Siltuximab
{{DrugProjectFormSinglePage |authorTag=Alberto Plate [1] |genericName=Siltuximab |aOrAn=a |drugClass=monoclonal antibody |indicationType=treatment |indication=patients with multi centric Castleman's disease (MCD) who are human immunodeficiency virus (HIV) negative and human herpesvirus-8 (HHV-8) negative. Siltuximab was not studied in patients with MCD who are HIV positive or HHV-8 positive because Siltuximab did not bind to virally produced IL-6 in a nonclinical study |adverseReactions=pruritus, increased weight, rash, hyperuricemia, and upper respiratory tract infection |blackBoxWarningTitle=TITLE |blackBoxWarningBody=Condition Name: (Content) |fdaLIADAdult=====Dosage====
- Siltuximab 11 mg/kg is given over 1 hour as an intravenous infusion administered every 3 weeks until treatment failure.
- Perform hematology laboratory tests prior to each dose of Siltuximab therapy for the first 12 months and every 3 dosing cycles thereafter. If treatment criteria outlined in TABLE 1 are not met, consider delaying treatment with Siltuximab. Do not reduce dose.

- Do not administer Siltuximab to patients with severe infections until the infection resolves.
- Discontinue Siltuximab in patients with severe infusion related reactions, anaphylaxis, severe allergic reactions, or cytokine release syndromes. Do not reinstitute treatment.
Instructions for Preparation and Administration
Use aseptic technique for reconstitution and preparation of dosing solution.
- 1.- Calculate the dose (mg), total volume (mL) of reconstituted Siltuximab solution required and the number of vials needed. A 21-gauge 1-½ inch needle is recommended for preparation. Infusion bags (250 mL) must contain Dextrose 5% in Water and must be made of Polyvinyl chloride (PVC) with Di-{2-ethylhexyl}phthalate (DEHP), or Polyolefin (PO).
- 2.- Allow the vial(s) of Siltuximab to come to room temperature over approximately 30 minutes. Siltuximab should remain at room temperature for the duration of the preparation.
- 3.- Aseptically reconstitute each Siltuximab vial as instructed in TABLE 2.

Gently swirl the reconstituted vials to aid the dissolution of the lyophilized powder. DO NOT SHAKE or SWIRL VIGOROUSLY. Do not remove the contents until all of the solids have been completely dissolved. The lyophilized powder should dissolve in less than 60 minutes.
Once reconstituted, and prior to further dilution, inspect the vials for particulates and discoloration. Do not use if particles or solution discoloration are present or if visibly opaque. The reconstituted product should be kept for no more than two hours prior to addition into the infusion bag.
- 4.- Dilute the reconstituted Siltuximab solution dose to 250 mL with sterile Dextrose 5% in Water by withdrawing a volume equal to the total calculated volume of reconstituted Siltuximab from the Dextrose 5% in Water, 250 mL bag. Slowly add the total calculated volume (mL) of reconstituted Siltuximab solution to the Dextrose 5% in Water infusion bag. Gently invert the bag to mix the solution.
- 5.- Administer the diluted Siltuximab solution in 5% Dextrose in Water 250 mL by intravenous infusion over a period of 1 hour using administration sets lined with polyvinyl chloride (PVC) or polyurethane (PU), containing a 0.2-micron inline polyethersulfone (PES) filter. The infusion should be completed within 4 hours of the dilution of the reconstituted solution to the infusion bag.
- 6.- Do not infuse Siltuximab concomitantly in the same intravenous line with other agents.
- 7.- Do not store any unused portion of the reconstituted product or of the infusion solution. Waste material should be disposed of in accordance with local requirements.
|offLabelAdultGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Siltuximab in adult patients. |offLabelAdultNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Siltuximab in adult patients. |offLabelPedGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Siltuximab in pediatric patients. |offLabelPedNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Siltuximab in pediatric patients. |contraindications=*Severe hypersensitivity reaction to siltuximab or any of the excipients in Siltuximab. |warnings=====Concurrent Active Severe Infections====
- Do not administer Siltuximab to patients with severe infections until the infection resolves. Siltuximab may mask signs and symptoms of acute inflammation including suppression of fever and of acute phase reactants such as C-reactive protein (CRP). Monitor patients receiving Siltuximab closely for infections. Institute prompt anti-infective therapy and do not administer further Siltuximab until the infection resolves.
