Theophylline
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Theophylline is an anti-asthmatic that is FDA approved for the treatment of is indicated for the treatment of the symptoms and reversible airflow obstruction associated with chronic asthma and other chronic lung diseases, e.g., emphysema and chronic bronchitis.. Common adverse reactions include vomiting, diarrhea, abdominal pain, hematemesis, acid-base disturbances, rhabdomyolysis, supraventricular tachycardia, shock, nervousness, tremors, disorientation and seziures.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
General Considerations
- The steady-state peak serum theophylline concentration is a function of the dose, the dosing interval, and the rate of theophylline absorption and clearance in the individual patient.
- Because of marked individual differences in the rate of theophylline clearance, the dose required to achieve a peak serum theophylline concentration in the 10-20 mcg/mL range varies fourfold among otherwise similar patients in the absence of factors known to alter theophylline clearance (e.g., 400-1600 mg/day in adults <60 years old and 10-36 mg/kg/day in children 1-9 years old).
- For a given population there is no single theophylline dose that will provide both safe and effective serum concentrations for all patients.
- Administration of the median theophylline dose required to achieve a therapeutic serum theophylline concentration in a given population may result in either sub-therapeutic or potentially toxic serum theophylline concentrations in individual patients.
- For example, at a dose of 900 mg/d in adults <60 years or 22 mg/kg/d in children 1-9 years, the steady state peak serum theophylline concentration will be <10 mcg/mL in about 30% of patients, 10-20 mcg/mL in about 50% and 20-30 mcg/mL in about 20% of patients.
- The dose of theophylline must be individualized on the basis of peak serum theophylline concentration measurements in order to achieve a dose that will provide maximum potential benefit with minimal risk to adverse effects.
- Transient caffeine-like adverse effects and excessive serum concentrations in slow metabolizers can be avoided in most patients by starting with a sufficiently low dose and slowly increasing the dose, if judged to be clinically indicated, in small increments (See Table V).
- Dose increases should only be made if the previous dosage is well tolerated and at intervals of no less than 3 days to allow serum theophylline concentrations to reach the new steady state. Dosage adjustment should be guided by serum theophylline concentration measurement.
- Health care providers should instruct patients and care givers to discontinue any dosage that causes adverse effects, to withhold the medication until these symptoms are gone and to then resume therapy at a lower, previously tolerated dosage.
- If the patient’s symptoms are well controlled, there are no apparent adverse effects, and no intervening factors that might alter dosage requirements , serum theophylline concentrations should be monitored at 6 month intervals for rapidly growing children and at yearly intervals for all others.
- In acutely ill patients, serum theophylline concentrations should be monitored at frequent intervals, e.g., every 24 hours.
- Theophylline distributes poorly into body fat, therefore, mg/kg dose should be calculated on the basis of ideal body weight.
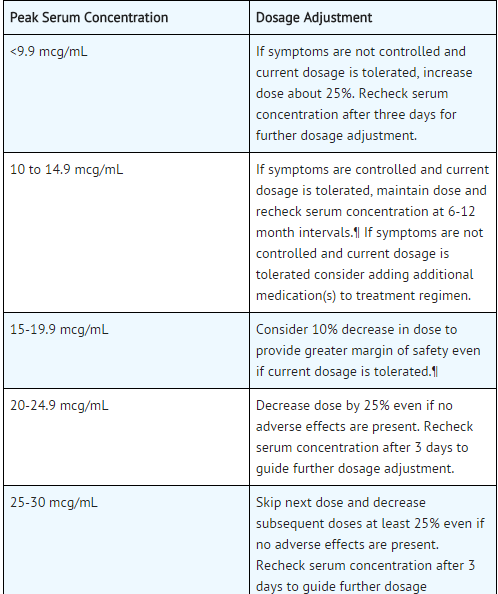
- Table V contains theophylline dosing titration schema recommended for patients in various age groups and clinical circumstances. Table VI contains recommendations for theophylline dosage adjustment based upon serum theophylline concentrations.
- Application of these general dosing recommendations to individual patients must take into account the unique clinical characteristics of each patient.
- In general, these recommendations should serve as the upper limit for dosage adjustments in order to decrease the risk of potentially serious adverse events associated with unexpected large increases in serum theophylline concentration.
Infants <1 year old
Initial Dosage
- Premature Neonates
- < 24 days postnatal age; 1.0 mg/kg every 12 hr
- >24 days postnatal age; 1.5 mg/kg every 12 hr
- Full term infants and infants up to 52 weeks of age:
- Total daily dose (mg) = [(0.2 x age in weeks)+5.0] x (Kg body Wt).
- Up to age 26 weeks; divide dose into 3 equal amounts administered at 8 hour intervals.
- >26 weeks of age; divide dose into 4 equal amounts administered at 6 hour intervals.
- Final Dosage.
- Adjusted to maintain a peak steady state serum theophylline concentration of 5-10 mcg/ml in neonates and 10-15 mcg/mL in older infants (see Table VI). :* Since the time required to reach steady-state is a function of theophylline half-life, up to 5 days may be required to achieve steady state in a premature neonate while only 2-3 days may be required in a 6 month old infant without other risk factors for impaired clearance in the absence of a loading dose.
- If a serum theophylline concentration is obtained before steady state is achieved, the maintenance dose should not be increased, even if the serum theophylline concentration is <10 mcg/mL.
This image is provided by the National Library of Medicine.
Patients With Risk Factors For Impaired Clearance, The Elderly (>60 Years), And Those In Whom It Is Not Feasible To Monitor Serum Theophylline Concentrations
- In children 1-15 years of age, the final theophylline dose should not exceed 16 mg/kg/day up to a maximum of 400 mg/day in the presence of risk factors for reduced theophylline clearance (see WARNINGS) or if it is not feasible to monitor serum theophylline concentrations.
- In adolescents ≥16 years and adults, including the elderly, the final theophylline dose should not exceed 400 mg/day in the presence of risk factors for reduced theophylline clearance (see WARNINGS) or if it is not feasible to monitor serum theophylline concentrations.
