Sandbox dialysis
|
Dialysis Main Page |
|
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [7]Associate Editor(s)-in-Chief: Seyedmahdi Pahlavani, M.D. [8]

Overview
In medicine, hemodialysis (also haemodialysis) is a method for removing waste products such as potassium and urea, as well as free water from the blood when the kidneys are incapable of this (i.e. in renal failure). It is a form of renal dialysis and is therefore a renal replacement therapy.
Hemodialysis is typically conducted in an dedicated facility, either a special room in a hospital or a clinic (with specialized nurses and technicians) that specializes in hemodialysis. Although less typical, dialysis can also be done in a patient's home as home hemodialysis.
Principle
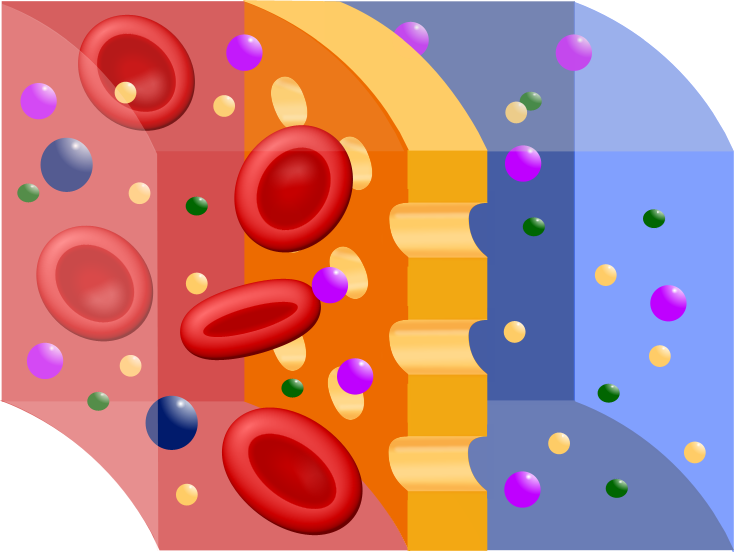
The principle of hemodialysis is the same as other methods of dialysis; it involves diffusion of solutes across a semipermeable membrane. Hemodialysis utilizes counter current flow, where the dialysate is flowing in the opposite direction to blood flow in the extracorporeal circuit. Counter-current flow maintains the concentration gradient across the membrane at a maximum and increases the efficiency of the dialysis.
Fluid removal (ultrafiltration) is achieved by altering the hydrostatic pressure of the dialysate compartment, causing free water and some dissolved solutes to move across the membrane along a created pressure gradient.
The dialysis solution that is used is a sterilized solution of mineral ions. Urea and other waste products, and also, potassium and phosphate, diffuse into the dialysis solution. However, concentrations of sodium and chloride are similar to those of normal plasma to prevent loss. Bicarbonate is added in a higher concentration than plasma to correct blood acidity. A small amount of glucose is also commonly used.
Note that this is a different process to the related technique of hemofiltration.
Prescription
A prescription for dialysis by a nephrologist (a medical kidney specialist) will specify various parameters for a dialysis treatment. These include frequency (how many treatments per week), length of each treatment, and the blood and dialysis solution flow rates, as well as the size of the dialyzer. The composition of the dialysis solution is also sometimes adjusted in terms of its sodium and potassium and bicarbonate levels.In general, the larger the body size of an individual, the more dialysis he will need. In the North America and UK, 3-4 hour treatments (sometimes up to 5 hours for larger patients) given 3 times a week are typical. However, dialysis six times a week more be more effective although with more complications from vascular access.[1] Twice-a-week sessions are limited to patients who have a substantial residual kidney function. Four sessions per week are often prescribed for larger patients, as well as patients who have trouble with fluid overload. Finally, there is growing interest in short daily home hemodialysis, which is comprised of 1.5 - 4 hr sessions given 5-7 times per week, usually at home. There also is interest in nocturnal dialysis, which involves dialyzing a patient, usually at home, for 8-10 hours per night, 3-6 nights per week. Nocturnal in-center dialysis, 3-4 times per week is also offered at a handful of dialysis units in the United States.