Vaccinations
- Do not administer live vaccines to patients receiving Siltuximab because IL-6 inhibition may interfere with the normal immune response to new antigens.
Infusion Related Reactions and Hypersensitivity
- Stop the infusion of Siltuximab if the patient develops signs of anaphylaxis. Discontinue further therapy with Siltuximab.
- Stop the infusion if the patient develops a mild to moderate infusion reaction. If the reaction resolves, the Siltuximab infusion may be restarted at a lower infusion rate. Consider medication with antihistamines, acetaminophen, and corticosteroids. Discontinue Siltuximab if the patient does not tolerate the infusion following these interventions.
- Administer Siltuximab in a setting that provides resuscitation equipment, medication, and personnel trained to provide resuscitation.
Gastrointestinal Perforation
- Gastrointestinal perforation has been reported in clinical trials although not in MCD trials. Use with caution in patients who may be at increased risk for GI perforation. Promptly evaluate patients presenting with symptoms that may be associated or suggestive of GI perforation.
|clinicalTrials=The following adverse reactions are also discussed in other sections of the labeling:
- Concurrent active severe infections.
- Infusion-related reactions and hypersensitivity.
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
- The most common adverse reactions (>10% compared to placebo) during treatment with Siltuximab in the MCD clinical trial were pruritus, increased weight, rash, hyperuricemia, and upper respiratory tract infection.
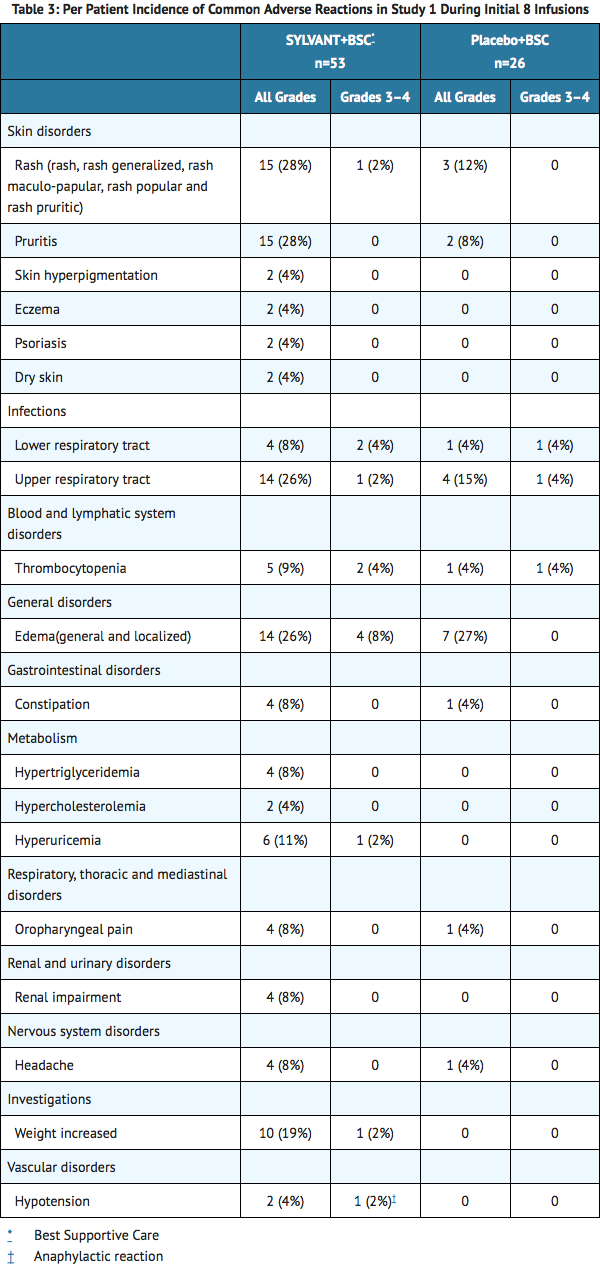
- The data presented below in TABLE 3 were collected from Study 1. Study 1, in MCD, was an international, multicenter, randomized phase 2 study of every 3 week infusions comparing Siltuximab and best supportive care (BSC) to placebo and BSC. There were 53 patients randomized to the Siltuximab arm at a dose of 11 mg/kg and 26 patients randomized to the placebo arm. Of the 26 placebo-treated patients, 13 patients subsequently crossed-over to receive Siltuximab The median age was 48 years (range 20 to 78), 66% male, 48% Asian, 39% White, 4% Black or African American, 7% other. The patients randomized to Siltuximab received a median of 19 infusions (range 1 to 50) compared to patients randomized to placebo who received a median of 8 infusions (range 2 to 32). To control for disparate exposure between arms, Table 3 reports the per patient incidence of adverse reactions that occurred during the first 8 infusions. Adverse reactions that occurred >3% in the Siltuximab arm are presented.
