Tavaborole
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aparna Vuppala, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Tavaborole is an antifungal that is FDA approved for the treatment of onychomycosis of the toenails due to trichophyton rubrum or trichophyton mentagrophytes.. Common adverse reactions include Application site erythema, dermatitis, ingrowing toenail, peeling of skin..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Onychomycosis
- Tavaborole topical solution, 5% is an oxaborole antifungal indicated for the treatment of onychomycosis of the toenails due to Trichophyton rubrum or Trichophyton mentagrophytes.
Dosing information
- Apply Tavaboroleto affected toenails once daily for 48 weeks.
- Tavaboroleshould be applied to the entire toenail surface and under the tip of each toenail being treated.
- Tavaboroleis for topical use only and not for oral, ophthalmic, or intravaginal use.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Tavaborole in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Tavaborole in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Tavaborole in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Tavaborole in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Tavaborole in pediatric patients.
Contraindications
- None.
Warnings
There is limited information regarding Tavaborole Warnings' in the drug label.
Adverse Reactions
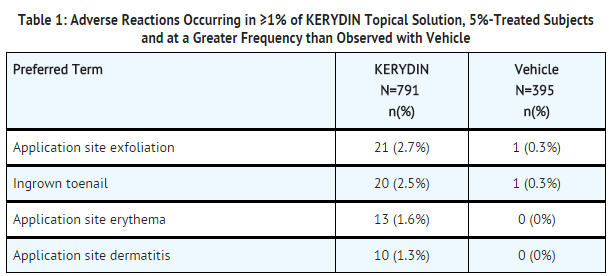
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- In two clinical trials, 791 subjects were treated with Tavaborole. The most commonly reported adverse reactions are listed below
- A cumulative irritancy study revealed the potential for Tavaboroleto cause skin irritation. There was no evidence that Tavaborole causes contact sensitization.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Tavaborole in the drug label.
Drug Interactions
- In vitro studies have shown that tavaborole, at therapeutic concentrations, neither inhibits nor induces cytochrome P450 (CYP450) enzymes.
Use in Specific Populations
Pregnancy
- There are no adequate and well-controlled studies with Tavaborolein pregnant women. Tavaborole should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Systemic embryofetal development studies were conducted in rats and rabbits and a dermal embryofetal development study was conducted in rabbits.
Oral administration:
- In an oral embryofetal development study in rats, oral doses of 30, 100, and 300 mg/kg/day tavaborole were administered during the period of organogenesis (gestational days 6-19) to pregnant female rats. In the presence of maternal toxicity, embryofetal toxicity (increased embryofetal resorption and/or deaths) and drug-related skeletal malformations and variations suggestive of delayed development (i.e., a delay in ossification) were noted in fetuses at 300 mg/kg/day tavaborole [570 times the Maximum Recommended Human Dose (MRHD) based on Area Under the Curve (AUC) comparisons]. No developmental toxicity was noted in rats at 100 mg/kg/day tavaborole (26 times the MRHD based on AUC comparisons).
- In an oral embryofetal development study in rabbits, oral doses of 15, 50, and 150 mg/kg/day tavaborole were administered during the period of organogenesis (gestational days 7-19) to pregnant female rabbits. In the presence of maternal toxicity, excessive embryofetal mortality due to post-implantation loss was noted at 150 mg/kg/day tavaborole. No drug related malformations were noted in rabbits at 150 mg/kg/day tavaborole (155 times the MRHD based on AUC comparisons). No embryofetal mortality was noted in rabbits at 50 mg/kg/day tavaborole (16 times the MRHD based on AUC comparisons).
Topical administration:
- In a dermal embryofetal development study in rabbits, topical doses of 1%, 5%, and 10% tavaborole solution were administered during the period of organogenesis (gestational days 6-28) to pregnant female rabbits. A dose dependent increase in dermal irritation at the treatment site was noted at 5% and 10% tavaborole solution. A decrease in fetal bodyweight was noted at 10% tavaborole solution. No drug related malformations were noted in rabbits at 10% tavaborole solution (36 times the MRHD based on AUC comparisons). No embryofetal toxicity was noted in rabbits at 5% tavaborole solution (26 times the MRHD based on AUC comparisons).Nonteratogenic effects:
- In an oral pre- and post-natal development study in rats, oral doses of 15, 60, and 100 mg/kg/day tavaborole were administered from the beginning of organogenesis (gestation day 6) through the end of lactation (lactation day 20). In the presence of minimal maternal toxicity, no embryofetal toxicity or effects on postnatal development were noted at 100 mg/kg/day (29 times the MRHD based on AUC comparisons).
