Dermacentor andersoni
| style="background:#Template:Taxobox colour;"|Dermacentor andersoni | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | ||||||||||||||||||
| style="background:#Template:Taxobox colour;" | Scientific classification | ||||||||||||||||||
| ||||||||||||||||||
| Binomial name | ||||||||||||||||||
| Dermacentor andersoni Stiles, 1908 | ||||||||||||||||||
| File:Dermacentor andersoni range map.svg |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Ilan Dock, B.S.
Overview
Dermacentor andersoni, commonly known as the Rocky Mountain wood tick, is a species of tick well known for its transmission of Rocky Mountain spotted fever, Colorado tick fever, and tularemia.[1]
Life Cycle
General Tick Life Cycle
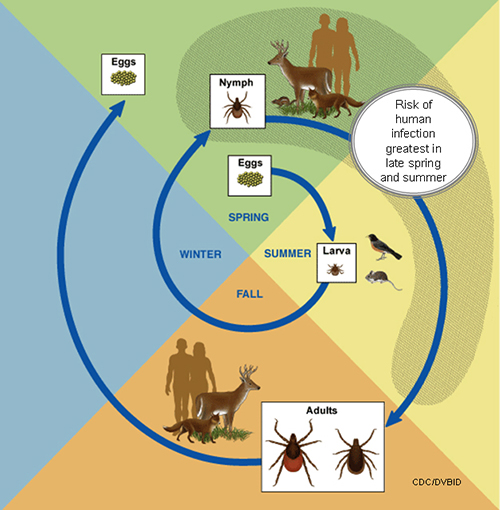
- A tick's life cycle is composed of four stages: hatching (egg), nymph (six legged), nymph (eight legged), and an adult.
- Ticks require blood meals to survive through their life cycle.
- Hosts for tick blood meals include mammals, birds, reptiles, and amphibians. Ticks will most likely transfer between different hosts during the different stages of their life cycle.
- Humans are most often targeted during the nymph and adult stages of the life cycle.
- Life cycle is also dependent on seasonal variation.
- Ticks will go from eggs to larva during the summer months, infecting bird or rodent host during the larval stage.
- Larva will infect the host from the summer until the following spring, at which point they will progress into the nymph stage.
- During the nymph stage, a tick will most likely seek a mammal host (including humans).
- A nymph will remain with the selected host until the following fall at which point it will progress into an adult.
- As an adult, a tick will feed on a mammalian host. However unlike previous stages, ticks will prefer larger mammals over rodents.
- The average tick life cycle requires three years for completion.
- Different species will undergo certain variations within their individual life cycles. [2]
Spread of Tick-borne Disease
- Ticks require blood meals in order to progress through their life cycles.
- The average tick requires 10 minutes to 2 hours when preparing a blood meal.
- Once feeding, releases anesthetic properties into its host, via its saliva.
- A feeding tube enters the host followed by an adhesive-like substance, attaching the tick to the host during the blood meal.
- A tick will feed for several days, feeding on the host blood and ingesting the host's pathogens.
- Once feeding is completed, the tick will seek a new host and transfer any pathogens during the next feeding process. [2]
Key features
- The larva only has three pairs of legs.
- The nymph has four pairs.
- A single pair of spiracular openings (stigmata) are seen close to the coxae (leg bases or segments) of the fourth pair of legs (except in larvae).
- A terminal capitulum (mouthparts) is visible from above in all hatched stages.
- A large sclerite called the scutum is present dorsally behind the capitulum. The scutum almost entirely covers the back of the male, but only partly covers the back of the female.
- Eyes, if present, are on the scutum.
- Sexual dimorphism in size and colour is frequent. The female is often larger.
- The posterior margin of opisthosoma is usually subdivided into sclerites called festoons.
- The pedipalps are rigid along the chelicerae, and are not leg-like.
Dermacentor andersoni Transmitted Diseases
Tick-borne diseases transmitted by the Rocky Mountain wood tick include, Rocky Mountain spotted fever (RMSF), Colorado tick fever, and Tularemia.
|
Transmitted Diseases ▸ RMSF ▸ Colorado tick fever ▸ Tularemia |
|
Geographic Distribution
- Rocky Mountain states
- Southwestern Canada 4,000 to 10,500 feet