- Siltuximab was also evaluated as a single agent in another hematologic disease in Study 2. Study 2 was an international, multicenter, randomized phase 2 study of every 4 week infusions comparing Siltuximab and BSC to placebo and BSC. There were 50 patients randomized to the Siltuximab arm at a dose of 15 mg/kg (unapproved dose) and 26 patients randomized to the placebo arm. The median age was 72 years (range 50 to 85), 58% male, 96% White, 1% Asian, 1% Black, and 1% other. The median number of infusions in both arms was 3 (range 1 to 4). The study was stopped early due to a lack of efficacy. Adverse reactions that occurred >3% in the Siltuximab arm are presented in Table 4.

Long Term Exposure
- The safety of long term administration of Siltuximab to patients with MCD was evaluated in Study 3. Study 3 enrolled patients from the initial dose finding study of Siltuximab with MCD who were benefiting from chronic Siltuximab therapy. Siltuximab was administered at a dose of 11 mg/kg every 3 to 6 weeks. At the time of data cut off 19 patients were enrolled. The median age was 44 years (range 18 – 76), 63% male, 84% Caucasian, 11% Asian, and 5% Black. The median exposure to Siltuximab for these 19 patients was 5.1 years (range 3.4 to 7.2). The most common adverse reaction (>20%) reported by subjects receiving Siltuximab in this study was upper respiratory tract infection (63%); diarrhea (32%); pain in extremities, arthralgia and fatigue (21% each). No patient was removed from therapy for any reason. There were no deaths. There were no cumulative toxicities identified with prolonged treatment with Siltuximab.
Anaphylaxis and Infusion Related Reactions
- Approximately 750 patients have been treated with Siltuximab. Of these, one patient experienced an anaphylactic reaction. Data from 249 patients treated with Siltuximab monotherapy forms the basis of the safety evaluation of infusion related reactions. Infusion related reactions were reported in 4.8% of these patients. Symptoms of infusion reactions consisted of back pain, chest pain or discomfort, nausea and vomiting, flushing, erythema, and palpitations.
Immunogenicity
- Immunogenicity data are highly dependent on the sensitivity and specificity of the test methods used. Additionally, the observed incidence of a positive result in a test method may be influenced by several factors, including sample handling, timing of sample collection, drug interference, concomitant medication and the underlying disease. Therefore, comparison of the incidence of antibodies to Siltuximab with the incidence of antibodies to other products may be misleading. The clinical significance of anti-siltuximab antibodies following treatment with Siltuximab is not known.
- The immunogenicity of siltuximab has been evaluated using antigen-bridging enzyme immunoassay (EIA) and electrochemiluminescence-based immunoassay (ECLIA) methods. A total of 411 patients across the clinical studies were evaluated at multiple time points for anti-therapeutic antibody (ATA) responses to siltuximab after treatment with Siltuximab Following Siltuximab dosing, 0.2% (1/411) of patients tested positive for anti-siltuximab antibodies. Further immunogenicity analyses of the single positive sample revealed a low titer of anti-siltuximab antibodies with non-neutralizing capabilities.
- No evidence of altered toxicity profile was identified in the patient who developed antibodies to siltuximab.
|drugInteractions=No in vitro or in vivo drug-drug interaction studies have been conducted with Siltuximab.
Cytochrome P450 Substrates
- Cytochrome P450s in the liver are down regulated by infection and inflammation stimuli including cytokines such as IL-6. Inhibition of IL-6 signaling in patients treated with Siltuximab may restore CYP450 activities to higher levels leading to increased metabolism of drugs that are CYP450 substrates compared to metabolism prior to treatment with Siltuximab.