Loading Dose for Acute Bronchodilatation
- An inhaled beta-2 selective agonist, alone or in combination with a systemically administered corticosteroid, is the most effective treatment for acute exacerbations of reversible airways obstruction.
- Theophylline is a relatively weak bronchodilator, is less effective than an inhaled beta-2 selective agonist and provides no added benefit in the treatment of acute bronchospasm.
- If an inhaled or parenteral beta agonist is not available, a loading dose of an oral immediate release theophylline can be used as a temporary measure. * A single 5 mg/kg dose of theophylline, in a patient who has not received any theophylline in the previous 24 hours, will produce an average peak serum theophylline concentration of 10 mcg/mL (range 5-15 mcg/mL).
- If dosing with theophylline is to be continued beyond the loading dose, the guidelines in Sections A.1.b., B.3, or C., above, should be utilized and serum theophylline concentration monitored at 24 hour intervals to adjust final dosage.
- Patients with more rapid metabolism, clinically identified by higher than average dose requirements, should receive a smaller dose more frequently to prevent breakthrough symptoms resulting from low trough concentrations before the next dose.
- A reliably absorbed slow-release formulation will decrease fluctuations and permit longer dosing intervals.
This image is provided by the National Library of Medicine. 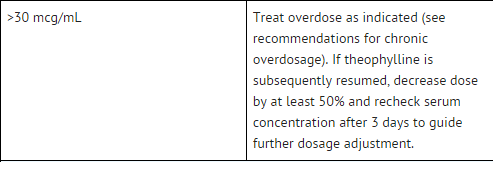
This image is provided by the National Library of Medicine.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Theophylline in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Theophylline in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Theophylline in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Theophylline in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Theophylline in pediatric patients.
Contraindications
- ELIXOPHYLLIN Elixir is contraindicated in patients with a history of hypersensitivity to theophylline or other components in the product.
Warnings
Concurrent Illness
- Theophylline should be used with extreme caution in patients with the following clinical conditions due to the increased risk of exacerbation of the concurrent condition:
- Active peptic ulcer disease
- Seizure disorders
- Cardiac arrhythmias (not including bradyarrhythmias)
- Conditions That Reduce Theophylline Clearance:
- Age
- Neonates (term and premature)
- Children <1 year
- Elderly (>60 years)
- Concurrent Diseases
- Acute pulmonary edema
- Congestive heart failure
- Cor pulmonale
- Fever; ≥102oF for 24 hours or more; or lesser temperature elevations for longer periods
- Hypothyroidism
- Liver disease; cirrhosis, acute hepatitis
- Reduced renal function in infants <3 months of age
- Sepsis with multi-organ failure
- Shock
- Cessation of Smoking
- Drug Interactions Adding a drug that inhibits theophylline metabolism (e.g., cimetidine, erythromycin, tacrine) or stopping a concurrently administered drug that enhances theophylline metabolism (e.g., carbamazepine, rifampin).
When Signs or Symptoms of Theophylline Toxicity Are Present
- Whenever a patient receiving theophylline develops nausea or vomiting, particularly repetitive vomiting, or other signs or symptoms consistent with theophylline toxicity (even if another cause may be suspected), additional doses of theophylline should be withheld and a serum theophylline concentration measured immediately.
- Patients should be instructed not to continue any dosage that causes adverse effects and to withhold subsequent doses until the symptoms have resolved, at which time the clinician may instruct the patient to resume the drug at a lower dosage
Dosage Increases
- Increases in the dose of theophylline should not be made in response to an acute exacerbation of symptoms of chronic lung disease since theophylline provides little added benefit to inhaled beta2-selective agonists and systemically administered corticosteroids in this circumstance and increases the risk of adverse effects.
- A peak steady state serum theophylline concentration should be measured before increasing the dose in response to persistent chronic symptoms to ascertain whether an increase in dose is safe.
- Before increasing the theophylline dose on the basis of a low serum concentration, the clinician should consider whether the blood sample was obtained at an appropriate time in relationship to the dose and whether the patient has adhered to the prescribed regimen.
- As the rate of theophylline clearance may be dose-dependent (i.e., steady-state serum concentrations may increase disproportionately to the increase in dose), an increase in dose based upon a sub-therapeutic serum concentration measurement should be conservative.
- In general, limiting dose increases to about 25% of the previous total daily dose will reduce the risk of unintended excessive increases in serum theophylline concentration.
Adverse Reactions
Clinical Trials Experience
- Adverse reactions associated with theophylline are generally mild when peak serum theophylline concentrations are <20 mcg/mL and mainly consist of transient caffeine-like adverse effects such as nausea, vomiting, headache, and insomnia.
- When peak serum theophylline concentrations exceed 20 mcg/mL, however, theophylline produces a wide range of adverse reactions including persistent vomiting, cardiac arrhythmias, and intractable seizures which can be lethal. * The transient caffeine-like adverse reactions occur in about 50% of patients when theophylline therapy is initiated at doses higher than recommended initial doses (e.g., >300 mg/day in adults and >12 mg/kg/day in children beyond >1 year of age).
- During the initiation of theophylline therapy, caffeine-like adverse effects may transiently alter patient behavior, especially in school age children, but this response rarely persists.
- Initiation of theophylline therapy at a low dose with subsequent slow titration to a predetermined age-related maximum dose will significantly reduce the frequency of these transient adverse effects (see DOSAGE AND ADMINISTRATION , TABLE V).
- In a small percentage of patients (<3% of children and <10% of adults) the caffeine-like adverse effects persist during maintenance therapy, even at peak serum theophylline concentrations within the therapeutic range (i.e., 10-20 mcg/mL).
- Dosage reduction may alleviate the caffeine-like adverse effects in these patients, however, persistent adverse effects should result in a reevaluation of the need for continued theophylline therapy and the potential therapeutic benefit of alternative treatment.
- Other adverse reactions that have been reported at serum theophylline concentrations <20 mcg/mL include diarrhea, irritability, restlessness, fine skeletal muscle tremors, and transient diuresis.