Prevention
Limiting tick exposure

It is unreasonable to assume that a person can completely eliminate activities that may result in tick exposure. Therefore, prevention measures should emphasize personal protection when exposed to natural areas where ticks are present:
- Wear light-colored clothing which allows you to see ticks that are crawling on your clothing.
- Tuck your pants legs into your socks so that ticks cannot crawl up the inside of your pants legs.
- Apply repellents to discourage tick attachment. Repellents containing permethrin can be sprayed on boots and clothing, and will last for several days. Repellents containing DEET (n, n-diethyl-m-toluamide) can be applied to the skin, but will last only a few hours before reapplication is necessary. Use DEET with caution on children. Application of large amounts of DEET on children has been associated with adverse reactions.
- Conduct a body check upon return from potentially tick-infested areas by searching your entire body for ticks. Use a hand-held or full-length mirror to view all parts of your body. Remove any tick you find on your body.
- Parents should check their children for ticks, especially in the hair, when returning from potentially tick-infested areas.
- Ticks may also be carried into the household on clothing and pets and only attach later, so both should be examined carefully to exclude ticks.[4]
The best way to remove a tick
- Use fine-tipped tweezers or notched tick extractor, and protect your fingers with a tissue, paper towel, or latex gloves. Persons should avoid removing ticks with bare hands.
- Grasp the tick as close to the skin surface as possible and pull upward with steady, even pressure. Do not twist or jerk the tick; this may cause the mouth-parts to break off and remain in the skin. (If this happens, remove mouth-parts with tweezers. Consult your health care provider if illness occurs.)
- After removing the tick, thoroughly disinfect the bite site and wash your hands with soap and water.
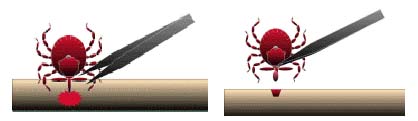
- Do not squeeze, crush, or puncture the body of the tick because its fluids may contain infectious organisms. Skin accidentally exposed to tick fluids can be disinfected with iodine scrub, rubbing alcohol, or water containing detergents.

- Save the tick for identification in case you become ill. This may help your doctor to make an accurate diagnosis. Place the tick in a sealable plastic bag and put it in your freezer. Write the date of the bite on a piece of paper with a pencil and place it in the bag. [5]
References
- ↑ Dergousoff SJ, Gajadhar AJ, Chilton NB (March 2009). "Prevalence of Rickettsia species in Canadian populations of Dermacentor andersoni and D. variabilis". Appl. Environ. Microbiol. 75 (6): 1786–9. doi:10.1128/AEM.02554-08. PMC 2655481. PMID 19151178.
- ↑ 2.0 2.1 Life Cycle of Ticks that Bite Humans (2015). http://www.cdc.gov/ticks/life_cycle_and_hosts.html Accessed on December 30, 2015
- ↑ Rocky Mountain Spotted Fever Information. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/rmsf/ Accessed on December 30, 2015
- ↑ General Tick Disease Information. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/ticks/symptoms.html Accessed on December 30, 2015
- ↑ Tick Removal. Centers for Disease Control and Prevention (2015). http://www.cdc.gov/ticks/removing_a_tick.html Accessed on December 30, 2015
Gallery
- Common name: Rocky Mountain wood tick
- Scientific name: Dermacentor andersoni
- Reservoir: small rodents (larvae and nymphs); large mammals (adult ticks)
- Geographic distribution: Rocky Mountain states
- Disease transmitted: Rocky Mountain spotted fever, tularemia
-
Rocky Mountain wood tick (Dermacentor andersoni)
Adapted from CDC -
Approximate distribution of the Rocky Mountain Wood tick
Adapted from CDC