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Tavaborole in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Tavaborole during labor and delivery.
Nursing Mothers
- It is not known whether tavaborole is excreted in human milk following topical application of KERYDIN. Because many drugs are excreted in human milk, caution should be exercised when Tavaboroleis administered to a nursing woman.
Pediatric Use
- Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
- In clinical trials of 791 subjects who were exposed to KERYDIN, 19% were 65 years of age and over, while 4% were 75 years of age and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, but greater sensitivity of some older individuals cannot be ruled out.
Gender
There is no FDA guidance on the use of Tavaborole with respect to specific gender populations.
Race
There is no FDA guidance on the use of Tavaborole with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Tavaborole in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Tavaborole in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Tavaborole in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Tavaborole in patients who are immunocompromised.
Administration and Monitoring
Administration
- Topical
Monitoring
There is limited information regarding Monitoring of Tavaborole in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Tavaborole in the drug label.
Overdosage
There is limited information regarding Chronic Overdose of Tavaborole in the drug label.
Pharmacology
| |
Tavaborole
| |
| Systematic (IUPAC) name | |
| 5-Fluoro-2,1-benzoxaborol-1(3H)-ol | |
| Identifiers | |
| CAS number | ? |
| ATC code | None |
| PubChem | ? |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | ? |
| SMILES | & |
| Synonyms | AN2690 |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status |
Template:Unicode Prescription only |
| Routes | Topical use only |
Mechanism of Action
- The mechanism of action of tavaborole is inhibition of fungal protein synthesis. Tavaborole inhibits protein synthesis by inhibition of an aminoacyl-transfer ribonucleic acid (tRNA) synthetase (AARS).
Activity in vitro and in clinical infections
- Tavaborole has been shown to be active against most strains of the following microorganisms, both in vitro and in clinical infections :
Mechanism of Resistance
- Trichophyton mentagrophytes and Trichophyton rubrum strains from isolates collected in the clinical trials have not demonstrated resistance following repeated exposure to tavaborole.
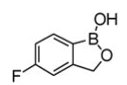
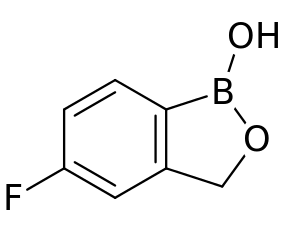
Structure
- Tavaborole(tavaborole) topical solution, 5% contains tavaborole, 5% (w/w) in a clear, colorless alcohol-based solution for topical use. The active ingredient, tavaborole, is an oxaborole antifungal with the chemical name of 5-fluoro-1,3-dihydro-1-hydroxy-2,1-benzoxaborole. The chemical formula is C7H6BFO2, the molecular weight is 151.93 and the structural formula is:
- Tavaborole is a white to off-white powder. It is slightly soluble in water and freely soluble in ethanol and propylene glycol.
- Each mL of Tavaborolecontains 43.5 mg of tavaborole. Inactive ingredients include alcohol, edetate calcium disodium, and propylene glycol.
Pharmacodynamics
- At therapeutic doses, Tavaboroleis not expected to prolong QTc to any clinically relevant extent.
Pharmacokinetics
- Tavaborole undergoes extensive metabolism. Renal excretion is the major route of elimination.
- In a clinical pharmacology trial of six healthy adult male volunteers who received a single topical application of 5% 14C-tavaborole solution, tavaborole conjugates and metabolites were shown to be excreted primarily in the urine.