Side-effects and complications
Hemodialysis usually also involves the removal (ultrafiltration) of extra fluid, because most patients with end-stage renal failure pass little or no urine. The sudden removal of fluid on dialysis may cause side effects, which are usually proportionate to the amount of fluid which is removed. These potential side effects include low blood pressure, fatigue, chest pains, leg-cramps and headaches. These side effects can be alleviated by dialyzing more often and/or longer than the standard three times a week schedule. Typically higher doses of dialysis are available only through home hemodialysis.
Since hemodialysis requires access to the circulatory system, patients undergoing hemodialysis have a portal of entry for microbes, which could lead to septicemia or an infection affecting the heart valves (endocarditis) or bone (osteomyelitis). The risk of infection depends on the type of access used (see below). Bleeding may also occur, again the risk depending on the type of access used.
Heparin is the most commonly used anticoagulant in hemodialysis patients, as it is generally well tolerated and can be quickly reversed with protamine sulfate. Heparin allergy can be a problem and can cause a low platelet count. In such patients, alternative anticoagulants can be used. In patients at high risk of bleeding, dialysis can be done without anticoagulation.
First Use Syndrome is a very rare but severe anaphylactic reaction to the dialyzer. Its symptoms include sneezing, wheezing, shortness of breath, back pain, chest pain, or sudden death. It can be caused by residual sterilant in the dialyzer or the material of the membrane itself. In recent years, the incidence of First Use Syndrome has fallen off, due to an increased use of gamma irradiation, steam sterilization, or electron-beam radiation instead of chemical sterilants, and the development of new dialyzer membranes of higher biocompatibility.
There are specific complications associated with different types of hemodialysis access, listed below.
Access
There are three primary modes of access to the blood in hemodialysis: an intravenous catheter, an arteriovenous (AV) fistula, or synthetic graft. The type of access is influenced by factors such as the expected time course of a patient's renal failure and the condition of his or her vasculature. Patients may have multiple accesses, usually because an AV fistula or graft is maturing, and a catheter is still being used.
Catheter
Catheter access, sometimes called a CVC (Central Venous Catheter), consists of a plastic catheter with two lumens (or occasionally two separate catheters) which is inserted into a large vein (usually the vena cava, via the internal jugular vein or the femoral vein) to allow large flows of blood to be withdrawn from one lumen, to go into the dialysis circuit, and to be returned via the other lumen. However, blood flow is almost always less than that of a well functioning fistula or graft.
They are usually found in two general varieties, tunnelled and non-tunnelled.
Non-tunnelled catheter access is for short term access (up to about 10 days, but often for one dialysis session only), and the catheter emerges from the skin at the site of entry into the vein.
Tunnelled catheter access involves a longer catheter, which is tunnelled under the skin from the point of insertion in the vein to an exit site some distance away. They are usually placed in the internal jugular vein in the neck and the exit site is usually on the chest wall. The tunnel acts as a barrier to invading microbes and as such tunnelled catheters are designed for short to medium term access (weeks to months only), as infection is still a frequent problem.
Aside from infection, central venous stenosis is another serious problem with catheter access. The catheter is a foreign body in the vein, and often provokes an inflammatory reaction in the vein wall, which results in scarring and narrowing of the vein, often to the point where it occludes. This can cause problems with severe venous congestion in the area drained by the vein and may also render the vein, and the veins drained by it, useless for the formation of a fistula or graft at a later date. Patients on longterm hemodialysis can literally 'run-out' of access, so this can be a fatal problem.
Catheter access is usually used for rapid access for immediate dialysis, for tunnelled access in patients who are deemed likely to recover from acute renal failure, and patients with end-stage renal failure, who are either waiting for alternative access to mature, or those who are unable to have alternative access.
Catheter access is often popular with patients, as attachment to the dialysis machine doesn't require needles. However the serious risks of catheter access noted above mean that such access should only be contemplated as a long term solution in the most desperate access situation.
