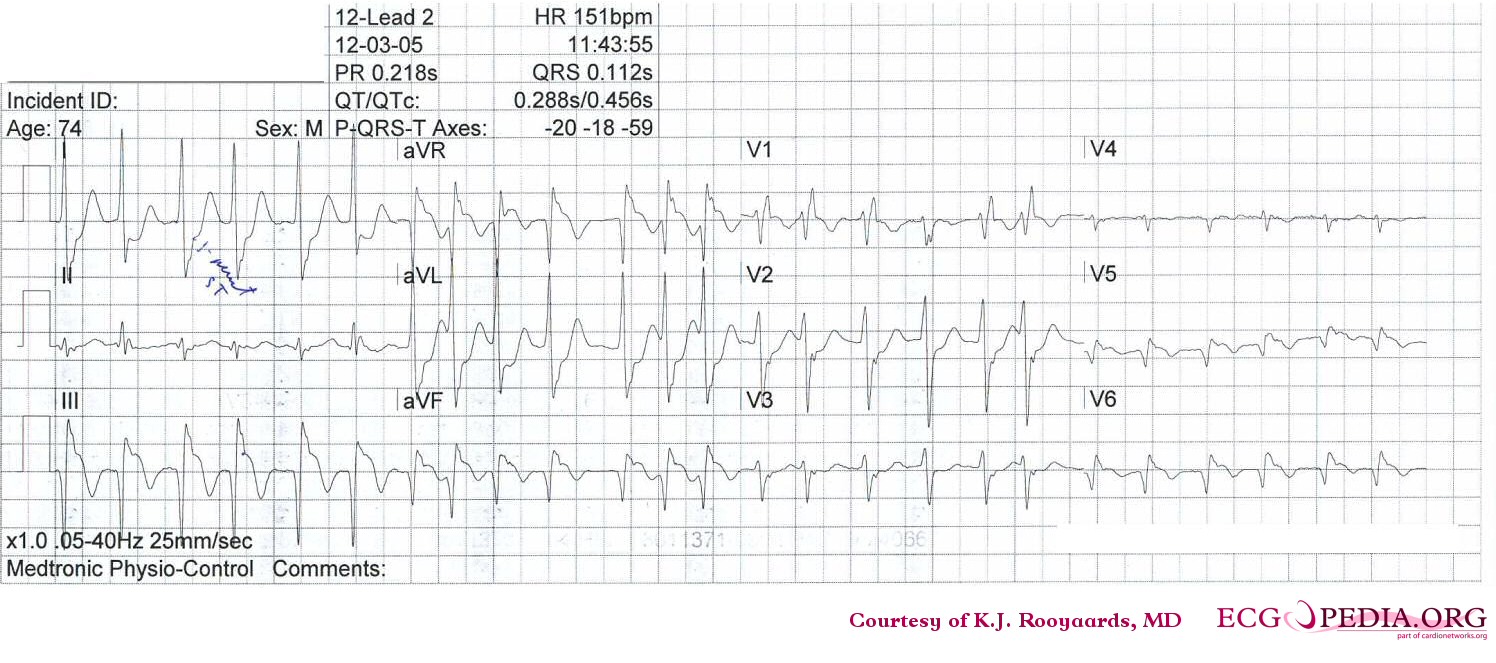
Shown below is an EKG demonstrating changes during acute posterolateral MI depicting ST depression in precordial leads V2-V3.