- Upon initiation or discontinuation of Siltuximab, in patients being treated with CYP450 substrates with a narrow therapeutic index, perform therapeutic monitoring of effect (e.g., warfarin) or drug concentration (e.g., cyclosporine or theophylline) as needed and adjust dose. The effect of Siltuximab on CYP450 enzyme activity can persist for several weeks after stopping therapy. Exercise caution when Siltuximab is co-administered with CYP3A4 substrate drugs where a decrease in effectiveness would be undesirable (e.g., oral contraceptives, lovastatin, atorvastatin).
|FDAPregCat=C |useInPregnancyFDA=====Risk-Summary====
- There are no adequate or well-controlled studies in pregnant women. In animal reproduction studies, administration of a human antibody to IL-6 to pregnant cynomolgus monkeys caused decreases in globulin levels in pregnant animals and in the offspring. Siltuximab crossed the placenta in monkeys. Infants born to pregnant women treated with Siltuximab may be at increased risk of infection, and caution is advised in the administration of live vaccines to these infants. Siltuximab should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Advise patients of childbearing potential to avoid pregnancy. Women of childbearing potential should use contraception during and for 3 months after treatment.
Animal Data
- In an embryo-fetal development study, siltuximab doses of 9.2 or 46 mg/kg/week were administered intravenously to pregnant monkeys during gestation days (GD) 20 to 118, which includes the period of organogenesis. Fetuses were evaluated on GD 140, approximately 25 days prior to the natural birth. Exposures at the low and high dose after the 25th administration were approximately 3 and 7 times respectively the exposure in humans at the recommended dose of 11 mg/kg. There was no siltuximab-related maternal or fetal toxicity. However, siltuximab crossed the placenta at both doses and when measured on GD 140, fetal serum concentrations of siltuximab were similar to maternal concentrations. In a combined embryofetal and pre- and post-natal development study, cynomolgus monkeys were intravenously administered doses of 10 or 50 mg/kg/week of a human antibody to IL-6 from GD 20 to natural delivery (GD 167). The offspring was evaluated up to 7 months after birth for developmental effects. No maternal or infant toxicity was observed; however, globulin levels were decreased in pregnant animals (GD 34 through lactation day 30) and in the offspring (lactation days 30–120) at both doses.
|useInNursing=*It is not known whether siltuximab is excreted in human milk or absorbed systemically after ingestion. Because many drugs and immunoglobulins are excreted in human milk, and because of the potential for adverse reactions in nursing infants from Siltuximab, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. |useInPed=The safety and efficacy of Siltuximab have not been established in pediatric patients. |useInGeri=*Of the patients treated with Siltuximab monotherapy in clinical studies 127 (35%) were 65 years and older. No overall differences in safety profile were observed between these patients and younger patients, and other reported clinical experience has not identified differences in the safety profile between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Clinical studies did not include sufficient numbers of patients aged 65 years and older to determine the effect of age on efficacy in MCD population. |useInRenalImpair=*Based on a population pharmacokinetic analysis using data from clinical trials in patients, no significant difference in siltuximab clearance was observed in patients with pre-existing renal impairment (creatinine clearance (CLCr) ≥15 mL/min) compared to patients with baseline normal renal function (CLCr ≥90 mL/min). No initial dosage adjustment is necessary for patients with CLCr ≥15 mL/min. The potential effect of end stage renal disease on siltuximab pharmacokinetics cannot be determined |useInHepaticImpair=*Based on a population pharmacokinetic analysis using data from clinical trials in patients, no significant difference in siltuximab clearance was observed in patients with pre-existing mild to moderate hepatic impairment (Child-Pugh Class A and B, respectively) compared to patients with baseline normal hepatic function. No initial dosage adjustment is necessary for patients with mild to moderate hepatic impairment. Patients with baseline severe hepatic impairment (Child-Pugh Class C) were not included in clinical trials. |overdose=No case of overdose has been reported. |drugBox=
Siltuximab?
| |
| Therapeutic monoclonal antibody | |
| Source | xi/o |
| Target | IL-6 |
| Identifiers | |
| CAS number | |
| ATC code | L04 |
| PubChem | ? |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 145.0 kDa |
| Synonyms | CNTO 328 |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
C(US) |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | ? |
|mechAction=*Siltuximab binds human IL-6 and prevents the binding of IL-6 to both soluble and membrane-bound IL-6 receptors. IL-6 has been shown to be involved in diverse normal physiologic processes such as induction of immunoglobulin secretion. Overproduction of IL-6 has been linked to systemic manifestations in patients with MCD. |PD=*Cardiac Electrophysiology: The effect of multiple doses of Siltuximab (15 mg/kg every 3 weeks for 4 cycles) on the QTc interval was evaluated in an open label, single arm study in 30 patients with Monoclonal Gammopathy of Undetermined Significance, Smoldering Multiple Myeloma, or Indolent Multiple Myeloma. No large changes in the mean QTc interval (i.e., >20 ms) were detected in the study.