AV fistula
AV (arteriovenous) fistulas are recognized as the preferred access method. To create a fistula, a vascular surgeon joins an artery and a vein together through anastomosis. Since this bypasses the capillaries, blood flows at a very high rate through the fistula. One can feel this by placing one's finger over a mature fistula. This is called feeling for "thrill", and feels like a distinct 'buzzing' feeling over the fistula. Fistulas are usually created in the non-dominant arm, and may be situated on the hand (the 'snuffbox' fistula'), the forearm (usually a radiocephalic fistula, or so-called Brescia-Cimino fistula, in which the radial artery is anastomosed to the cephalic vein) or the elbow (usually a brachiocephalic fistula, where the brachial artery is anastomosed to the cephalic vein). A fistula will take a number of weeks to mature, on average perhaps 4-6 weeks. During treatment, two needles are inserted into the fistula, one to draw blood and one to return it.
The advantages of the AV fistula use are lower infection rates, as there is no foreign material involved in their formation, higher blood flow rates (which translates to more effective dialysis), and a lower incidence of thrombosis. The complications are few, but if a fistula has a very high flow in it, and the vasculature that supplies the rest of the limb is poor, then a steal syndrome can occur, where blood entering the limb is drawn into the fistula and returned to the general circulation without entering the capillaries of the limb. This results in cold extremities of that limb, cramping pains, and if severe, tissue damage. One long term complication of an AV fistula can be the development of a bulging in the wall of the vein, or aneurysm, where the vessel wall is weakend by the repeated insertion of needles over time. To a large extent the risk of developing an aneurysm can be reduced by careful needling technique. Aneurysms may necessitate corrective surgery and may shorten the useful life of a fistula. To prevent damage to the fistula and aneurysm or pseudoaneurysm formation, it is recommended that different needle sticking points be used in a rotating fashion. Another approach is to cannulate the fistula with a blunted needle, in exactly the same place. This is called a 'buttonhole' approach. Often two or three buttonhole places are available on a given fistula. This also can prolong fistula life and help prevent damage to the fistula.
AV graft
AV (arteriovenous) grafts are much like fistulas in most respects, except that an artificial vessel is used to join the artery and vein. The graft usually is made of a synthetic material, often PTFE, but sometimes chemically-treated, sterilized veins from animals are used. Grafts are used when the patient's native vasculature does not permit a fistula. They mature faster than fistulas, and may be ready to be used several weeks after formation (some newer grafts may be used even sooner). However, AV grafts are at high risk for developing narrowing, especially in the vein just downstream to where the graft has been sewn to the vein. As a result of the narrowing, clotting or thrombosis often occurs. As foreign material, they are at greater risk for becoming infected. The options for sites to place a graft are larger, due to the fact that the graft can be fashioned quite long. Thus they can be placed in the thigh or even the neck (the 'necklace graft').
Fistula First project
The access patency and access survival with AV fistulas is much better than that with venous catheters or grafts. Also, patient survival is better with AV fistulas, and AV fistulas have much lower complication rates compared to grafts or venous catheters. For this reason, the Centers for Medicare & Medicaid (CMS) has set up a Fistula First Initiative [2], the object of which is to increase the utilization of AV fistulas in dialysis patients.
Equipment
The hemodialysis machine performs the function of pumping the patient's blood and the dialysate through the dialyzer. The newest dialysis machines on the market are highly computerized and continuously monitor an array of safety-critical parameters, including blood and dialysate flow rates, dialysis solution conductivity, temperature, and pH; as well as dialysate for evidence of blood leakage or presence of air. If any reading is out of normal range, an audible alarm will sound to alert the patient-care technician who is monitoring the patient. Manufacturers of dialysis machines include companies such as Fresenius, Gambro, Baxter, B. Braun, and Bellco.
Water system
An extensive water purification system is absolutely critical for hemodialysis. Since dialysis patients are exposed to vast quantities of water, which is mixed with dialysate concentrate to form the dialysate, even trace mineral contaminants or bacterial endotoxins can filter into the patient's blood. Because the damaged kidneys are not able to perform their intended function of removing impurities, ions that are introduced into the blood stream via water can build up to hazardous levels, causing numerous symptoms including death. Aluminum, chloramine, fluoride, copper, and zinc, as well as bacterial fragments and endotoxins, have all caused problems in this regard.