- In patients with hypoxia secondary to COPD, multifocal atrial tachycardia and flutter have been reported at serum theophylline concentrations ≥15 mcg/mL.
- There have been a few isolated reports of seizures at serum theophylline concentrations <20 mcg/mL in patients with an underlying neurological disease or in elderly patients.
- The occurrence of seizures in elderly patients with serum theophylline concentrations <20 mcg/mL may be secondary to decreased protein binding resulting in a larger proportion of the total serum theophylline concentration in the pharmacologically active unbound form.
- The clinical characteristics of the seizures reported in patients with serum theophylline concentrations <20 mcg/mL have generally been milder than seizures associated with excessive serum theophylline concentrations resulting from an overdose (i.e., they have generally been transient, often stopped without anticonvulsant therapy, and did not result in neurological residua).
This image is provided by the National Library of Medicine. 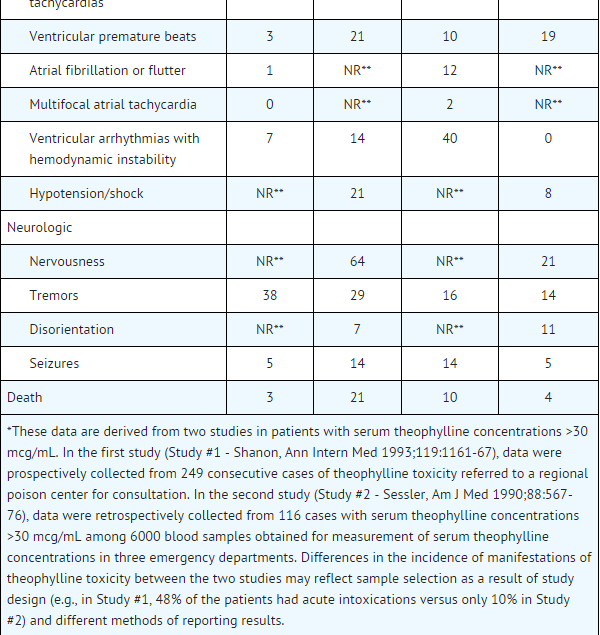
This image is provided by the National Library of Medicine.
Cardiovascular
Digestive
Endocrine
Hematologic and Lymphatic
Metabolic and Nutritional
Musculoskeletal
Neurologic
Respiratory
Skin and Hypersensitivy Reactions
Special Senses
Urogenital
Miscellaneous
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Theophylline in the drug label.
Drug Interactions
There is limited information regarding Theophylline Drug Interactions in the drug label.
Use in Specific Populations
Pregnancy
- Pregnancy Category
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Theophylline in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Theophylline during labor and delivery.
Nursing Mothers
There is no FDA guidance on the use of Theophylline with respect to nursing mothers.
Pediatric Use
There is no FDA guidance on the use of Theophylline with respect to pediatric patients.
Geriatic Use
There is no FDA guidance on the use of Theophylline with respect to geriatric patients.
Gender
There is no FDA guidance on the use of Theophylline with respect to specific gender populations.
Race
There is no FDA guidance on the use of Theophylline with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Theophylline in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Theophylline in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Theophylline in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Theophylline in patients who are immunocompromised.
Administration and Monitoring
Administration
Monitoring
There is limited information regarding Monitoring of Theophylline in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Theophylline in the drug label.
Overdosage
General
- The chronicity and pattern of theophylline overdosage significantly influences clinical manifestations of toxicity, management and outcome.
- There are two common presentations: (1) acute overdose, i.e., ingestion of a single large excessive dose (>10 mg/kg) as occurs in the context of an attempted suicide or isolated medication error, and (2) chronic overdosage, i.e., ingestion of repeated doses that are excessive for the patient’s rate of theophylline clearance. The most common causes of chronic theophylline overdosage include patient or care giver error in dosing, clinician prescribing of an excessive dose or a normal dose in the presence of factors known to decrease the rate of theophylline clearance, and increasing the dose in response to an exacerbation of symptoms without first measuring the serum theophylline concentration to determine whether a dose increase is safe.
- Severe toxicity from theophylline overdose is a relatively rare event. In one health maintenance organization, the frequency of hospital admissions for chronic overdosage of theophylline was about 1 per 1000 person-years exposure.
- In another study, among 6000 blood samples obtained for measurement of serum theophylline concentration, for any reason, from patients treated in an emergency department, 7% were in the 20-30 mcg/mL range and 3% were >30 mcg/mL.
- Approximately two-thirds of the patients with serum theophylline concentrations in the 20-30 mcg/mL range had one or more manifestations of toxicity while >90% of patients with serum theophylline concentrations >30mcg/mL were clinically intoxicated.
- Similarly, in other reports, serious toxicity from theophylline is seen principally at serum concentrations >30 mcg/mL.
- Several studies have described the clinical manifestations of theophylline overdose and attempted to determine the factors that predict life-threatening toxicity.
- In general, patients who experience an acute overdose are less likely to experience seizures than patients who have experienced a chronic overdosage, unless the peak serum theophylline concentration is >100 mcg/mL.
- After a chronic overdosage, generalized seizures, life-threatening cardiac arrhythmias, and death may occur at serum theophylline concentrations >30 mcg/mL.
- The severity of toxicity after chronic overdosage is more strongly correlated with the patient’s age than the peak serum theophylline concentration; patients >60 years are at the greatest risk for severe toxicity and mortality after a chronic overdosage.
- Pre-existing or concurrent disease may also significantly increase the susceptibility of a patient to a particular toxic manifestation, e.g., patients with neurologic disorders have an increased risk of seizures and patients with cardiac disease have an increased risk of cardiac arrhythmias for a given serum theophylline concentration compared to patients without the underlying disease.
- The frequency of various reported manifestations of theophylline overdose according to the mode of overdose are listed in Table IV.
- Other manifestations of theophylline toxicity include increases in serum calcium, creatine kinase, myoglobin and leukocyte count, decreases in serum phosphate and magnesium, acute myocardial infarction, and urinary retention in men with obstructive uropathy.
