Schizophrenia pathophysiology
Jump to navigation
Jump to search
| https://https://www.youtube.com/watch?v=PURvJV2SMso%7C350}} |
|
Schizophrenia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Schizophrenia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Schizophrenia pathophysiology |
|
Risk calculators and risk factors for Schizophrenia pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Vindhya BellamKonda, M.B.B.S [2], Irfan Dotani
Overview
Studies suggest that genetics, early environmental, neurobioloic, psychological and social processes are important contributory factors in the development of schizophrenia. Current psychiatric research is focused on the role of neurobiology, but a clear organic cause has not been found.
Pathophysiology
- Differences in the size and structure of certain brain areas have been found in some adults diagnosed with schizophrenia.
- Early findings came from the discovery of ventricular enlargement in people diagnosed with schizophrenia with negative symptoms most prominent.[1]
- However, this finding has not proved particularly reliable on the level of the individual person, with considerable variation between patients.
- More recent studies have shown a large number of differences in brain structure between people with and without diagnoses of schizophrenia.[2]
- However, as with earlier studies, many of these differences are only reliably detected when comparing groups of people and are unlikely to predict any differences in brain structure of an individual person with schizophrenia.
Brain structure and Imaging
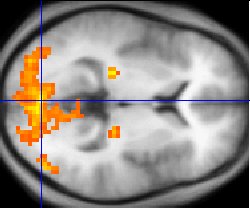
- Studies using neuropsychological tests and brain imaging technologies such as fMRI and PET to examine functional differences in brain activity have shown that differences seem to most commonly occur in the frontal lobes, hippocampus, and temporal lobes.[3]
- These differences are heavily linked to the neurocognitive deficit often asssociated with schizophrenia, particularly in areas of memory, attention, problem solving, executive function, and social cognition.
- A recent study by UCLA researchers [3] involved MRI scanning in recently diagnosed schizophrenic patients over a period of 5 years.
- Researchers found a dramatic destruction of gray matter in a short period of time in those diagnosed, the destruction spreading from the back of the brain to the front over time.
- Interestingly, when the destruction had reached the frontal lobe, the acutest symptoms arose, and severe delusions began.
- Those with the most severe symptoms were shown to have lost the most brain matter per year.
- This study is important in shedding light on schizophrenia as a physical disorder of the brain and less likely "a disease invented by society".
- There have also been findings of differences in the size and structure of certain brain areas in schizophrenia, starting with the discovery of ventricular enlargement in those for whom negative symptoms were most prominent.[1]
- However, this has not proven particularly reliable on the level of the individual person, with considerable variation between patients.
- More recent studies have shown various differences in brain structure between people with and without diagnoses of schizophrenia.[2]
- However, as with earlier studies, many of these differences are only reliably detected when comparing groups of people and are unlikely to predict any differences in brain structure of an individual person with schizophrenia.
Electroencephalography
- Electroencephalograph (EEG) recordings of persons with schizophrenia performing perception oriented tasks showed an absence of gamma band activity in the brain, indicating weak integration of critical neural networks in the brain.[4]
- Those who experienced intense hallucinations, delusions and disorganized thinking showed the lowest frequency synchronization.
- None of the drugs taken by the persons scanned had moved neural synchrony back into the gamma frequency range.
- Gamma band and working memory alterations may be related to alterations in interneurons that produce the neurotransmitter GABA.
Dopamine
- Particular focus has been placed upon the function of dopamine in the mesolimbic pathway of the brain.
- This focus largely resulted from the accidental finding that a drug group which blocks dopamine function, known as the phenothiazines, could reduce psychotic symptoms.
- An influential theory, known as the "dopamine hypothesis of schizophrenia", proposed that a malfunction involving dopamine pathways was therefore the cause of (the positive symptoms of) schizophrenia.
- This theory is now thought to be overly simplistic as a complete explanation, partly because newer antipsychotic medication (called atypical antipsychotic medication) can be equally effective as older medication (called typical antipsychotic medication) while also affecting serotonin function and having somewhat less of a dopamine blocking effect.
- In addition, dopamine pathway dysfunction has not been reliably shown to correlate with symptom onset or severity.
Glutamate
- Interest has also focused on the neurotransmitter glutamate and the reduced function of the NMDA glutamate receptor in schizophrenia.
- This has largely been suggested by abnormally low levels of glutamate receptors found in postmortem brains of people previously diagnosed with schizophrenia and the discovery that the glutamate blocking drugs such as phencyclidine and ketamine can mimic the symptoms and cognitive problems associated with the condition.[5][6]
- The fact that reduced glutamate function is linked to poor performance on tests requiring frontal lobe and hippocampal function and that glutamate can affect dopamine function, all of which have been implicated in schizophrenia, have suggested an important mediating (and possibly causal) role of glutamate pathways in schizophrenia.[7] *Further support of this theory has come from preliminary trials suggesting the efficacy of coagonists at the NMDA receptor complex in reducing some of the positive symptoms of schizophrenia.[8]
References
- ↑ 1.0 1.1 Johnstone EC, Crow TJ, Frith CD, Husband J, Kreel L. (1976). Cerebral ventricular size and cognitive impairment in chronic schizophrenia. Lancet, 30;2 (7992), 924–6. PMID 62160
- ↑ 2.0 2.1 Flashman LA, Green MF (2004). Review of cognition and brain structure in schizophrenia: profiles, longitudinal course, and effects of treatment. Psychiatric Clinics of North America, 27 (1), 1–18, vii. PMID 15062627
- ↑ Green, M.F. (2001) Schizophrenia Revealed: From Neurons to Social Interactions. New York: W.W. Norton. ISBN 0-393-70334-7
- ↑ Spencer KM, Nestor PG, Perlmutter R, et al (2004). Neural synchrony indexes disordered perception and cognition in schizophrenia. Proceedings of the National Academy of Sciences, 101, 17288-93. PMID 15546988 Full text, Retrieved 2007-05-16.
- ↑ Konradi C, Heckers S. (2003). Molecular aspects of glutamate dysregulation: implications for schizophrenia and its treatment. Pharmacology and Therapeutics, 97(2), 153–79. PMID 12559388
- ↑ Lahti AC, Weiler MA, Tamara Michaelidis BA, Parwani A, Tamminga CA. (2001). Effects of ketamine in normal and schizophrenic volunteers. Neuropsychopharmacology, 25(4), 455–67. PMID 11557159
- ↑ Coyle JT, Tsai G, Goff D. (2003). Converging evidence of NMDA receptor hypofunction in the pathophysiology of schizophrenia. Annals of the New York Academy of Sciences, 1003, 318–27. PMID 14684455
- ↑ Tuominen HJ, Tiihonen J, Wahlbeck K. (2005). Glutamatergic drugs for schizophrenia: a systematic review and meta-analysis. Schizophr Res, 72:225–34. PMID 15560967