For this reason, water used in hemodialysis is carefully purified prior to use. Initially it is filtered and temperature-adjusted, and its pH is corrected by addition of acid or base. Then it is softened. Next the water is run through a tank containing activated charcoal to adsorb organic contaminants. Primary purification is then done by forcing water through a membrane with very tiny pores, a so-called reverse osmosis membrane. This lets the water pass, but holds back even very small solutes such as electrolytes. Final removal of left over electrolytes is done by running the water through a tanks with ion-exchange resins, that basically take up any left over anions or cations and replace them with hydroxyl and hydrogen molecules, respectively, leaving ultrapure water.
Ultrapure dialysate
Even this degree of water purification may not be enough. The trend lately is to pass this final purified water (after mixing with dialysate concentrate) through a dialyzer membrane, to have another layer of protection in terms of removing impurities, especially those of bacterial origin that may have accumulated in the water after its passage through the original water purification system.
On-line monitoring of dialysis solution during dialysis Once purified water is mixed with dialysate concentrate, its conductivity increases, since water that contains charged ions conducts electricity. During dialysis, the conductivity of dialysis solution is continuously monitored, to make sure that the water and dialysate concentrate are being mixed in the proper proportions. Both excessively concentrated dialysis solution, and excessively dilute solution can cause severe clinical problems.
Dialyzer
Basic construction:
The dialyzer is the piece of equipment that actually filters the blood. Almost all dialyzers in use today are of the hollow-fiber variety. A cylindrical bundle of hollow fibers, the walls of which are composed of semi-permeable membrane, is anchored at each end into potting compound (a sort of glue), and then this assembly is put into a clear plastic cylindrical shell with 4 openings. One opening or blood port at each end of the cylinder communicates with each end of the bundle of hollow fibers. This forms the "blood compartment" of the dialyzer. Two other ports are cut into the side of the cylinder. These communicate with the space around the hollow fibers, the "dialysate compartment". Blood is pumped via the blood ports through this bundle of very thin capillary-like tubes, and the dialysate is pumped through the space surrounding the fibers. Pressure gradients are applied when necessary in order to move fluid from the blood to the dialysate compartment.
Membrane and flux:
Dialyzer membranes come with different pore sizes. Those with smaller pore size are called "low-flux", and those with larger pore sizes are called "high-flux". Some larger molecules, for example, beta-2-microglobulin are not removed at all with low-flux dialyzers, and the trend has been to use high-flux dialyzers lately. However, then newer dialysis machines and high-quality dialysis solution needs to be used, to control the rate of fluid removal properly, and to prevent backflow of dialysis solution impurities into the patient through the membrane.
Dialyzer membranes used to be made primarily of cellulose (derived from cotton linter). The surface of such membranes was not very biocompatible, because exposed hydroxyl groups would activate complement in the blood passing by the membrane. Modifications of the basic, "unsubstituted" cellulose membrane were then developed. One was to cover these hydroxyl groups with acetate groups (cellulose acetate); another was to mixing in some compounds that would inhibit complement activation at the membrane surface (modified cellulose). The original "unsubstituted cellulose" membranes are no longer in wide use, whereas cellulose acetate and modified cellulose dialyzers are still used. Cellulosic membranes can be made in either low-flux or high-flux configuration, depending on their pore size.
Another group of membranes is made from synthetic materials, made of polymers such as polyarylethersulfone, polyamide, polyvinylpyrrolidone, polycarbonate, or polyacrylonitrile. These synthetic membranes activate complement to a lesser degree than unsubstituted cellulose membranes. Synthetic membranes can be made in either low- or high-flux configuration, but most of them tend to be high-flux.
Nanotechnology is being used in some of the most recent high-flux membranes in order to have a uniform pore size. The goal of high-flux membranes is to pass relatively large molecules such as beta-2-microglobulin (MW 11,600 daltons), but to not pass albumin (MW ~66,400 daltons). Whenever a membrane is made, there is a size distribution range of the pores, and as larger pore sizes are approached, some high-flux dialyzers begin to let albumin pass out of the blood into the dialysate. This is thought to be undesirable, although one school of thought believes that some albumin removal may be beneficial in terms of removing protein-bound uremic toxins.