- Seizures associated with serum theophylline concentrations >30 mcg/mL are often resistant to anticonvulsant therapy and may result in irreversible brain injury if not rapidly controlled.
- Death from theophylline toxicity is most often secondary to cardiorespiratory arrest and/or hypoxic encephalopathy following prolonged generalized seizures or intractable cardiac arrhythmias causing hemodynamic compromise.
Overdose Management
- General Recommendations for Patients with Symptoms of Theophylline Overdose or Serum Theophylline Concentrations >30 mcg/mL (Note: Serum theophylline concentrations may continue to increase after presentation of the patient for medical care.)
- While simultaneously instituting treatment, contact a regional poison center to obtain updated information and advice on individualizing the recommendations that follow.
- Institute supportive care, including establishment of intravenous access, maintenance of the airway, and electrocardiographic monitoring.
- Treatment of seizures Because of the high morbidity and mortality associated with theophylline-induced seizures, treatment should be rapid and aggressive.
- Anticonvulsant therapy should be initiated with an intravenous benzodiazepine, e.g., diazepam, in increments of 0.1-0.2 mg/kg every 1-3 minutes until seizures are terminated. Repetitive seizures should be treated with a loading dose of phenobarbital (20 mg/kg infused over 30- 60 minutes). * Case reports of theophylline overdose in humans and animal studies suggest that phenytoin is ineffective in terminating theophylline-induced seizures.
- The doses of benzodiazepines and phenobarbital required to terminate theophylline-induced seizures are close to the doses that may cause severe respiratory depression or respiratory arrest; the clinician should therefore be prepared to provide assisted ventilation.
- Elderly patients and patients with COPD may be more susceptible to the respiratory depressant effects of anticonvulsants.
- Barbiturate-induced coma or administration of general anesthesia may be required to terminate repetitive seizures or status epilepticus. General anesthesia should be used with caution in patients with theophylline overdose because fluorinated volatile anesthetics may sensitize the myocardium to endogenous catecholamines released by theophylline.
- Enflurane appears to less likely to be associated with this effect than halothane and may, therefore, be safer.
- Neuromuscular blocking agents alone should not be used to terminate seizures since they abolish the musculoskeletal manifestations without terminating seizure activity in the brain.
- Anticipate Need for Anticonvulsants In patients with theophylline overdose who are at high risk for theophylline induced seizures, e.g., patients with acute overdoses and serum theophylline concentrations >100 mcg/mL chronic overdosage in patients >60 years of age with serum theophylline concentrations >30 mcg/mL, the need for anticonvulsant therapy should be anticipated.
- A benzodiazepine such as diazepam should be drawn into a syringe and kept at the patient’s bedside and medical personnel qualified to treat seizures should be immediately available.
- In selected patients at high risk for theophylline-induced seizures, consideration should be given to the administration of prophylactic anticonvulsant therapy.
- Situations where prophylactic anticonvulsant therapy should be considered in high risk patients include anticipated delays in instituting methods for extracorporeal removal of theophylline (e.g., transfer of a high risk patient from one health care facility to another for extracorporeal removal) and clinical circumstances that significantly interfere with efforts to enhance theophylline clearance (e.g., a neonate where dialysis may not be technically feasible or a patient with vomiting unresponsive to antiemetics who is unable to tolerate multiple-dose oral activated charcoal).
- In animal studies, prophylactic administration of phenobarbital, but not phenytoin, has been shown to delay the onset of theophylline induced generalized seizures and to increase the dose of theophylline required to induce seizures (i.e., markedly increases the LD50).
- Although there are no controlled studies in humans, a loading dose of intravenous phenobarbital (20 mg/kg infused over 60 minutes) may delay or prevent life-threatening seizures in high risk patients while efforts to enhance theophylline clearance are continued.
- Phenobarbital may cause respiratory depression, particularly in elderly patients and patients with COPD.
- Treatment of cardiac arrhythmias Sinus tachycardia and simple ventricular premature beats are not harbingers of life-threatening arrhythmias, they do not require treatment in the absence of hemodynamic compromise, and they resolve with declining serum theophylline concentrations.
- Other arrhythmias, especially those associated with hemodynamic compromise, should be treated with antiarrhythmic therapy appropriate for the type of arrhythmia.
- Gastrointestinal decontamination Oral activated charcoal (0.5 g/kg up to 20 g and repeat at least once 1-2 hours after the first dose) is extremely effective in blocking the absorption of theophylline throughout the gastrointestinal tract, even when administered several hours after ingestion. * If the patient is vomiting, the charcoal should be administered through a nasogastric tube or after administration of an antiemetic. Phenothiazine antiemetics such as prochlorperazine or perphenazine should be avoided since they can lower the seizure threshold and frequently cause dystonic reactions. * A single dose of sorbitol may be used to promote stooling to facilitate removal of theophylline bound to charcoal from the gastrointestinal tract.
- Sorbitol, however, should be dosed with caution since it is a potent purgative which can cause profound fluid and electrolyte abnormalities, particularly after multiple doses.
- Commercially available fixed combinations of liquid charcoal and sorbitol should be avoided in young children and after the first dose in adolescents and adults since they do not allow for individualization of charcoal and sorbitol dosing.
- Ipecac syrup should be avoided in theophylline overdoses. Although ipecac induces emesis, it does not reduce the absorption of theophylline unless administered within 5 minutes of ingestion and even then is less effective than oral activated charcoal.
- Moreover, ipecac induced emesis may persist for several hours after a single dose and significantly decrease the retention and the effectiveness of oral activated charcoal.
- Serum Theophylline Concentration Monitoring The serum theophylline concentration should be measured immediately upon presentation, 2-4 hours later, and then at sufficient intervals, e.g., every 4 hours, to guide treatment decisions and to assess the effectiveness of therapy.
- Serum theophylline concentrations may continue to increase after presentation of the patient for medical care as a result of continued absorption of theophylline from the gastrointestinal tract.