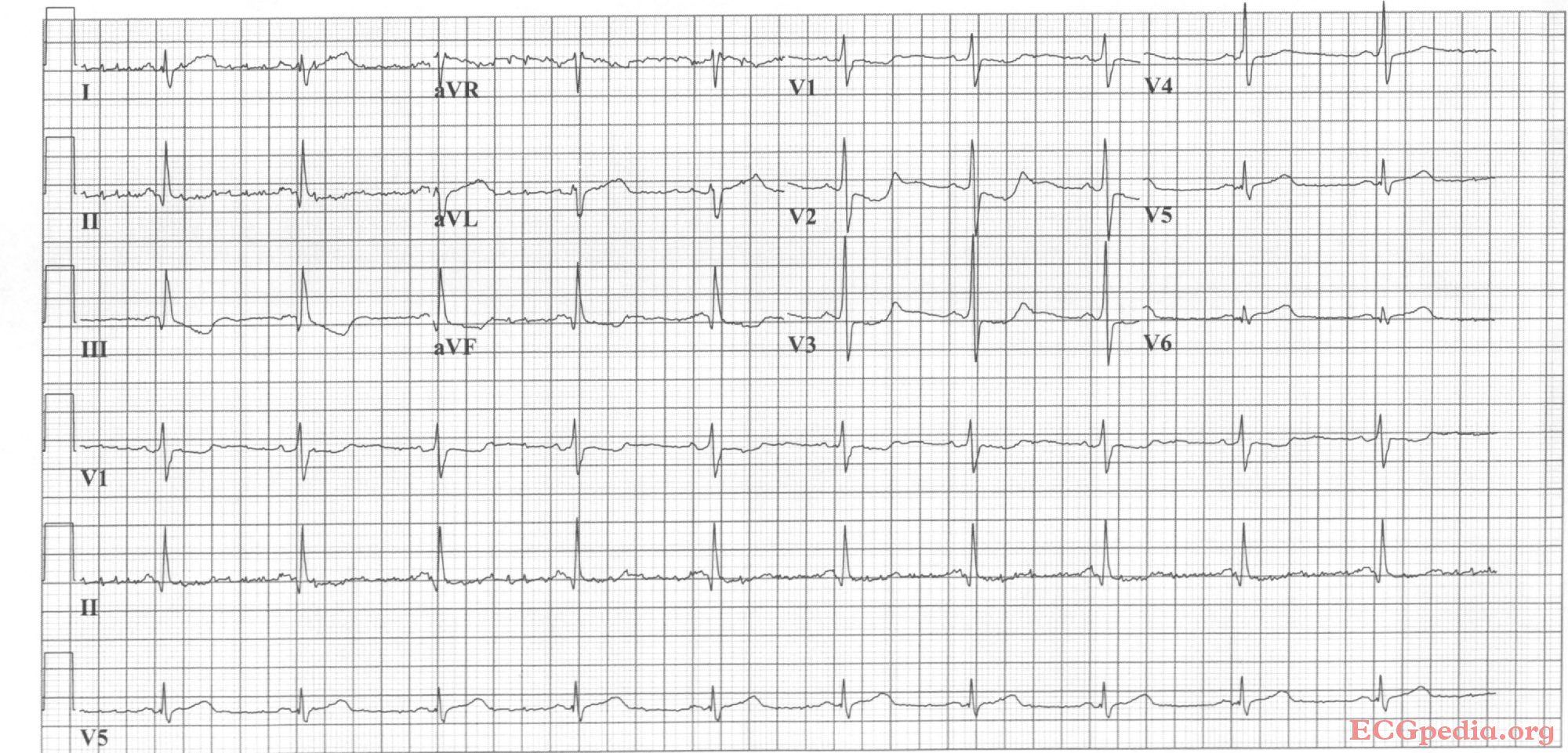
Copyleft image obtained courtesy of, http://en.ecgpedia.org/wiki/Main_Page
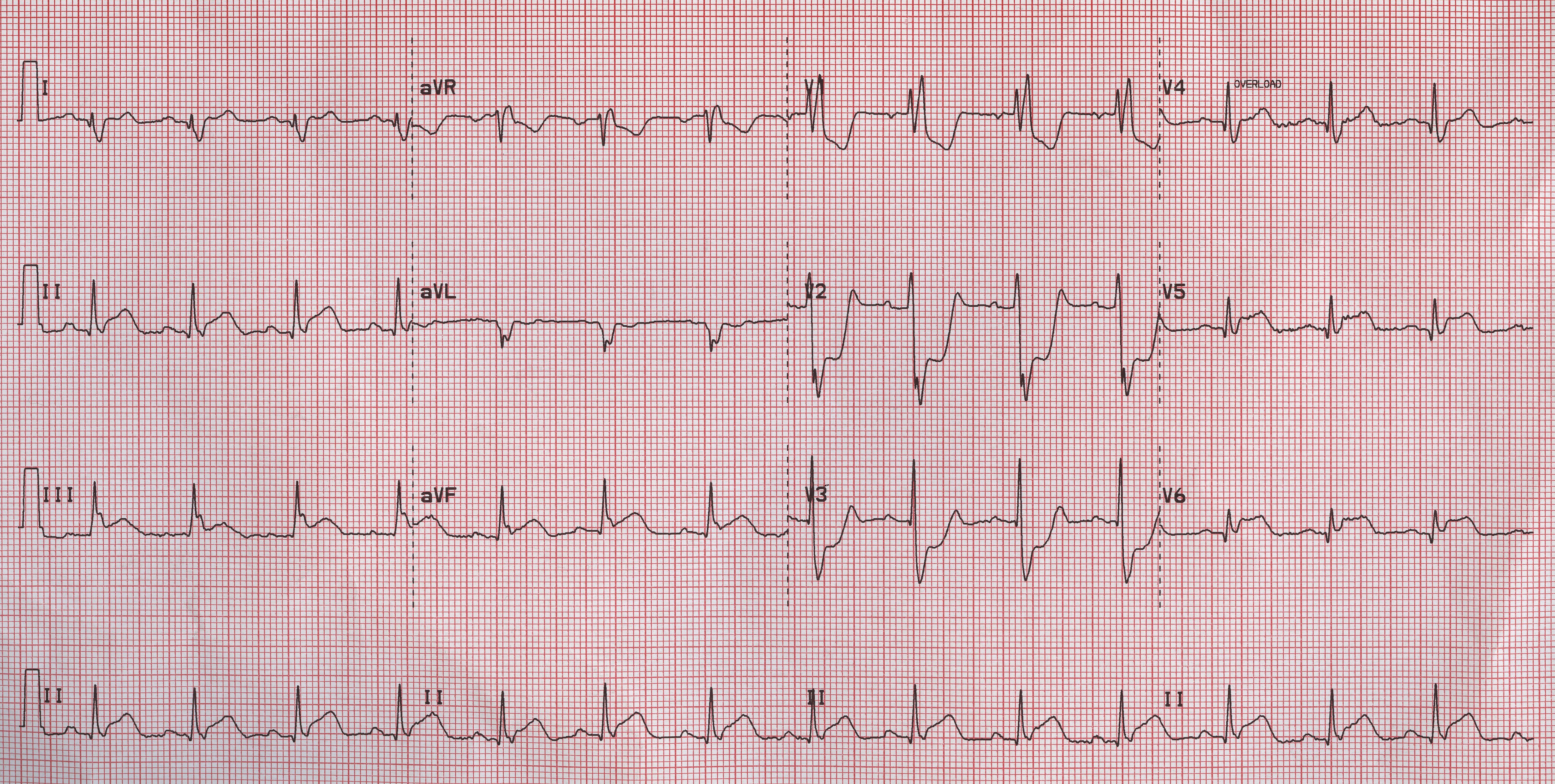
Shown below is an EKG illustrating inferior-posterior myocardial infarction with complete AV block and ventricular escape rhythm with RBBB pattern and left axis, followed by sinus rhythm.
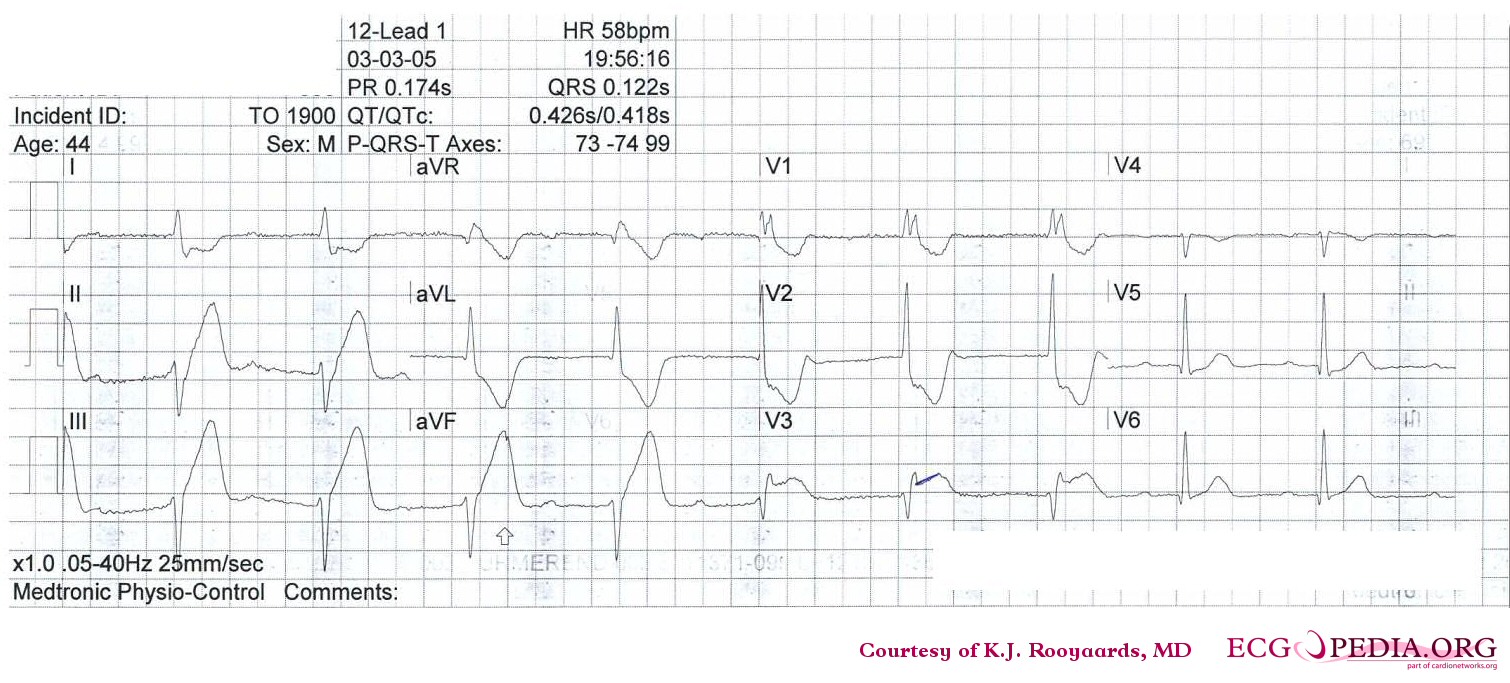
Copyleft image obtained courtesy of, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an EKG demonstrating atrial fibrillation and inferior-posterior myocardial infarction.
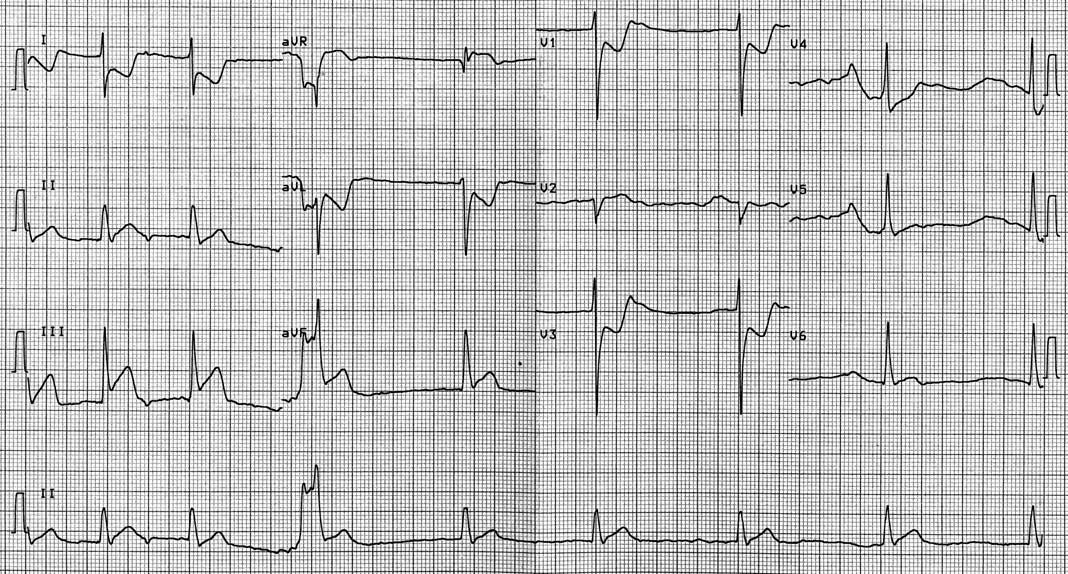