- Measurement of IL-6 concentrations in serum or plasma during treatment should not be used as pharmacodynamic marker, as siltuximab-neutralized antibody-IL-6 complexes interfere with current immunological-based IL-6 quantification methods.
|PK=The pharmacokinetics of siltuximab were evaluated in patients with multi centric Castleman's disease and hematological and non-hematological malignancies. The serum siltuximab pharmacokinetics are adequately described by a linear two-compartment intravenous model with first-order elimination.
Distribution
- Following Siltuximab administration (11 mg/kg, once every 3 weeks as 1-hour intravenous infusion) in patients with multi centric Castleman's disease, the maximum serum siltuximab concentration (Cmax) occurred close to the end of infusion. At steady state, the serum mean Cmax value for siltuximab is 332 mcg/mL (42% CV), and the serum mean predose trough value is 84 mcg/mL (78% CV).
- With the once every 3 week dosing regimen, siltuximab steady state is achieved by the sixth infusion, and siltuximab accumulates approximately 1.7-fold relative to a single dose. Following multiple dosing, siltuximab showed approximately dose proportional pharmacokinetics over the dose range of 2.8 to 11 mg/kg.
- Based on population pharmacokinetic analysis, the central volume of distribution in a male subject with body weight of 70 kg is 4.5 L (20% CV).
Elimination
- Based on the population pharmacokinetic analysis, the clearance of siltuximab in patients is 0.23 L/day (51% CV). Based on population pharmacokinetic analysis (n=378), body weight was identified as the only statistically significant covariate for siltuximab clearance. Therefore, the body weight based dosing is appropriate.
- The mean terminal half-life (t1/2) for siltuximab in patients after the first intravenous infusion of 11 mg/kg is 20.6 days (range: 14.2 to 29.7 days).
Specific Populations
- Age and Gender: Based on population pharmacokinetic analysis, age [range: 18 to 85 years (n=378)] and gender [female (n=175), male (n=203)] do not affect exposure of siltuximab.
- Renal Impairment: A population pharmacokinetic analysis (based on pre-existing renal function) was carried out with data from 377 patients enrolled in clinical trials, including 176 with normal renal function (CLCr ≥90 mL/min), 122 with mild renal impairment (CLCr 60 to <90 mL/min), 75 with moderate renal impairment (CLCr 30 to <60 mL/min), and 3 with severe renal impairment (CLCr 15 to 29 mL/min). The apparent clearance of siltuximab was similar in patients with pre-existing mild, moderate and severe renal impairment (CLCr 15 to <90 mL/min) compared to patients with normal renal function. The potential effect of end stage renal disease on siltuximab pharmacokinetics cannot be determined as clinical and pharmacokinetic data are available from only one patient.
- Hepatic Impairment: A population pharmacokinetic analysis (based on pre-existing hepatic function) was carried out with data from 377 patients enrolled in clinical trials, including 302 with normal hepatic function, 72 with mild hepatic impairment (Child-Pugh A), and 3 with moderate hepatic impairment (Child-Pugh B). The apparent clearance of siltuximab was similar in patients with pre-existing mild and moderate hepatic impairment (Child-Pugh Class A and B) compared to patients with normal hepatic function. The potential effect of severe hepatic impairment on siltuximab pharmacokinetics cannot be determined as clinical and pharmacokinetic data are not available.
|nonClinToxic=====Carcinogenesis, Mutagenesis, Impairment of Fertility====
- No carcinogenicity or genotoxicity studies have been conducted with siltuximab.