- Serial monitoring of serum theophylline serum concentrations should be continued until it is clear that the concentration is no longer rising and has returned to non-toxic levels.
- General Monitoring Procedures Electrocardiographic monitoring should be initiated on presentation and continued until the serum theophylline level has returned to a non-toxic level.
- Serum electrolytes and glucose should be measured on presentation and at appropriate intervals indicated by clinical circumstances. Fluid and electrolyte abnormalities should be promptly corrected. Monitoring and treatment should be continued until the serum concentration decreases below 20 mcg/mL.
- Enhance clearance of theophylline Multiple-dose oral activated charcoal (e.g., 0.5 mg/kg up to 20 g, every two hours) increases the clearance of theophylline at least twofold by adsorption of theophylline secreted into gastrointestinal fluids.
- Charcoal must be retained in, and pass through, the gastrointestinal tract to be effective; emesis should therefore be controlled by administration of appropriate antiemetics.
- Alternatively, the charcoal can be administered continuously through a nasogastric tube in conjunction with appropriate antiemetics.
- A single dose of sorbitol may be administered with the activated charcoal to promote stooling to facilitate clearance of the adsorbed theophylline from the gastrointestinal tract.
- Sorbitol alone does not enhance clearance of theophylline and should be dosed with caution to prevent excessive stooling which can result in severe fluid and electrolyte imbalances.
- Commercially available fixed combinations of liquid charcoal and sorbitol should be avoided in young children and after the first dose in adolescents and adults since they do not allow for individualization of charcoal and sorbitol dosing.
- In patients with intractable vomiting, extracorporeal methods of theophylline removal should be instituted.
Specific Recommendations
Acute Overdose
- Serum Concentration >20<30 mcg/mL
- Administer a single dose of oral activated charcoal.
- Monitor the patient and obtain a serum theophylline concentration in 2-4 hours to insure that the concentration is not increasing.
- Serum Concentration >30<100 mcg/mL
- Administer multiple dose oral activated charcoal and measures to control emesis.
- Monitor the patient and obtain serial theophylline concentrations every 2-4 hours to gauge the effectiveness of therapy and to guide further treatment decisions.
- Institute extracorporeal removal if emesis, seizures, or cardiac arrhythmias cannot be adequately controlled.
- Serum Concentration >100 mcg/mL
- Consider prophylactic anticonvulsant therapy.
- Administer multiple-dose oral activated charcoal and measures to control emesis.
- Consider extracorporeal removal, even if the patient has not experienced a seizure (see OVERDOSAGE, EXTRACORPOREAL REMOVAL).
- Monitor the patient and obtain serial theophylline concentrations every 2-4 hours to gauge the effectiveness of therapy and to guide further treatment decisions.
Chronic Overdosage
- Serum Concentration >20<30 mcg/mL (with manifestations of theophylline toxicity)
- Administer a single dose of oral activated charcoal.
- Monitor the patient and obtain a serum theophylline concentration in 2-4 hours to insure that the concentration is not increasing.
- Serum Concentration >30 mcg/mL in patients <60 years of age
- Administer multiple-dose oral activated charcoal and measures to control emesis.
- Monitor the patient and obtain serial theophylline concentrations every 2-4 hours to gauge the effectiveness of therapy and to guide further treatment decisions.
- Institute extracorporeal removal if emesis, seizures, or cardiac arrhythmias cannot be adequately controlled.
- Serum Concentration >30 mcg/mL in patients ≥60 years of age.
- Consider prophylactic anticonvulsant therapy.
- Administer multiple-dose oral activated charcoal and measures to control emesis.
- Consider extracorporeal removal even if the patient has not experienced a seizure (see OVERDOSAGE, EXTRACORPOREAL REMOVAL).
- Monitor the patient and obtain serial theophylline concentrations every 2-4 hours to gauge the effectiveness of therapy and to guide further treatment decisions.
=Extracorporeal Removal=
- Increasing the rate of theophylline clearance by extracorporeal methods may rapidly decrease serum concentrations, but the risks of the procedure must be weighed against the potential benefit. Charcoal hemoperfusion is the most effective method of extracorporeal removal, increasing theophylline clearance up to six fold, but serious complications, including hypotension, hypocalcemia, platelet consumption and bleeding diatheses may occur.
- Hemodialysis is about as efficient as multiple-dose oral activated charcoal and has a lower risk of serious complications than charcoal hemoperfusion.
- Hemodialysis should be considered as an alternative when charcoal hemoperfusion is not feasible and multiple-dose oral charcoal is ineffective because of intractable emesis.
- Serum theophylline concentrations may rebound 5-10 mcg/mL after discontinuation of charcoal hemoperfusion or hemodialysis due to redistribution of theophylline from the tissue compartment. Peritoneal dialysis is ineffective for theophylline removal; exchange transfusions in neonates have been minimally effective.
Pharmacology
| |
| |
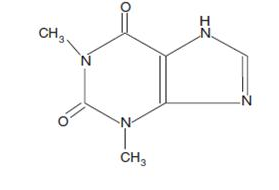
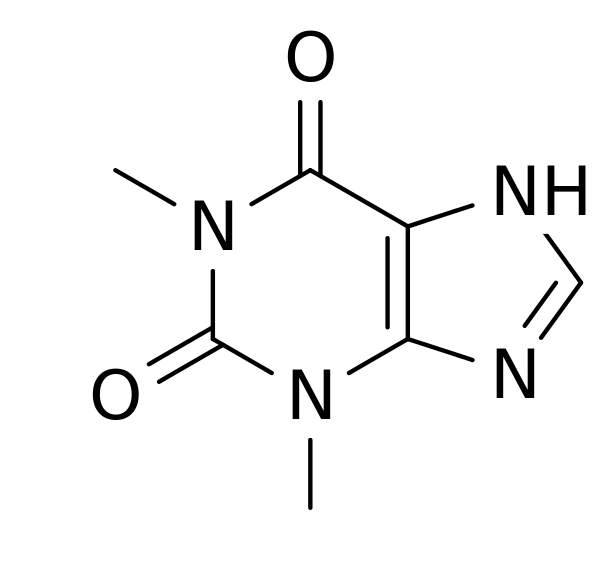
Theophylline
| |
| Systematic (IUPAC) name | |
| 1,3-dimethyl-7H-purine-2,6-dione | |
| Identifiers | |
| CAS number | |
| ATC code | R03 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 180.164 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | 100% |
| Protein binding | 40%, primarily to albumin |
| Metabolism | hepatic to 1-methyluric acid |
| Half life | 5-8 hours |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. | |
| Legal status |
Prescription Only (S4)(AU) ?(CA) POM(UK) [[Prescription drug|Template:Unicode-only]](US) |
| Routes | oral, IV, rectal |
Mechanism of Action
- Theophylline has two distinct actions in the airways of patients with reversible obstruction; smooth muscle relaxation (i.e., bronchodilation) and suppression of the response of the airways to stimuli (i.e., non-bronchodilator prophylactic effects).