Copyleft image obtained courtesy of, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an EKG demonstrating inferior-posterior-lateral myocardial infarction with a nodal escape rhythm
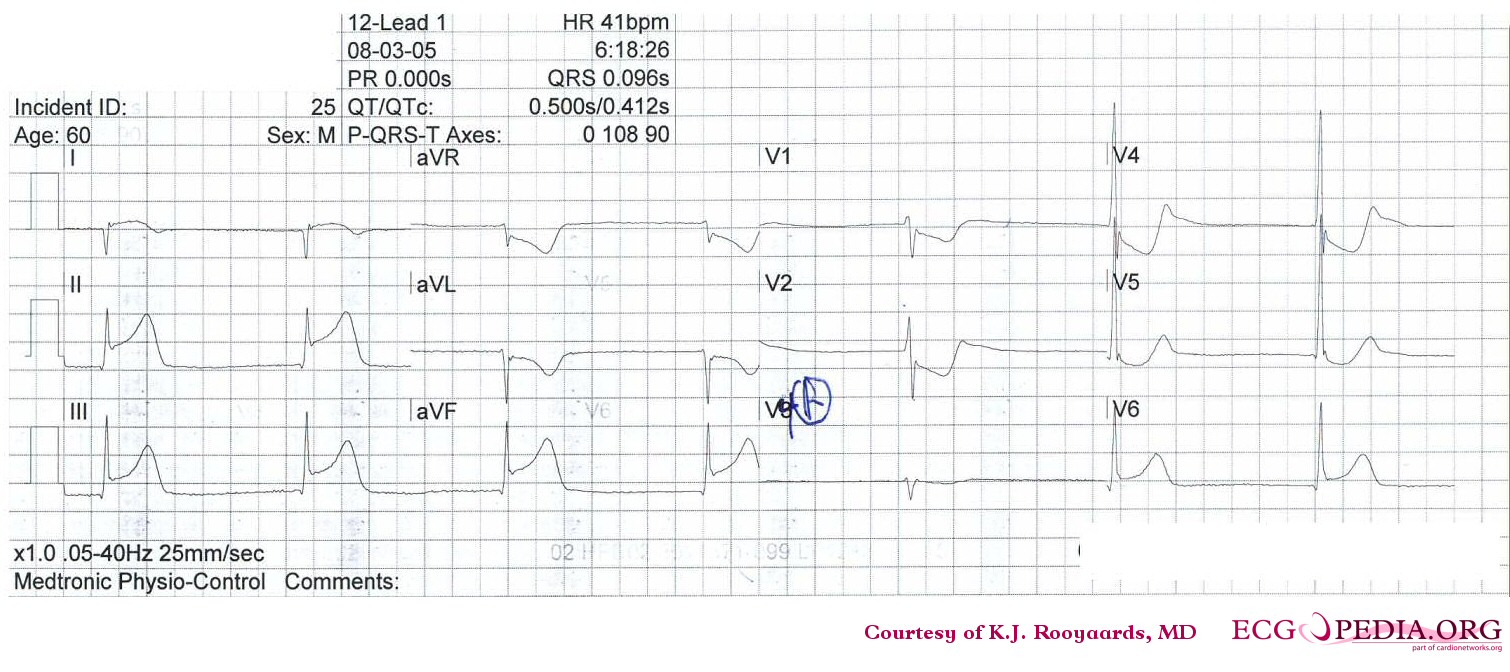
Copyleft image obtained courtesy of, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an EKG demonstrating atrial fibrillation with inferior-posterior-lateral myocardial infarction and incomplete right bundle branch block. Lead I shows ST depression, suggestive of right coronary artery involvement.
Copyleft image obtained courtesy of, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an EKG demonstrating ST elevation in leads II, III and aVF and ST depression in leads V1, V2 and V3 depicting a posterior MI.
Angiography
Posterior MI results from the total occlusion of either the right coronary artery or the left circumflex.
Shown below are an animated image and a static image depicting PERFUSE grade 6 thrombus in the RCA. Encircled in yellow in the image on the right is the thrombus area where you can notice an abrupt blunt cut-off appearance beyond which no dye is penetrating the artery.
Shown below are two animated images of the same case depicting TIMI grade 6 thrombus in the left circumflex. The image on the left shows the same thrombus before PCI and the image on the left shows the patent left circumflex after PCI.
References
- ↑ Pride YB, Tung P, Mohanavelu S, Zorkun C, Wiviott SD, Antman EM; et al. (2010). "Angiographic and clinical outcomes among patients with acute coronary syndromes presenting with isolated anterior ST-segment depression: a TRITON-TIMI 38 (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition With Prasugrel-Thrombolysis In Myocardial Infarction 38) substudy". JACC Cardiovasc Interv. 3 (8): 806–11. doi:10.1016/j.jcin.2010.05.012. PMID 20723851.