Radial catheterization hemostasis
Jump to navigation
Jump to search
|
Radial artery cathetarization Microchapters |
|
Case Studies |
|---|
|
Radial catheterization hemostasis On the Web |
|
American Roentgen Ray Society Images of Radial catheterization hemostasis |
|
Directions to Hospitals Treating Radial artery cathetarization |
|
Risk calculators and risk factors for Radial catheterization hemostasis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Achieving hemostasis after Radial Artery Catheterization
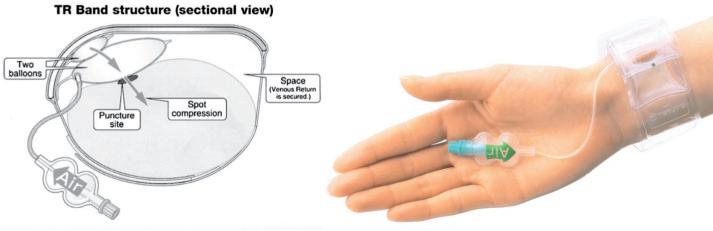
Instructions for the use of the TR Band
- Radial arterial sheath removal after cardiac catheterization or PCI, or peripheral angiography with or without intervention will be performed by trained personnel
- Radial sheaths placed by cardiologists must be removed by a trained or supervised Cardiology Fellow or attending. Radial sheaths placed by a vascular surgeon must be removed by a Vascular surgery attending, fellow, PA, NP or trained surgical resident as designated by vascular MD’s.
- Radial artery sheaths will be removed in the Cardiac Catheterization Laboratory prior to transfer to a medical surgical inpatient unit. A radial artery sheath may be removed in the ICU or VICU setting.
- This device is placed on the hyper extended wrist and tightened via a Velcro band.
- A small green box indicates where the band should be placed proximal to the radial percutaneous site. Single wall stick; place the green dot on the TR Band about 3-4 mm proximal to the skin insertion site. Double wall stick; place the green dot just 1 mm or two proximal to the skin insertion site
- The TR Band inflator syringe is filled with 18 cc of air and slowly injected into the one-way side port which inflates the balloon overlying the radial artery.
- Concomitantly, the radial sheath is slowly pulled out completely, as the balloon is inflated to the maximum of 18 cc of air.
- Then slowly, withdraw air back out via the syringe, 1cc at a time, until the operator observes for blood leaking out from the puncture site, at which time, 1 cc of air is re-injected into the balloon and the syringe is disconnected.
- Keep the plunger in place with your thumb when inflating/deflating the TR band. Releasing the plunger will cause air to expel out of the band to quickly
- Remember to keep the syringe for later deflation
Application tips to remember:
- Make sure the radial artery insertion site is 3 or more cm proximal to the wrist crease. If the site and thus the band are too close to the wrist, it may slip if the wrist bends
- Make sure the site is cleaned with sterile saline and dried completely before the band is placed on the wrist
- Place the green box proximal to the sheath insertion site(Terumo logo closest to the patients little finger)
- Pulling the sheath slowly as you are simultaneously inflating the TR Band to 18 cc’s. You should be completely removing the sheath at about the same time you hit 18cc’s.
- Once all 18cc’s are in the band and the sheath is removed, you slowly about 1cc per second begin reducing the amount of air in the band while visualizing the access site for a blood flash
- Once you visualize a blood flash you immediately put 1 to 2cc’s back into the band and disconnect the syringe confirming that the blood has ceased.
- If the air is released slowly out of the band, there is no need for gauze to be positioned under the TR Band. If you are removing the air slowly and at first sight of a blood flash 1 to 2 cc’s is put back into the band you will have a dry field. You want to have complete visualization of the access site, you do not want a gauze pad to block your visualization of the arteriotomy.
- Also, there is no need to make a skin nick when introducing the sheath (unless completely necessary). The Glidesheath is hydrophilic coated and has a near seamless transition and will not require a nick for insertion. The TR Band is designed to provide the least amount of pressure to gain hemostasis while maintaining flow through both the radial and ulnar arteries. The TR Band is not designed to provide hemostasis for both the arteriotomy of the access site as well as a large skin nick. That is why with the design of both these products a skin nick is not needed and you should never experience a situation in which you would need more than 18cc’s of air, which is occlusive pressure.
TR-Band used to achieve radial artery hemostasis