- While the mechanisms of action of theophylline are not known with certainty, studies in animals suggest that bronchodilatation is mediated by the inhibition of two isozymes of phosphodiesterase (PDE III and, to a lesser extent, PDE IV) while non-bronchodilator prophylactic actions are probably mediated through one or more different molecular mechanisms, that do not involve inhibition of PDE III or antagonism of adenosine receptors.
- Some of the adverse effects associated with theophylline appear to be mediated by inhibition of PDE III (e.g., hypotension, tachycardia, headache, and emesis) and adenosine receptor antagonism (e.g., alterations in cerebral blood flow).
- Theophylline increases the force of contraction of diaphragmatic muscles. This action appears to be due to enhancement of calcium uptake through an adenosine-mediated channel.
Structure
Pharmacodynamics
There is limited information regarding Theophylline Pharmacodynamics in the drug label.
Pharmacokinetics
Overview
- Theophylline is rapidly and completely absorbed after oral administration in solution or immediate-release solid oral dosage form. Theophylline does not undergo any appreciable pre-systemic elimination, distributes freely into fat-free tissues and is extensively metabolized in the liver.
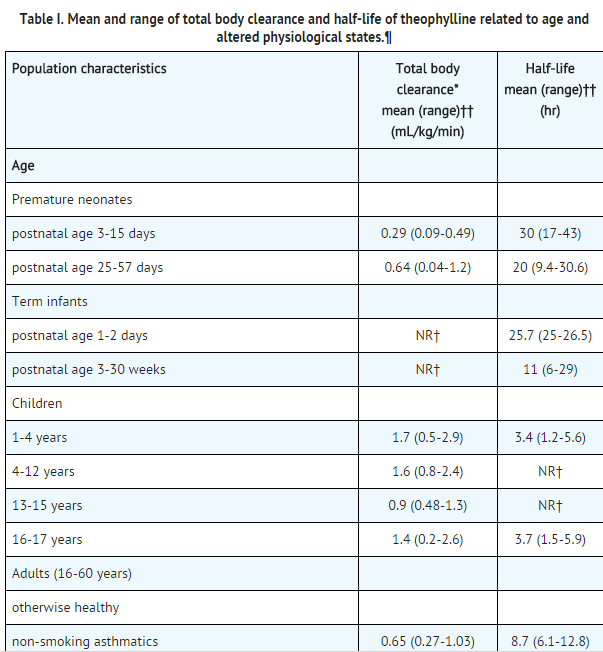
- The pharmacokinetics of theophylline vary widely among similar patients and cannot be predicted by age, sex, body weight or other demographic characteristics.
- In addition, certain concurrent illnesses and alterations in normal physiology and co-administration of other drugs (see Table II) can significantly alter the pharmacokinetic characteristics of theophylline. Within-subject variability in metabolism has also been reported in some studies, especially in acutely ill patients.
- It is, therefore, recommended that serum theophylline concentrations be measured frequently in acutely ill patients (e.g., at 24-hour intervals) and periodically in patients receiving long-term therapy, e.g., at 6-12 month intervals. More frequent measurements should be made in the presence of any condition that may significantly alter theophylline clearance
This image is provided by the National Library of Medicine. 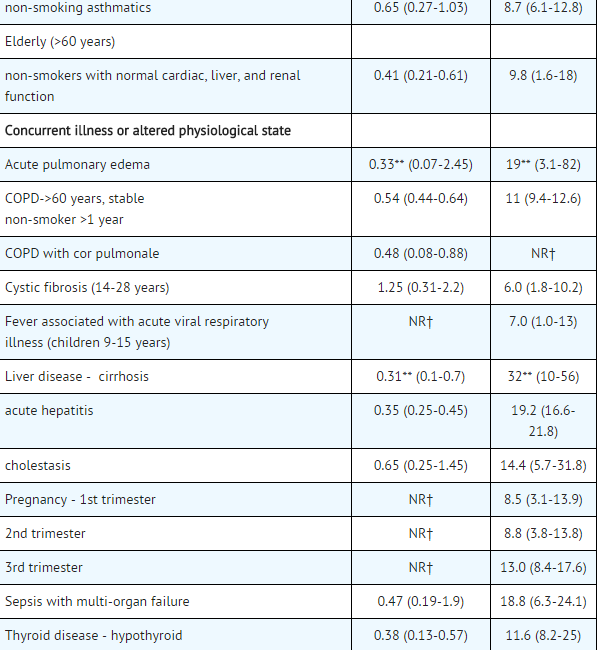
This image is provided by the National Library of Medicine. 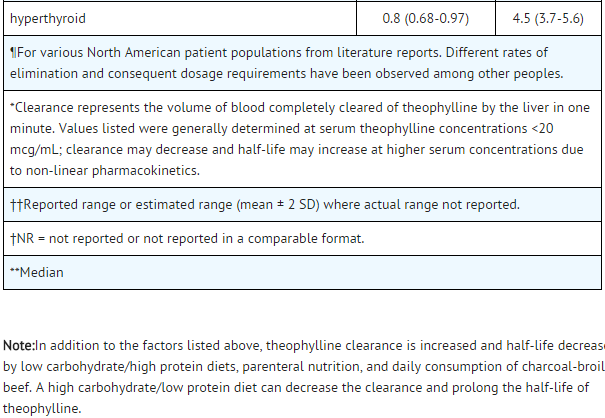
This image is provided by the National Library of Medicine.