Membrane flux and outcome
Whether use of a high-flux dialyzer results in better patient outcomes is somewhat controversial, but several important studies have suggested that there are clinical benefits to doing so. The NIH funded HEMO trial compared survival and hospitalizations in a randomized trial in patients being dialyzed with low-flux vs. high-flux membranes. Although the primary outcome (all-cause mortality) was not quite statistically significantly better in the group randomized to use high-flux membranes, several secondary outcomes were better in the high-flux group [3][4]. A recent Cochrane analysis concluded that benefit of membrane choice on outcomes has not yet been demonstrated [5].
Membrane flux and beta-2-microglobulin amyloidosis
Another area where use of high-flux dialysis membranes, and/or use of intermittent on-line hemodiafiltration (IHDF) may be of benefit has to do with complications of beta-2-microglobulin accumulation. Beta-2-microglobulin is a large molecule, with a molecular weight of about 11,600 daltons. This large molecule does not pass at all through low-flux dialysis membranes. Beta-2-M is removed with high-flux dialysis, but is removed even more efficiently with IHDF. After several years have passed (usually at least 5-7), patients on hemodialysis begin to develop complications from the accumulation of beta-2-M, including carpal tunnel syndrome, bone cysts, and accumulation of this amyloid in joints and other tissues. Beta-2-M amyloidosis can cause very serious complications, including a spondylarthropathy, and often is associated with shoulder joint problems. Observational studies from Europe and Japan have suggested a lower incidence of beta-2-M complications when high-flux membranes are used in dialysis mode, or when IHDF is used, as opposed to regular dialysis using a low-flux membrane. [6] [7] [8] [9] [10]
Dialyzer size and efficiency:
Dialyzers come in many different sizes. A larger dialyzer with an increased membrane area (A), will usually remove more solutes than a smaller dialyzer, especially at high blood flow rates. This also depends on the membrane permeability coefficient K0 for the solute in question. So dialyzer efficiency is usually expressed as the K0A - the product of permeability coefficient and area. Most dialyzers have membrane surface areas of 0.8 to 2.2 square meters, and values of K0A ranging from about 500 to 1500 ml/min. K0A, expressed in ml/min can be thought of the maximum clearance of a dialyzer at very high blood and dialysate flow rates.
Reuse of dialyzers
The dialyzer may either be discarded after each treatment or reused. If it is reused, there is an extensive procedure of high-level disinfection. Dialyzers are not shared between patients in the practice of reuse. There was initially controversy about whether reuse of dialyzers resulted in worse patient outcomes. The consensus today is, that dialyzer reuse, done carefully and properly, is associated with similar outcomes to single-use of dialyzers [11].
See also
- Dialysis
- Home hemodialysis
- Peritoneal dialysis
- Hemofiltration
- Extracorporeal therapies
- Renal replacement therapy
- Step-by-step description of hemodialysis
History
For an earlier history of successful and unsuccessful attempts at dialysis, including pioneers such as Abel and Roundtree, Haas, and Necheles, see this review by Kjellstrand [12].
Many have played a role in developing dialysis as a practical treatment for renal failure, starting with Thomas Graham of Glasgow, who first presented the principles of solute transport across a semipermeable membrane in 1854.[13] The artificial kidney was first developed by Abel, Rountree and Turner in 1913,[14], the first hemodialysis in a human being was by Hass (February 28, 1924)[15] and the artificial kidney was develop a into clinically useful apparatus by Kolff in 1943 - 1945.[16] This research showed that life could be prolonged in patients dying of renal failure.