- Two fertility studies were conducted. In one study, drug-treated male mice were mated with untreated females and in the second study drug-treated female mice were mated with untreated males. A murine analog of siltuximab was administered subcutaneously at doses up to 100 mg/kg/week for a total of 7 doses in both studies. There was no effect on male or female fertility parameters. In addition, siltuximab did not produce any toxicity in the reproductive organs in cynomolgus monkeys in the 6-month repeat-dose toxicology study at doses up to 46 mg/kg (approximately 7 times) the systemic exposure in patients at the recommended dose.
|clinicalStudies=*The clinical efficacy and safety of Siltuximab for the treatment of patients with MCD was established in Study 1, a phase 2, multinational, randomized (2:1) double blind, placebo controlled study. In this study 53 patients were randomized to Best Supportive Care (BSC) and Siltuximab at a dose of 11 mg/kg every 3 weeks and 26 patients were randomized to BSC and placebo. The median age was 48 years (range 20 to 78), 66% male, 48% Asian, 39% White, 4% Black or African American, 7% other. The histological subtype of MCD was similar in both treatment arms, with 33% hyaline vascular subtype, 23% plasmacytic subtype and 44% mixed subtype. Treatment was continued until treatment failure (defined as disease progression based on increase in symptoms, radiologic progression or deterioration in performance status) or unacceptable toxicity.
- The major efficacy outcome of the study was durable tumor and symptomatic response, defined as tumor response (PR and CR based on modified International Working Group response criteria for malignant lymphoma) assessed by independent review and complete resolution or stabilization of MCD symptoms. Thirty-four MCD related signs and symptoms prospectively identified were collected and graded according to the NCI-CTCAE v 4, by investigators. A durable response was defined as tumor and symptomatic response that persisted for a minimum of 18 weeks without treatment failure. The durable tumor and symptomatic response in the Siltuximab arm was 34% compared to 0% in the placebo arm (95% CI: 11.1, 54.8; p=0.0012).
- Other analyses included tumor response, time to treatment failure and an increase in hemoglobin of 1.5 g/dL or more, in patients who were anemic at time of study entry, at week 13. The results are summarized in TABLE 5.
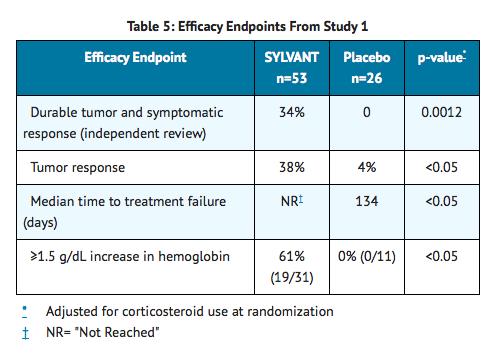
- A consistent treatment effect was confirmed on subgroup analysis for all parameters evaluated with the exception of the hyaline vascular histological subtype. There were no patients with hyaline vascular histology who demonstrated a durable tumor and symptomatic response. However, activity was suggested in this subtype based on change in hemoglobin and median time to treatment failure.
- At the time of the analysis, overall survival data were not mature. One year survival rate was 100% in the Siltuximab arm and 92% in the placebo arm.
|howSupplied=Each Siltuximab vial is individually packaged in a carton:
- NDC 57894-420-01 contains one 100 mg vial, single use vial
- NDC 57894-421-01 contains one 400 mg vial, single use vial
|storage=*Siltuximab must be refrigerated at 2ºC to 8ºC (36ºF to 46ºF). Do not use Siltuximab beyond the expiration date (EXP) located on the carton and the vial.
- While stored, protect from light. This product contains no preservative.
|packLabel=



|fdaPatientInfo=

Patients or their caregivers should be advised of the potential benefits and risks of Siltuximab. Physicians should instruct their patients to read the patient labeling before starting Siltuximab therapy and to reread it each time they receive an infusion. It is important that the patient's overall health be assessed at each treatment visit and that any questions resulting from the patient's or their caregiver's reading of the patient labeling be discussed.
Infections
- Inform patients that Siltuximab may lower their resistance to infections. Instruct the patient of the importance of contacting their doctor immediately when symptoms suggesting infection appear in order to assure rapid evaluation and appropriate treatment.
Vaccination
- Inform the patient that they should discuss the recommended vaccinations prior to treatment with Siltuximab.
Allergic Reactions
- Advise patients to seek immediate medical attention if they experience any symptoms of serious allergic reactions during the infusion. Signs include: difficulty breathing, chest tightness, wheezing, severe dizziness or light-headedness, swelling of the lips or skin rash.
Contraception
- Advise patients of childbearing potential to avoid pregnancy which may include use of contraception during treatment and for 3 months after Siltuximab therapy.
Other Medical Conditions
- Advise patients to report any signs of new or worsening medical conditions.
|alcohol=Alcohol-Siltuximab interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. |brandNames=*Sylvant }}