Absorption
- Theophylline is rapidly and completely absorbed after oral administration in solution or immediate-release solid oral dosage form. After a single dose of 5 mg/kg in adults, a mean peak serum concentration of about 10 mcg/mL (range 5-15 mcg/mL) can be expected 1-2 hr after the dose.
- Co-administration of theophylline with food or antacids does not cause clinically significant changes in the absorption of theophylline from immediate-release dosage forms.
Distribution
- Once theophylline enters the systemic circulation, about 40% is bound to plasma protein, primarily albumin. Unbound theophylline distributes throughout body water, but distributes poorly into body fat.
- The apparent volume of distribution of theophylline is approximately 0.45 L/kg (range 0.3-0.7 L/kg) based on ideal body weight.
- Theophylline passes freely across the placenta, into breast milk and into the cerebrospinal fluid (CSF).
- Saliva theophylline concentrations approximate unbound serum concentrations, but are not reliable for routine or therapeutic monitoring unless special techniques are used. An increase in the volume of distribution of theophylline, primarily due to reduction in plasma protein binding, occurs in premature neonates, patients with hepatic cirrhosis, uncorrected acidemia, the elderly and in women during the third trimester of pregnancy.
- In such cases, the patient may show signs of toxicity at total (bound +unbound) serum concentrations of theophylline in the therapeutic range (10-20 mcg/mL) due to elevated concentrations of the pharmacologically active unbound drug.
- Similarly, a patient with decreased theophylline binding may have a subtherapeutic total drug concentration while the pharmacologically active unbound concentration is in the therapeutic range.
- If only total serum theophylline concentration is measured, this may lead to an unnecessary and potentially dangerous dose increase. In patients with reduced protein binding, measurement of unbound serum theophylline concentration provides a more reliable means of dosage adjustment than measurement of total serum theophylline concentration.
- Generally, concentrations of unbound theophylline should be maintained in the range of 6-12 mcg/mL.
Metabolism
- Following oral dosing, theophylline does not undergo any measurable first-pass elimination. In adults and children beyond one year of age, approximately 90% of the dose is metabolized in the liver.
- Biotransformation takes place through demethylation to 1-methylxanthine and 3-methylxanthine and hydroxylation to 1,3-dimethyluric acid. 1-methylxanthine is further hydroxylated, by xanthine oxidase, to 1-methyluric acid. About 6% of a theophylline dose is N-methylated to caffeine.
- Theophylline demethylation to 3-methylxanthine is catalyzed by cytochrome P-450 1A2, while cytochromes P-450 2E1 and P-450 3A3 catalyze the hydroxylation to 1,3-dimethyluric acid. Demethylation to 1-methylxanthine appears to be catalyzed either by cytochrome P-450 1A2 or a closely related cytochrome.
- In neonates, the N-demethylation pathway is absent while the function of the hydroxylation pathway is markedly deficient. The activity of these pathways slowly increases to maximal levels by one year of age.
- Caffeine and 3-methylxanthine are the only theophylline metabolites with pharmacologic activity. 3-methylxanthine has approximately one tenth the pharmacologic activity of theophylline and serum concentrations in adults with normal renal function are <1 mcg/mL.
- In patients with end-stage renal disease, 3-methylxanthine may accumulate to concentrations that approximate the unmetabolized theophylline concentration.
- Caffeine concentrations are usually undetectable in adults regardless of renal function. In neonates, caffeine may accumulate to concentrations that approximate the unmetabolized theophylline concentration and thus, exert a pharmacologic effect.
- Both the N-demethylation and hydroxylation pathways of theophylline biotransformation are capacity-limited. Due to the wide intersubject variability of the rate of theophylline metabolism, non-linearity of elimination may begin in some patients at serum theophylline concentrations <10 mcg/mL.
- Since this non-linearity results in more than proportional changes in serum theophylline concentrations with changes in dose, it is advisable to make increases or decreases in dose in small increments in order to achieve desired changes in serum theophylline concentrations.
- Accurate prediction of dose-dependency of theophylline metabolism in patients a priori is not possible, but patients with very high initial clearance rates (i.e., low steady state serum theophylline concentrations at above average doses) have the greatest likelihood of experiencing large changes in serum theophylline concentration in response to dosage changes.
Excretion
- In neonates, approximately 50% of the theophylline dose is excreted unchanged in the urine.
- Beyond the first three months of life, approximately 10% of the theophylline dose is excreted unchanged in the urine.
- The remainder is excreted in the urine mainly as 1,3-dimethyluric acid (35-40%), 1-methyluric acid (20-25%) and 3-methylxanthine (15-20%). Since little theophylline is excreted unchanged in the urine and since active metabolites of theophylline (i.e., caffeine, 3-methylxanthine) do not accumulate to clinically significant levels even in the face of end-stage renal disease, no dosage adjustment for renal insufficiency is necessary in adults and children >3 months of age.
- In contrast, the large fraction of the theophylline dose excreted in the urine as unchanged theophylline and caffeine in neonates requires careful attention to dose reduction and frequent monitoring of serum theophylline concentrations in neonates with reduced renal function.
Serum Concentrations at Steady State
- After multiple doses of theophylline, steady state is reached in 30-65 hours (average 40 hours) in adults.
- At steady state, on a dosage regimen with 6-hour intervals, the expected mean trough concentration is approximately 60% of the mean peak concentration, assuming a mean theophylline half-life of 8 hours.
- The difference between peak and trough concentrations is larger in patients with more rapid theophylline clearance.
- In patients with high theophylline clearance and half-lives of about 4-5 hours, such as children age 1 to 9 years, the trough serum theophylline concentration may be only 30% of peak with a 6-hour dosing interval.