Dr. Willem Kolff was the first to construct a working dialyzer in 1943. The first successfully treated patient was a 67-year-old woman in uremic coma regained consciousness after 11 hours of hemodialysis with Kolff’s dialyzer in 1945. At the time of its creation, Kolff’s goal was to provide life support during recovery from acute renal failure. After World War II ended, Kolff donated the five dialysers he’d made to hospitals around the world, including Mt. Sinai Hospital in New York. Kolff gave a set of blueprints for his hemodialysis machine to George Thorn at the Peter Bent Brigham Hospital in Boston. This led to the manufacture of the next generation of Kolff’s dialyzer, a stainless steel Kolff-Brigham dialysis machine.
By the 1950s, Willem Kolff’s invention of the dialyser was used for acute renal failure, but it was not seen as a viable treatment for patients with end stage renal disease (ESRD). At the time, doctors believed it was impossible for patients to have dialysis indefinitely for two reasons. Firstly, they thought no man-made device could replace the function of kidneys over the long term. In addition, a patient undergoing dialysis suffered from damaged veins and arteries, so that after several treatments, it became difficult to find a vessel to access the patient’s blood.
Dr. Nils Alwall: The original Kolff kidney was not very useful clinically, because it did not allow for removal of excess fluid. Dr. Nils Alwall [17] encased a modified version of this kidney inside a stainless steel canister, to which a negative pressure could be applied, in this way effecting the first truly practical application of hemodialysis, which was done in 1946 at the University of Lund. Alwall also was arguably the inventor of the arteriovenous shunt for dialysis. He reported this first in 1948, where he used such an arteriovenous shunt in rabbits. Subsequently he used such shunts, made of glass, as well as his canister-enclosed dialyzer, to treat 1500 patients in renal failure between 1946 and 1960, as reported to the First International Congress of Nephrology held in Evian in September 1960. Alwall was appointed to a newly-created Chair of Nephrology at the University of Lund in 1957. Subsequently, he collaborated with Swedish businessman Holger Crafoord to found one of the key companies that would manufacture dialysis equipment in the past 40 years, Gambro, Inc. The early history of dialysis has been reviewed by Stanley Shaldon [18].
Dr. Belding H. Scribner working with a surgeon, Dr. Wayne Quinton, modified the glass shunts used by Alwall by making them from Teflon. Another key improvement was to connect them to a short piece of silicone elastomer tubing. This formed the basis of the so-called Scribner shunt, perhaps more properly called the Quinton-Scribner shunt. After treatment, the circulatory access would be kept open by connecting the two tubes outside the body using a small U-shaped Teflon tube, which would shunt the blood from the tube in the artery back to the tube in the vein [19].
In 1962, Scribner started the world’s first outpatient dialysis facility, the Seattle Artificial Kidney Center, later renamed the Northwest Kidney Centers. Immediately the problem arose of who should be given dialysis, since demand far exceeded the capacity of the six dialysis machines at the center. Scribner decided that the decision about who would receive dialysis and who wouldn’t, would not be made by him. Instead, the choices would be made by an anonymous committee, which could be viewed as one of the first bioethics committees.
References
- ↑ FHN Trial Group. Chertow GM, Levin NW, Beck GJ, Depner TA, Eggers PW; et al. (2010). "In-center hemodialysis six times per week versus three times per week". N Engl J Med. 363 (24): 2287–300. doi:10.1056/NEJMoa1001593. PMID 21091062.