- The pharmacokinetics of tavaborole was investigated in 24 subjects with distal subungual onychomycosis involving at least 4 toenails (including at least 1 great toenail) following a single dose and a 2-week daily topical application of 200 μL of a 5% solution of tavaborole to all ten toenails and 2 mm of skin surrounding each toenail. Steady state was achieved after 14 days of dosing. After a single dose, the mean (± standard deviation) peak concentration (Cmax) of tavaborole was 3.54 ± 2.26 ng/mL (n=21 with measurable concentrations, range 0.618-10.2 ng/mL, LLOQ=0.5 ng/mL), and the mean AUClast was 44.4 ± 25.5 ng*hr/mL (n=21). After 2 weeks of daily dosing, the mean Cmax was 5.17 ± 3.47 ng/mL (n=24, range 1.51-12.8 ng/mL), and the mean AUCτ was 75.8 ± 44.5 ng*hr/mL.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- In an oral carcinogenicity study in Sprague-Dawley rats, oral doses of 12.5, 25, and 50 mg/kg/day tavaborole were administered to rats once daily for 104 weeks. No drug related neoplastic findings were noted at oral doses up to 50 mg/kg/day tavaborole (14 times the MRHD based on AUC comparisons).
- In a dermal carcinogenicity study in CD-1 mice, topical doses of 5%, 10%, and 15% tavaborole solution were administered to mice once daily for 104 weeks. No drug related neoplastic findings were noted at topical doses up to 15% tavaborole solution (89 times the MRHD based on AUC comparisons).
- Tavaborole revealed no evidence of mutagenic or clastogenic potential based on the results of two in vitro genotoxicity tests (Ames assay and Human lymphocyte chromosomal aberration assay) and one in vivo genotoxicity test (rat micronucleus assay).
- No effects on fertility were observed in male and female rats that were administered oral doses up to 300 mg/kg/day tavaborole (107 times the MRHD based on AUC comparisons) prior to and during early pregnancy.
Clinical Studies
- The efficacy and safety of Tavaborole was evaluated in two multicenter, double-blind, randomized, vehicle-controlled trials. Tavaboroleor vehicle was applied once daily for 48 weeks in subjects with 20% to 60% clinical involvement of the target toenail, without dermatophytomas or lunula (matrix) involvement.
- A total of 1194 subjects (795 KERYDIN, 399 Vehicle) 18 to 88 years of age, 82% male, 84% white, participated in these two trials. Efficacy assessments were made at 52 weeks following a 48-week treatment period.
- The Complete Cure efficacy endpoint included negative mycology (negative KOH wet mount and negative fungal culture) and Completely Clear Nail (no clinical evidence of onychomycosis as evidenced by a normal toenail plate, no onycholysis, and no subungual hyperkeratosis). Efficacy results from the two trials are summarized in
How Supplied
- Tavaborole(tavaborole) topical solution, 5% is a clear, colorless solution supplied in an amber glass bottle with a screw cap. At initial use, the screw cap is replaced with the dropper assembly.
- Tavaborole(tavaborole) topical solution, 5% is supplied in the following presentations:
- NDC 55724-111-11: One 12 mL bottle containing 10 mL of solution with one glass pointed-tip dropper
- NDC 55724-111-21: One 10 mL bottle containing 4 mL of solution with one glass pointed-tip dropper
Storage
Storage and Handling
- Store at 20–25°C (68–77°F); excursions permitted to 15–30°C (59–86°F) [see USP Controlled Room Temperature].
- CAUTION: Flammable. Keep away from heat and flame.
- Discard product within 3 months after insertion of the dropper.
- Keep bottle tightly closed. Keep out of reach of children.
Images
Drug Images
{{#ask: Page Name::Tavaborole |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Tavaborole |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- The patient should be told the following:
- Use Tavaborole as directed by a health care professional.
- Tavaborole is for external use only. Avoid contact with eyes, mouth, or vagina. Avoid contact with skin other than skin immediately surrounding the treated nail(s). Wipe away excess solution from surrounding skin.
- Clean and dry nails prior to Tavaboroleuse. Tavaborole should be applied to completely cover the nail surface and also applied under the tip of each nail being treated. Allow solution to dry following application.
- Inform a health care professional if the area of application shows signs of persistent irritation (for example, redness, itching, swelling).
- Forty-eight (48) weeks of daily application with tavaborole is considered the full treatment for toenail onychomycosis.
- Do not use Tavaborolefor any disorder other than that for which it is prescribed
- Product is flammable. Avoid use near heat or open flame.
Precautions with Alcohol
- Alcohol-Tavaborole interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- ®[1]
Look-Alike Drug Names
There is limited information regarding Tavaborole Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Tavaborole |Label Name=Tavaborole04.png
}}
{{#subobject:
|Label Page=Tavaborole |Label Name=Tavaborole05.png
}}