- In these patients a slow release formulation would allow a longer dosing interval (8-12 hours) with a smaller peak/trough difference.
Geriatric
- The clearance of theophylline is decreased by an average of 30% in healthy elderly adults (> 60 yrs) compared to healthy young adults. Careful attention to dose reduction and frequent monitoring of serum theophylline concentrations are required in elderly patients.
Pediatrics
- The clearance of theophylline is very low in neonates. Theophylline clearance reaches maximal values by one year of age, remains relatively constant until about 9 years of age and then slowly decreases by approximately 50% to adult values at about age 16.
- Renal excretion of unchanged theophylline in neonates amounts to about 50% of the dose, compared to about 10% in children older than three months and in adults.
- Careful attention to dosage selection and monitoring of serum theophylline concentrations are required in pediatric patients.
Gender
- Gender differences in theophylline clearance are relatively small and unlikely to be of clinical significance. Significant reduction in theophylline clearance, however, has been reported in women on the 20th day of the menstrual cycle and during the third trimester of pregnancy.
Race
- Pharmacokinetic differences in theophylline clearance due to race have not been studied.
Renal Insufficiency
- Only a small fraction, e.g., about 10%, of the administered theophylline dose is excreted unchanged in the urine of children greater than three months of age and adults. Since little theophylline is excreted unchanged in the urine and since active metabolites of theophylline (i.e., caffeine, 3-methylxanthine) do not accumulate to clinically significant levels even in the face of end-stage renal disease, no dosage adjustment for renal insufficiency is necessary in adults and children >3 months of age.
- In contrast, approximately 50% of the administered theophylline dose is excreted unchanged in the urine in neonates.
- Careful attention to dose reduction and frequent monitoring of serum theophylline concentrations are required in neonates with decreased renal function.
Hepatic Insufficiency
- Theophylline clearance is decreased by 50% or more in patients with hepatic insufficiency (e.g., cirrhosis, acute hepatitis, cholestasis).
- Careful attention to dose reduction and frequent monitoring of serum theophylline concentrations are required in patients with reduced hepatic function.
Congestive Heart Failure (CHF)
- Theophylline clearance is decreased by 50% or more in patients with CHF. The extent of reduction in theophylline clearance in patients with CHF appears to be directly correlated to the severity of the cardiac disease.
- Since theophylline clearance is independent of liver blood flow, the reduction in clearance appears to be due to impaired hepatocyte function rather than reduced perfusion.
- Careful attention to dose reduction and frequent monitoring of serum theophylline concentrations are required in patients with CHF.
Smokers
- Tobacco and marijuana smoking appears to increase the clearance of theophylline by induction of metabolic pathways.
- Theophylline clearance has been shown to increase by approximately 50% in young adult tobacco smokers and by approximately 80% in elderly tobacco smokers compared to non-smoking subjects.
- Passive smoke exposure has also been shown to increase theophylline clearance by up to 50%. Abstinence from tobacco smoking for one week causes a reduction of approximately 40% in theophylline clearance.
- Careful attention to dose reduction and frequent monitoring of serum theophylline concentrations are required in patients who stop smoking. Use of nicotine gum has been shown to have no effect on theophylline clearance.
Fever
- Fever, regardless of its underlying cause, can decrease the clearance of theophylline. The magnitude and duration of the fever appear to be directly correlated to the degree of decrease of theophylline clearance. Precise data are lacking, but a temperature of 39oC (102oF) for at least 24 hours is probably required to produce a clinically significant increase in serum theophylline concentrations.
- Children with rapid rates of theophylline clearance (i.e., those who require a dose that is substantially larger than average [e.g., >22 mg/kg/day] to achieve a therapeutic peak serum theophylline concentration when afebrile) may be at greater risk of toxic effects from decreased clearance during sustained fever.
- Careful attention to dose reduction and frequent monitoring of serum theophylline concentrations are required in patients with sustained fever.
Miscellaneous
- Other factors associated with decreased theophylline clearance include the third trimester of pregnancy, sepsis with multiple organ failure, and hypothyroidism.
- Careful attention to dose reduction and frequent monitoring of serum theophylline concentrations are required in patients with any of these conditions.
- Other factors associated with increased theophylline clearance include hyperthyroidism and cystic fibrosis.
Clinical Studies
- In patients with chronic asthma, including patients with severe asthma requiring inhaled corticosteroids or alternate-day oral corticosteroids, many clinical studies have shown that theophylline decreases the frequency and severity of symptoms, including nocturnal exacerbations, and decreases the “as needed” use of inhaled beta-2 agonists.
- Theophylline has also been shown to reduce the need for short courses of daily oral prednisone to relieve exacerbations of airway obstruction that are unresponsive to bronchodilators in asthmatics.
- In patients with chronic obstructive pulmonary disease (COPD), clinical studies have shown that theophylline decreases dyspnea, air trapping, the work of breathing, and improves contractility of diaphragmatic muscles with little or no improvement in pulmonary function measurements.
Nonclinical Toxicology
There is limited information regarding Nonclinical Toxicology of Theophylline in the drug label.
Clinical Studies
There is limited information regarding Clinical Studies of Theophylline in the drug label.
How Supplied
- ELIXOPHYLLIN Elixir is a clear red solution with a mixed fruit flavor. Each tablespoonful (15 mL) contains 80 mg theophylline anhydrous.
- ELIXOPHYLLIN Elixir is available in bottles of
- 473 mL NDC 49708-644-90
Storage
- Store at 25oC (77oF); excursions permitted to 15o - 30oC (59o - 86oF) [see USP Controlled Room Temperature].
- Dispense in tight container.
Images
Drug Images
{{#ask: Page Name::Theophylline |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Theophylline |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Theophylline in the drug label.
Precautions with Alcohol
- Alcohol-Theophylline interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- THEOPHYLLINE ®[1]
Look-Alike Drug Names
There is limited information regarding Theophylline Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Theophylline |Label Name=RECOMMENDED STORAGE.jpg
}}