- ↑ Fistula First Initiative
- ↑ Eknoyan G, Beck GJ, Cheung AK, Daugirdas JT, Greene T, Kusek JW, Allon M, Bailey J, Delmez JA, Depner TA, Dwyer JT, Levey AS, Levin NW, Milford E, Ornt DB, Rocco MV, Schulman G, Schwab SJ, Teehan BP, Toto R; Hemodialysis (HEMO) Study Group. Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med. 2002 Dec 19;347(25):2010-9. PMID 12490682
- ↑ Cheung AK, Levin NW, Greene T, Agodoa L, Bailey J, Beck G, Clark W, Levey AS, Leypoldt JK, Ornt DB, Rocco MV, Schulman G, Schwab S, Teehan B, Eknoyan G. Effects of high-flux hemodialysis on clinical outcomes: results of the HEMO study. J Am Soc Nephrol. 2003 Dec;14(12):3251-63. PMID 14638924
- ↑ MacLeod AM, Campbell M, Cody JD, Daly C, Donaldson C, Grant A, Khan I, Rabindranath KS, Vale L, Wallace S. Cellulose, modified cellulose and synthetic membranes in the haemodialysis of patients with end-stage renal disease. The Cochrane Database of Systematic Reviews 2007 Issue 1. [1]
- ↑ van Ypersele de Strihou C, Jadoul M, Malghem J, Maldague B, Jamart J. Effect of dialysis membrane and patient's age on signs of dialysis-related amyloidosis. The Working Party on Dialysis Amyloidosis. Kidney Int. 1991 May;39(5):1012-9. PMID 2067196
- ↑ KDOQI Clinical Practice Guidelines for Hemodialysis Adequacy, 2006 Updates. CPR 5. [2]
- ↑ Kuchle C, Fricke H, Held E, Schiffl H. High-flux hemodialysis postpones clinical manifestation of dialysis-related amyloidosis. Am J Nephrol. 1996;16(6):484-8. PMID 8955759
- ↑ Koda Y, Nishi S, Miyazaki S, Haginoshita S, Sakurabayashi T, Suzuki M, Sakai S, Yuasa Y, Hirasawa Y, Nishi T. Switch from conventional to high-flux membrane reduces the risk of carpal tunnel syndrome and mortality of hemodialysis patients. Kidney Int. 1997 Oct;52(4):1096-101. PMID 9328951
- ↑ Locatelli F, Mastrangelo F, Redaelli B, Ronco C, Marcelli D, La Greca G, Orlandini G. Effects of different membranes and dialysis technologies on patient treatment tolerance and nutritional parameters. The Italian Cooperative Dialysis Study Group. Kidney Int. 1996 Oct;50(4):1293-302. PMID 8887291
- ↑ KDOQI Clinical Practice Guidelines for Hemodialysis Adequacy, 2006 Updates. CPR 5. [3]
- ↑ Kjellstrand CM. History of Dialysis, Men and Ideas. Talk given to the Nordic Nephrology Days Symposium, Lund, 1997, as archived on HDCN. [4]
- ↑ http://links.jstor.org/sici?sici=0261-0523(1854)144%3C177%3ATBLOOF%3E2.0.CO%3B2-E Graham T. The Bakerian lecture: on osmotic force. Philosophical Transactions of the Royal Society in London. 1854;144:177–228.
- ↑ http://books.google.com/books?id=KMcCAAAAYAAJ&dq=&pg=PA51&ots=UM7CVprPEW&sig=Xpnf-kEJTYO7iFSxhdSoC2Ujh3Y&prev Abel, J. J., Rountree, L. G., and Turner, B. B. The removal of diffusible substances from the circulating blood by means of dialysis. Tn. Assoc. Am. Phys., 28:51, 1913.
- ↑ http://www.uniklinikum-giessen.de/med3/history/haas/2001-Dial-Transpl.pdf Georg Haas (1886–1971): The Forgotten Hemodialysis Pioneer
- ↑ http://jasn.asnjournals.org/cgi/reprint/8/12/1959 Kolff, W. J., and Berk, H. T. J. Artificial kidney, dialyzer with great area. Geneesk. gids., 21:1944.
- ↑ University of Lund website: Nils Alwall. [5]
- ↑ Shaldon S. Development of Hemodialysis, From Access to Machine (presentation given during a symposium entitled: Excellence in Dialysis: Update in Nephrology; Karachi, Pakistan. October, 2002, as archived on HDCN [6]
- ↑ http://kidney.niddk.nih.gov/about/Research_Updates/win00-01/contrib.htm NIDDK Contributions to Dialysis
External links
- Your Kidneys and How They Work - (American) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), NIH.
- Treatment Methods for Kidney Failure - (American) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), NIH.
- Treatment Methods for Kidney Failure: Hemodialysis - (American) National Kidney and Urologic Diseases Information Clearinghouse, NIH.
- Online Community for Dialysis Patients by Dialysis Patients
- What is dialysis? - Kidney Foundation of Canada.